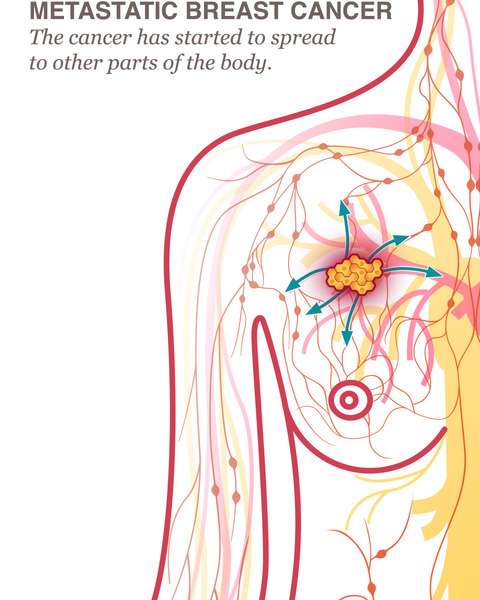
Where Can Breast Cancer Spread
The most common places for breast cancer to spread to are the lymph nodes, bone, liver, lungs and brain. The symptoms you may experience will depend on where in the body the cancer has spread to. You might not have all of the symptoms mentioned here.
Remember other conditions can cause these symptoms. They dont necessarily mean that you have cancer that has spread. But if you have symptoms that you are worried about, discuss them with your GP, cancer specialist, or breast care nurse so that you can be checked.
Symptoms If Cancer Has Spread To The Bones
You may have any of these symptoms if your cancer has spread to the bones:
- an ache or pain in the affected bone
- breaks in the bones because they are weaker
- breathlessness, looking pale, bruising and bleeding due to low levels of blood cells – blood cells are made in the bone marrow and can be crowded out by the cancer cells
Sometimes when bones are damaged by advanced cancer, the bones release calcium into the blood. This is called hypercalcaemia and can cause various symptoms such as:
Diagnosing Metastatic Breast Cancer
Getting a clear picture of where breast cancer has spread is essential for creating a personalized treatment plan. Your care team will likely use a combination of the following tests and tools to diagnose both localized and advanced breast cancer:
Ultrasound exam: With this imaging technique, sound waves create a picture of internal areas of the body.
Magnetic resonance imaging : This procedure produces detailed images using magnetic fields and radio waves.
Blood chemistry studies: A blood sample is taken to measure the amounts of certain substances that are released by your organs and tissues. A higher or lower amount of a particular substance may be a sign of disease.
Biopsy: A biopsy is the removal of cells or tissues so a pathologist may view them through a microscope. Your original breast cancer diagnosis was likely confirmed with a biopsy.
You May Like: What Is The Prognosis For Stage 4 Breast Cancer
Recommended Reading: How Long Can You Have Breast Cancer
Where Does Breast Cancer Spread To
Breast cancer cells seem to prefer to settle into:-
- long bones in the arms and legs
With an osteolytic metastasis, the cancer kind of eats away at the bone, creating holes.
With an osteoblastic bone metastasis, the bone mineral density actually increases, but this can cause the bones to fracture more easily. This requires a little more explanation. Breast cancer metastases tend to be lytic when they are untreated, and then they become densely sclerotic as they respond to treatment.
Even if no treatment is given yet, an osteoblastic metastasis from breast cancer generally indicates that the persons own body is trying to fight cancer with some success.
A CT scan may also be used to check for metastasis to the lungs or liver. A CT scan is essentially an X-ray linked to a computer. The breast cancer doctor injects a contrast dye agent into the bloodstream and this makes any cancer cells in the liver and chest easier to see.
What Is Early Stage Breast Cancer
If youâre diagnosed with early stage breast cancer, find out what to expect and what treatment options are available.
Stage III is locally advanced cancer. It is divided into Stage IIIA, IIIB, and IIIC.
Stage IIIA
Stage IIIA is one of the following:
- The tumor is no more than 5 centimeters across. The cancer has spread to underarm lymph nodes that are attached to each other or to other structures. Or the cancer may have spread to lymph nodes behind the breastbone.
- The tumor is more than 5 centimeters across. The cancer has spread to underarm lymph nodes that are either alone or attached to each other or to other structures. Or the cancer may have spread to lymph nodes behind the breastbone.
T0, T1, T2, or T3 N2 M0 or if the tumor is more than 50mm and has spread to 1-2 axillary lymph nodes â T3, N1, M0
Stage IIIB
Stage IIIB is a tumor of any size that has grown into the chest wall or the skin of the breast. It may be associated with swelling of the breast or with nodules in the breast skin:
T4 N0, N1, or N2 M0
Stage IIIC
Stage IIIC is a tumor of any size. It has spread in one of the following ways:
- The cancer has spread to the lymph nodes behind the breastbone and under the arm.
- The cancer has spread to the lymph nodes above or below the collarbone.
Any T, N3, M0
Recommended Reading: Does Hormone Therapy For Breast Cancer Cause Weight Gain
How Is A Local Recurrence After Lumpectomy Diagnosed
After a diagnosis of early stage breast cancer, any remaining breast tissue should be evaluated annually with scans .
Most local recurrences within the breast after lumpectomy are detected on routine annual breast imaging, which usually takes the form of mammography and ultrasound, and on occasions MRI.
If you have a local recurrence or new primary breast cancer, you may find symptoms similar to an initial breast cancer. This includes:
- A new lump in the breast, armpit area or around the collarbone
- A change in breast size or shape
- Changes to the nipple, such as sores or crusting, an ulcer or inverted nipple
- Clear or bloody nipple discharge
- Changes to the skin including redness, puckering or dimpling
- Breast tenderness or pain
Once a local recurrence has been diagnosed, we do tests to see whether there are signs of cancer elsewhere in the body. These may include a chest X-ray, CT scan, bone scan or PET scan, and blood tests , then we have to figure out how best to treat the tumour in the breast. Usually in these cases we do a mastectomy, as the prior less drastic surgery and radiation didnt take care of it.
Biopsy Of An Enlarged Lymph Node
If any of the lymph nodes under the arm or around the collarbone are swollen, they may be checked for cancer with a needle biopsy, either a fine needle aspiration or a core needle biopsy. Less often, the enlarged node is removed with surgery. If cancer is found in the lymph node, more nodes will need to be removed .
Don’t Miss: Where To Buy Breast Cancer Merchandise
Looking For More Of An Introduction
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
-
ASCO AnswersFact Sheet: Read a 1-page fact sheet that offers an introduction to metastatic breast cancer. This free fact sheet is available as a PDF, so it is easy to print.
-
ASCO AnswersGuide:Get this free 52-page booklet that helps you better understand breast cancer and its treatment options. The booklet is available as a PDF, so it is easy to print.
Limited Arm And Shoulder Movement
You might also have limited movement in your arm and shoulder after surgery. This is more common after ALND than SLNB. Your doctor may advise exercises to help keep you from having long-lasting problems .
Some women notice a rope-like structure that begins under the arm and can extend down toward the elbow. This is sometimes called axillary web syndrome or lymphatic cording. It is more common after ALND than SLNB. Symptoms may not appear for weeks or even months after surgery. It can cause pain and limit movement of the arm and shoulder. This often goes away without treatment, although some women may find physical therapy helpful.
Also Check: Melatonin And Estrogen Positive Breast Cancer
Sentinel Lymph Node Biopsy
In a sentinel lymph node biopsy , the surgeon finds and removes the first lymph node to which acancer is likely to spread . A radioactive substance and/or a blue dye is injected into the tumor, the area around it, or the area around the nipple. Lymph vessels will carry these substances along the same path that the cancer would likely take. The first lymph node the dye or radioactive substance travels to will be the sentinel node.
After the substance has been injected, the sentinel node can be found either by using a special machine to detect radioactivity in the nodes, or by looking for nodes that have turned blue. Sometimes, both methods are used. The surgeon cuts the skin over the lymph node area and removes the node containing the dye or radioactivity.
The few removed lymph nodes are then checked closely in the lab for cancer cells by a pathologist. Sometimes, this is done during the surgery. Because there is a chance that other lymph nodes in the same area will also have cancer if cancer is found in the sentinel lymph node, the surgeon may go ahead with an axillary dissection to remove more lymph nodes while you are still on the operating table. If no cancer cells are seen in the node at the time of the surgery, or if they are not checked by a pathologist at the time of the surgery, they will be examined more closely over the next several days.
Based on the studies that have looked at this, skipping the ALND may be an option for:
Diagnosing Secondary Cancer In The Lymph Nodes
Secondary cancer in the lymph nodes may be diagnosed at the same time as the primary cancer. It may also be found during routine tests and scans after treatment.
If a lymph node close to the surface of the skin is affected, your doctor may be able to see it or feel it. If an affected lymph node is deep inside the chest, tummy or pelvis, only a scan can find it.
If you have had cancer before, you may only need a scan to make a diagnosis of secondary cancer in the lymph nodes. This may be:
- A CT scan
A CT scan takes a series of x-rays, which build up a 3D picture of the inside of the body.
- An MRI scan
An MRI scan uses magnetism to build up a detailed picture of the inside of your body.
- An ultrasound scan
Recommended Reading: Can You Get Breast Cancer In Your 20s
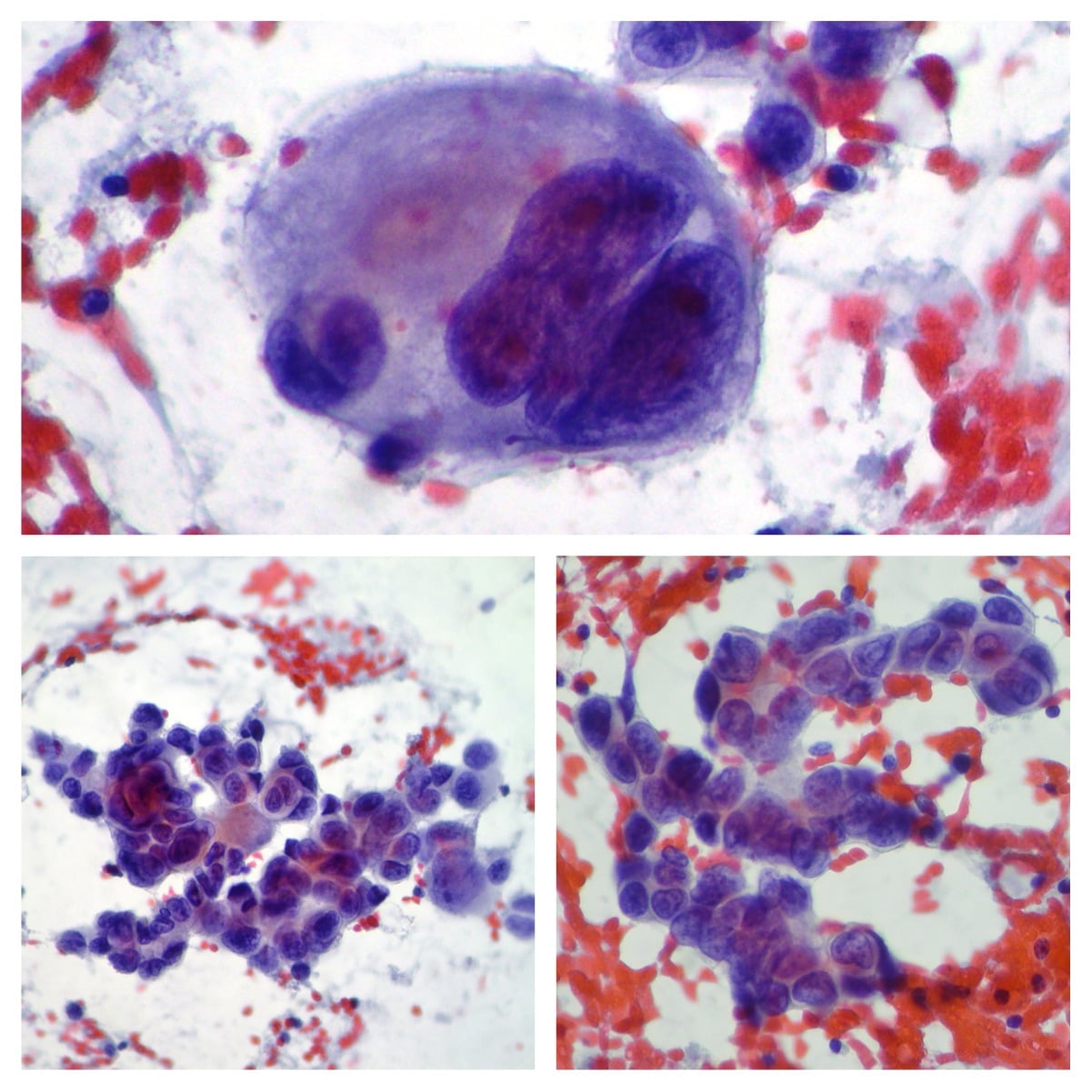
Identification Of Tumor Cells In Lymph Nodes By Mass Cytometry
Our material consisted of lymph nodes from 52 patients with primary operable nonmetastatic breast cancer . For simultaneous profiling of tumor and immune cells, we established a 37parameter antibody panel with markers for identification and subtyping of tumor cells, immune cell phenotypes, and functional assessment . The panel identified both tumor cells and a diversity of immune cell populations as expected . Eleven cases had sufficient number of metastatic tumor cells for further analysis, and the expression patterns of ER, PgR, and HER2 in the metastatic tumor cells reflected the pathology assessment of the corresponding primary tumors . Hierarchical clustering and viSNE analysis of mass cytometry data revealed intertumoral heterogeneity in the expression of stem cell markers CD44 and CD24 across the 11 samples, whereas PDL1/PDL2 expression was low/undetectable in all cases . The viSNE analysis further showed limited intratumoral variation . These results could be biased due to low numbers of tumor cells per sample analyzed or might reflect that only specific subpopulations of the primary tumor are capable of metastasizing, resulting in lower heterogeneity of metastasizing tumor cells .
Mechanisms Of Breast Cancer Metastasis
No one really knows what factors will make a certain patient more or less susceptible to breast cancer metastasis.
There is growing awareness that part of that susceptibility is due to host factors. The host factors are the characteristics of the non-malignant cells and the general biological environment surrounding the malignant breast tumor.
Sometimes the host factors are referred to as the pre-metastatic niche and it is thought that bone-marrow-derived progenitor cells may directly influence the dissemination of malignant cells to distant areas.
Non-neoplastichost cells within the tumor may also play a key role in the regulation of breast cancer metastasis.
You May Like: Can Iodine Cure Breast Cancer
When To Contact A Doctor
If a person notices any signs of cancer having spread to their lymph nodes, they should speak with a doctor immediately.
Additionally, if a person with cancer notices any unusual new symptoms, they should contact a doctor. The sooner a person receives treatment for cancer that has spread, the better their chances of survival.
If Your Breast Cancer Has Spread
Even if your breast cancer has spread to other parts of your body, it does not necessarily mean its not treatable. If the cancer cannot be removed, the goal of treatment is to improve symptoms, improve quality of life and extend survival.
Some women live with breast cancer for several years as they learn to adjust and accept that theyll be on treatment for an indefinite period of time, explains Dr. Roesch. Your cancer team will help you learn and cope with what you can expect on this journey.
Also Check: Baking Soda And Breast Cancer
Also Check: What Do Breast Cancer Look Like
What Is Stage Ii Breast Cancer
Stage II describes cancer that is in a limited region of the breast but has grown larger. It reflects how many lymph nodes may contain cancer cells. This stage is divided into two subcategories.
Stage IIA is based on one of the following:
- Either there is no tumor in the breast or there is a breast tumor up to 20 millimeters , plus cancer has spread to the lymph nodes under the arm.
- A tumor of 20 to 50 millimeters is present in the breast, but cancer has not spread to the lymph nodes.
Stage IIB is based on one of these criteria:
- A tumor of 20 to 50 millimeters is present in the breast, along with cancer that has spread to between one and three nearby lymph nodes.
- A tumor in the breast is larger than 50 millimeters, but cancer has not spread to any lymph nodes.
Emma D Wrenn And Kevin J Cheung
A large number of tumor cells reaching distant sites will die and never grow into a clinically detectable metastasis . Disseminated tumor cells encounter inhospitable stromal matrices, cell types, and paracrine signals different from their organ of origin. In addition, they are actively eliminated by immune cells, such as natural killer and T-cells. Diverse mechanisms have been described that enable tumor cells to overcome these barriers: entry into a stem cell-like state, epithelial-to-mesenchymal and mesenchymal-to-epithelial transitions, genetic mutation, and co-option of the native microenvironment for example . Here, we focus on an emerging mechanism by which cancer cells increase their chance of successmetastasizing as cohesive clusters of cells, also known as collective metastasis.
Fig. 2
Clusters resist programmed cell death. Tumor cell clusters have increased survival at metastatic sites through several mechanisms including depletion of reactive oxygen species, resistance to NK cell killing, and pro-survival signals transduced downstream of cellcell adhesion
Read Also: Is There Stage 0 Breast Cancer
Treatment For Cam And Prognosis
There were 2 patients who refused any treatment after CAM. Of the remaining cases, 52 patients received chemotherapy, 8 patients received anti-HER2 therapy, 6 patients received contralateral axillary radiotherapy, and 16 patients received endocrine therapy. A total of 20 patients underwent contralateral axillary lymph node dissection or low-middle level ALND, and 3 patients underwent surgical castration. Detailed information on the pathological results of lymph nodes at different levels was queried in 12 patients . Contralateral mastectomy was performed in 5 patients, and no tumor was found in the gland.
Table 3 Metastatic status of contralateral axillary lymph nodes.
The prognosis of isolated CAM patients was better than that of patients with other distant metastases in terms of CAM-OS and PFS with significant differences and OS without significant differences .
Figure 2 Survival curves of CAM patients with or without other distant metastases. CAM-OS of CAM patients with or without other distant metastases. PFS of CAM patients with or without other distant metastases. OS of CAM patients with or without other distant metastases.
For the isolated CAM patients, 22 patients developed tumor progression after CAM treatment with a mean PFS of 34.4 months, and 18 patients survived during the follow-up. The five-year survival rate of isolated CAM patients was 67.4%, and the five-year disease-free survival rate was 52.9%.
The Extrinsic Effect Of Targeted Therapy
Fig. 4: The effects of cell-extrinsic and cell-intrinsic determinants in dictating breast cancer outcomes.
Part I The journey of a breast cancer patient from the development of undetectable disease and its clinical discovery , through its surgical removal and adjuvant ET , to metastatic relapse and death . The presence of tumour lesions across the body is indicated by starsthe smaller referring to the clinically undetectable ones , the bigger ones to the clinically detectable ones . Part II The development of an HR+ breast tumour lesion in the breast , comprising a mixture of ER+/PR+ and ER/PR cells . DTC escape from the primary site can occur early and/or late during tumorigenesis , although the HR phenotype of DTCs at these stages is often unclear. Bones, lungs and liver are represented as common secondary sites for breast cancer metastases, albeit the sequential patterns of DTC spread among these organs are still elusive . Targeted treatment for HR+ breast cancer patients relies on adjuvant ET. Several mechanisms of ET resistance cytostasis, ESR1 mutations and HR function regulationcontribute to DTC outgrowth. DTC disseminated tumour cell, ER oestrogen receptor, ET endocrine therapy, HR hormone receptor, PR progesterone receptor. Figure created with BioRender.com.
Recommended Reading: What Stages Of Breast Cancer Are There
Contralateral Axillary Lymph Node Metastases At The Time Of Primary Breast Cancer Diagnosis: Curative Or Palliative Intent
C. Zhou
1Department of Surgery, Medical Center Alkmaar, Alkmaar, The Netherlands
2Department of Radiation Oncology, Medical Center Alkmaar, Alkmaar, The Netherlands
Academic Editor:
Abstract
Contralateral axillary lymph node metastases in breast cancer patients are uncommon. CAM can be found at the time of primary breast cancer diagnosis or following prior treatment of breast cancer as a recurrence. This distinction may have important implications for disease staging and treatment selection. We report the case of a premenopausal woman with synchronous CAM. Despite extensive multimodality treatment, a recurrence was found 27 months after primary surgery. We reviewed the literature on histopathological tumor characteristics associated with CAM, lymphatic drainage of the breast to other sites than the ipsilateral axilla, and outcome of cases with CAM. This case contradicts current conceptions that CAM only develops from tumors with poor histopathological features. Emerging evidence shows that altered lymphatics play a central role in development of synchronous CAM. It is precisely this etiology that supports the concept that synchronous CAM occurs by lymphatic spread and not by hematogenous spread. Although controversial, treatment of synchronous CAM should therefore be of curative intent.
1. Background
Recommended Reading: Stage 2 Breast Cancer