Why Werent These Escaping Cells Identified The First Time The Cancer Was Treated
Although scans of the body can detect if there is obvious spread to these other organs, for women with early stage breast cancer there rarely is anything that shows up on a scan. There is a limit to what scans can tell us: they wont show extremely tiny spots of cancer, and they definitely cant show us if there are individual cells circulating in the body. Neither will any blood test, or any other test for that matter. So the first time around we perform our surgery and give our treatmentschemotherapy, hormonal therapy, radiationwith the hope that if microscopic spread has already taken place, the treatments will scavenge those cells and kill them before they take up residence someplace in the body.
Unfortunately, these treatments dont work 100 percent of the time. So if cells have spread, and if the treatments we give dont affect them, the cancer cells can persist and take hold someplace, developing into metastases, or spread. This is why and how recurrence happens.
Annual Recurrence Pattern According To Our Single
Figure 1C shows the smoothed ARR curves of breast cancer after mastectomy and lumpectomy. The ARR curve after mastectomy displayed a double-peaked pattern, with the major high peak at 2 years and a low flat peak at 5 years . In contrast, the ARR curve after lumpectomy exhibited one peak near 56 years . The first recurrence surge observed after mastectomy was not obvious after lumpectomy. In order to confirm the influence of menopausal status on recurrence timing and pattern, we performed an additional subgroup analysis according to menopausal status in women who underwent lumpectomy. The result shows that there was a difference in recurrence timing between premenopausal and postmenopausal women who underwent lumpectomy. However, the timing difference is only about 1 year, which indicates that our observation of an obvious difference in recurrence timing between lumpectomy and mastectomy is not a result of the higher proportion of premenopausal women in the lumpectomy group.
Risk Factors For Developing Locoregional Recurrence
Over the last decade, tumor biology has emerged as one of the most powerful determinants of locoregional recurrence. The incidence of IBTRs and chest wall or regional node recurrences varies based on the stage of disease at presentation and adjuvant treatments. Young age, nodal positivity, larger tumors, and hormone receptornegative tumors have been associated with a higher risk of recurrence. However, this rate has been dropping. Tumor biology impacts the interval to ILRR the median time to ILRR is longer for estrogen receptor -positive vs ER-negative cancers. Triple-negative breast cancers have a higher early local failure rate compared with ER-positive cancers, with a 5-year cumulative incidence of 4.2% and 5.4% for lumpectomy and mastectomy, respectively. Notably, ILRR events among patients with ER-positive cancers continue over a 20-year period.
The molecular profiling of tumors has shed further light on the biological behavior of breast cancer, including the risk of locoregional recurrence. A high Oncotype DX Recurrence Score, indicative of a patients risk for distant metastases in ER-positive carcinomas, is also associated with a higher risk of locoregional recurrence.
Lumpectomy margins and radiotherapy
Nodal involvement
Systemic therapy
Don’t Miss: Can You Die From Stage 0 Breast Cancer
Family History Genetic Test For Gene Mutations
The researchers asked study participants about the type of treatment they had, as well as the clinical indications for double mastectomy, including the patients family history of breast and ovarian cancer, and the results of any genetic testing.
Women with a family history of breast or ovarian cancer, or with a positive genetic test for mutations in the BRCA1 or BRCA2 genes, may be advised to consider having both breasts removed, because they are at high risk of a new cancer developing in the other breast. This represents about 10 percent of all women diagnosed with breast cancer. Women without these indications are very unlikely to develop a second cancer in the healthy breast, according to the researchers.
Dont Miss: Can You Get Breast Cancer At 16
Should I Have Regular Routine Scans Or Blood Tests To Check For Distant Breast Cancer Recurrence
No. Routine scans to check for the presence of distant disease recurrence are not recommended in the absence of symptoms
Given the ominous nature of stage 4 disease, the obvious question is, why dont we scan for spread regularly after a first diagnosis, so that we can detect it early if it does return? The reason we dont scan or test for metastasis is that there really is no early stage 4 disease, and thus no real opportunity to intervene earlier and increase the chance of cure. Its also important to know that with recurrence, one does not progress from one stage to the next: a woman who was originally diagnosed with stage 1 breast cancer does not recur as stage 2, because once cells have taken up residence elsewhere, she is immediately considered to have stage 4 disease. And with stage 4 disease, either you respond well to treatment and the disease regresses, or you dont and it doesnt. Studies have shown that getting frequent scans after a first cancer diagnosis does not lead to improved survival, which is why we dont scan for stage 4even if we wish we could.
Current guidelines and evidence therefore recommend against routine CT or bone scans, or blood tests, to look for recurrence of cancer in patients who do not have any symptoms or other concerns that need to be followed up on.
If you do have concerning symptoms , then you should bring them to the attention of your healthcare team to be checked out.
Read Also: What Is The Survival Rate Of Her2 Positive Breast Cancer
What Are The Signs Of Breast Cancer Recurrence
Breast cancer can return to the original site or it can return and spread to other areas of the body, which is called distant recurrence or metastasis. Local recurrence is generally discovered during routine mammograms or when the patient notices a physical change. Most often, women experience symptoms such as weight loss, bone pain, or shortness of breath. There can often be nodules on or under the skin of the chest wall, or a new area of thickening near the scar left from the mastectomy. If the cancer recurrence in the regional area, such as the lymph nodes, you may notice swelling or a lump under your arm, in your neck, or near the collarbone.
Depending on what the symptoms are, your doctor may want to do a tissue biopsy, blood tests such as a tumor marker, or other imaging tests like a CT scan or bone scan. If the cancer is determined to be metastatic breast cancer, this means that it has spread to other areas such as the lungs, bones, or brain. Its still called breast cancer, even though it has spread.
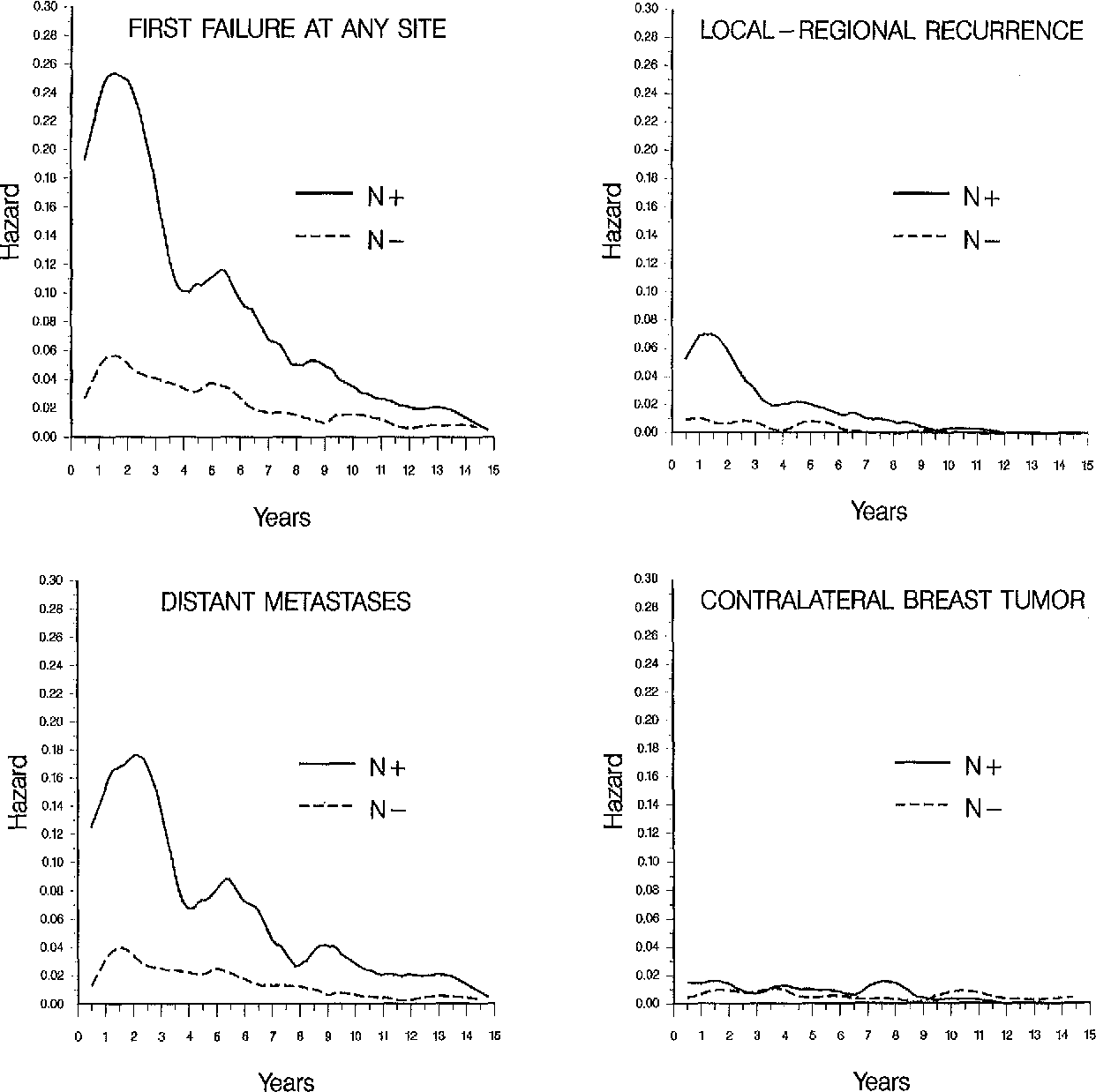
Hr By Tumor Histologic Grade And Disease Stage
Women with different tumor grades showed even more dynamic changes in the annual HR for the first recurrence over the 10 years of follow-up . Women with poorly differentiated histology had a higher annual HR of recurrence in the first 5 years than the women with other grades after primary treatment . The dynamic differences in hazard by histologic grade became more dynamic among women with advanced AJCC stage . Unlike women with stage I disease, women with stage III disease and with a well-differentiated grade showed several peaks of hazard within the 10 years of follow-up women with unknown grades also had a second peak around 6 years and a third sharp peak after 9 years.
However, it should be noted that the pathologic specimen may not always capture the dominant component of the tumor grade within entire tumor lesion. Therefore, the category of tumor with unknown grade might also consist of a mixture of grades such as well-to-moderately differentiated or poorly differentiated histopathology within the same tumor.
Recommended Reading: How To Survive Triple Negative Breast Cancer
Talking To Family And Friends About Your Illness
Women who have breast cancer are often concerned about how the disease will affect their relationship with their partner and if they are mothers their children. The stress of treatment often makes sexual needs a lower priority for a while. It can affect your daily routine and require a lot of decisions and planning. All this can give rise to conflicts. Its important to keep talking to your partner. If you have reached your limits you can get psychological counseling or support, either individually, or as a couple.
Whether children are still very young or already grown up, many mothers find it difficult to talk to their children or grandchildren about their disease. It might stir up memories of the first time they were diagnosed and the same fears may resurface, along with new worries as well. But even if you would rather protect your children from this situation, children do sense when something is wrong. So it is a good idea to speak openly with them about the cancer coming back and about the fact that there may be more treatment to come, and that you may once again need to rest more often.
What Types Of Breast Cancer Have The Highest Recurrence Rates
A study published in the Journal of Clinical Oncology found the risk of recurrence for all breast cancers was highest in the first five years from the initial cancer diagnosis at 10.4%. This was highest between the first and second years after the initial diagnosis. During the first five years after the initial diagnosis, patients with oestrogen receptor positive breast cancer had lower rates of recurrence compared with those with ER negative disease. However, beyond five years, patients with ER positive disease had higher rates of recurrence.
Also Check: What To Say To Someone Just Diagnosed With Breast Cancer
Breast Cancer Recurrence After Mastectomy And Reconstruction
In many cases, women experience breast cancer recurrence, especially after mastectomy and reconstruction surgery. In addition, its not uncommon for breast cancer to spread to the second one in one breast.
Learn more about how it can happen and what you should do if it recurs in your other breast.
We want to talk with you about the possible treatment options if your tumor metastasizes or reappears in your other breast after a mastectomy and reconstruction surgery. The two main treatments we talk about are mastectomy and reconstruction.
In some cases, it happens that breast cancer returns. Even after mastectomy and reconstruction surgery, there are still minimal chances of cancer recurrence. But if it does occur, you could need to think about the best treatment options available.
What Is My Prognosis
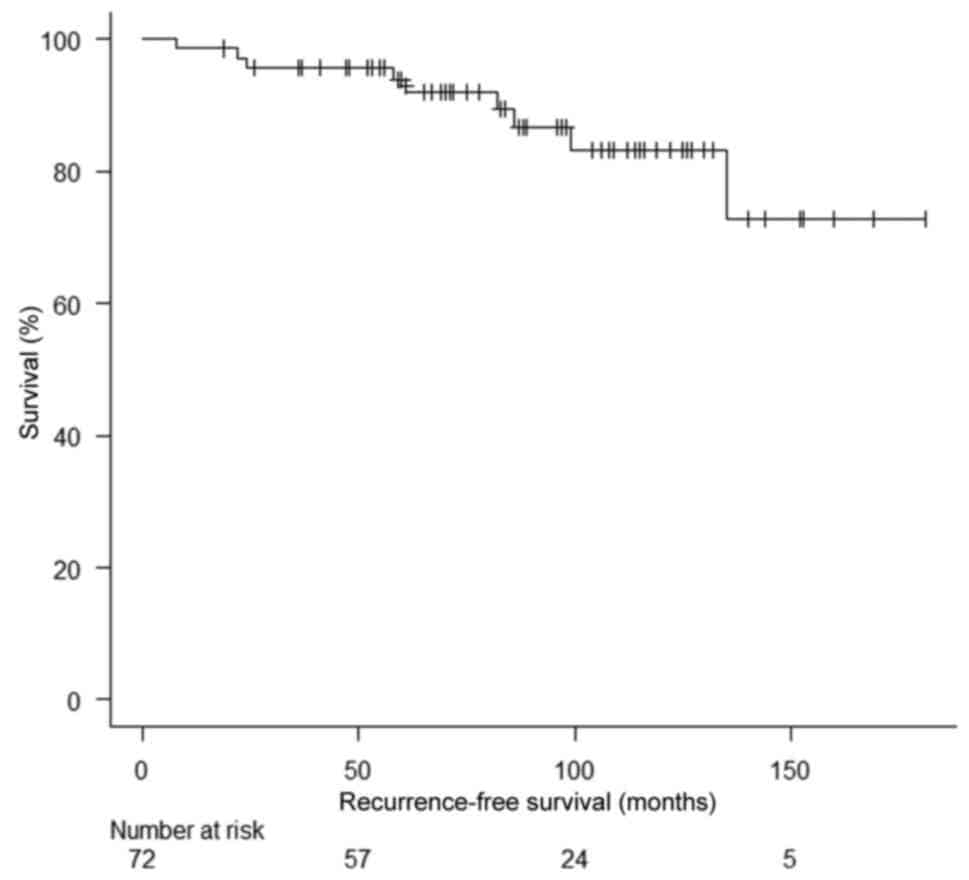
This is a very common question that isnt always easy to answer. There are many factors involved in working out prognosis. Remember that a prognosis is just a figure at the point at which you receive it. For most people, the prognosis gets better with time.
Sometimes we use a five-year figure because we know that if cancer comes back, most of the time it comes back within five years. If the cancer has not come back within five years, then the chance of it coming back within ten years is quite low, and if it does not come back within ten years, then you have an almost normal life expectancy.
Its a bit like buying a second hand car. You dont really know how long its going to last, but if it lasts year after year without breaking down, then the car starts to look more and more reliable to make that long trip.
Working out prognosis can be difficult.
Recommended Reading: Can Young Women Get Breast Cancer
Is A Mastectomy My Only Option For Preventing Breast Cancer
Getting a tumor in your breast does not necessarily mean you will have toremove your breast entirely. Many cases of breast cancer can be treated byremoving the tumor itself and some of the surrounding tissue. Treatment mayalso include chemotherapy, radiation or hormone therapy. Treatments forbreast cancer are continually evolving, offering patients greater choicesand improved outcomes. Surgeons with the Johns Hopkins Breast Center are onthe front lines of developing and performing the most innovative oncologicprocedures. Talk to your surgical oncologist about your treatment options.
Factors That Affect The Risk Of Breast Cancer Recurrence Following A Mastectomy
Your individual risk for breast cancer recurrence after receiving a mastectomy will depend on several factors, including the type of breast cancer you have and whether it is affected by hormones, the size and location of your tumor, how quickly the cancer cells grew and the stage of cancer at the time of treatment. In particular, if breast cancer has spread to nearby lymph nodes, such as those in the underarm area, the likelihood of recurrence may be higher.
Also Check: What Is The Blood Test For The Breast Cancer Gene
What Are The Signs That Breast Cancer Has Returned
Signs and symptoms of local recurrence on the chest wall after a mastectomy may include: One or more painless nodules on or under the skin of your chest wall.Local recurrenceA new lump in your breast or irregular area of firmness.Changes to the skin of your breast.Skin inflammation or area of redness.Nipple discharge.
Current Strategies For The Management Of Locoregional Breast Cancer Recurrence
In this review, we focus primarily on describing locoregional and systemic management strategies for isolated locoregional recurrences manifesting as isolated first-failure events following mastectomy or breast-conserving therapy.
Advances in the treatment of breast cancer have decreased the rate of isolated locoregional recurrences over time. Surgery, radiation therapy, and systemic therapies are used to manage these failure events and their associated poor prognosis. Operable ipsilateral breast tumor recurrences are treated by either salvage mastectomy or, in select cases, repeat lumpectomy. Axillary nodal recurrences and postmastectomy chest wall relapses are commonly amenable to surgical resection, too. Repeat sentinel node mapping may be undertaken after IBTRs and chest wall recurrences. Aberrant lymphatic drainage, especially after previous mastectomy, is frequently observed. Adjuvant radiation is recommended for most ILRR cases the dose and volume must be adjusted for prior to receipt of therapy. Implementation of adjuvant systemic therapies after ILRR should be based on the expression of molecular markers in the recurrent tumor. Administration of chemotherapy for estrogen receptornegative ILRR is indicated, since it significantly decreases the rate of distant metastases.
Read Also: Breast Cancer Ductal Carcinoma In Situ
Can Breast Cancer Return After A Double Mastectomy
During the course of breast cancer treatment, a woman may decide, after discussion with her doctors, to have both of her breasts removed.
She might choose to have a double mastectomy in the hope that it will reduce the risk of breast cancer recurring in the remaining tissue or a new cancer developing in the opposite, unaffected breast.
A woman who has had breast cancer does not inherently or automatically face an increased risk of being diagnosed with another type of cancer, says Ellis Levine, MD, Chief of Breast Medicine at Roswell Park Comprehensive Cancer Center.
Unless they have an underlying hereditary genetic mutation, I do not consider them at exquisite risk to develop another type of cancer, he says. The cancer that is most often genetically linked to breast cancer is ovarian, due to mutations in the BRCA 1 or BRCA 2 genes.
When mastectomies are performed, surgeons will remove as much of the cancerous tissue as possible. If a woman, in consultation with her doctors, decides to have a skin-sparing or nipple-sparing mastectomy, a small amount of healthy breast tissue may be left behind on the skin to allow for reconstruction of her breasts.
Even if the full breast is removed, surgeons will not have removed 100% of the breast cells, explains Jessica Young, MD, a breast surgeon at Roswell Park. The risk of cancer recurring is lower if the whole breast is removed, but it is not zero percent.
Breast Cancer Treatment
What Causes Breast Cancer Recurrence
The goal of cancer treatments is to kill cancer cells. But, cancer cells are tricky. Treatments can reduce tumors so much that tests dont detect their presence. These weakened cells can remain in the body after treatment. Over time, the cells get stronger. They start to grow and multiply again.
Even surgery to remove a cancerous tumor isnt always 100% effective. Cancer cells can move into nearby tissue, lymph nodes or the bloodstream before surgery takes place.
You May Like: What Foods To Avoid When You Have Breast Cancer
How Do Surgeons Use Tissue From A Womans Own Body To Reconstruct The Breast
In autologous tissue reconstruction, a piece of tissue containing skin, fat, blood vessels, and sometimes muscle is taken from elsewhere in a womans body and used to rebuild the breast. This piece of tissue is called a flap.
Different sites in the body can provide flaps for breast reconstruction. Flaps used for breast reconstruction most often come from the abdomen or back. However, they can also be taken from the thigh or buttocks.
Depending on their source, flaps can be pedicled or free.
- With a pedicled flap, the tissue and attached blood vessels are moved together through the body to the breast area. Because the blood supply to the tissue used for reconstruction is left intact, blood vessels do not need to be reconnected once the tissue is moved.
- With free flaps, the tissue is cut free from its blood supply. It must be attached to new blood vessels in the breast area, using a technique called microsurgery. This gives the reconstructed breast a blood supply.
Abdominal and back flaps include:
Flaps taken from the thigh or buttocks are used for women who have had previous major abdominal surgery or who dont have enough abdominal tissue to reconstruct a breast. These types of flaps are free flaps. With these flaps an implant is often used as well to provide sufficient breast volume.
Recommended Reading: Can Asbestos Cause Breast Cancer