Breast Cancer Screening Patient Version
On This Page
Screening is looking for signs of disease, such as breast cancer, before a person has symptoms. The goal of screening tests is to findcancer at an early stage when it can be treated and may be cured. Sometimes a screening test finds cancer that is very small or very slow growing. These cancers are unlikely to cause death or illness during the person’s lifetime.
Scientists are trying to better understand whichpeople are more likely to get certain types of cancer. For example, they look at the person’s age, their family history, and certain exposures during their lifetime. Thisinformation helps doctors recommend who should be screened for cancer, whichscreening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarilythink you have cancer if he or she suggests a screening test. Screeningtests are done when you have no cancer symptoms. Women who have a strong family history or a personal history of cancer or other risk factors may also be offered genetic testing.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests, rather than screening tests.
See the following PDQ summary for more information about cancer screening:
How Private Is Your Genetic Information
Unlike some companies that test DNA to identify relatives, none of OSUs genetic testing partners share information with the police, she told The Dispatch.
Individuals are also protected by the 2008 Genetic Information Nondiscrimination Act , which prevents employers and health insurers from asking about genetic information when making decisions. However, exceptions are made for life insurance and long-term care insurers, who can ask for such information. It is often best to buy such coverage before undergoing genetic testing, said Byrne.
Kalister said that for at-risk individuals like himself, genetic counseling should be a no-brainer.
The counselors are really really good, he said. This is what they do they talk to people about this kind of testing, these results, theyre there to answer questions.
OSU also provides Family HealthLink, a free online tool that estimates cancer risk by reviewing family patterns.
Peter Gill covers immigration and new American communities for The Dispatch in partnership with Report for America. You can support work like his with a tax-deductible donation to Report for America here:bit.ly/3fNsGaZ.
pgill@dispatch.com
Magnetic Resonance Imaging May Be Used To Screen Women Who Have A High Risk Of Breast Cancer
MRI is a procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging . MRI does not use any x-rays and the woman is not exposed to radiation.
Note: The inset shows an MRI image of the insides of both breasts. Credit for inset: The Cancer Imaging Archive .
MRI may be used as a screening test for women who have a high risk of breast cancer. Factors that put women at high risk include the following:
- Certain gene changes, such as changes in the BRCA1 or BRCA2 genes.
- A family history with breast cancer.
- Certain geneticsyndromes, such as Li-Fraumeni or Cowden syndrome.
An MRI is more likely than mammography to find a breast mass that is not cancer.
Women with dense breasts who have supplemental screening show higher rates of breast cancer detection, but there is limited evidence about whether this leads to better health outcomes.
Read Also: Will I Lose My Hair With Radiation For Breast Cancer
Why Should I Choose Msk For Male Breast Cancer Treatment
Because there are so few cases of male breast cancer, it is important to choose a care team that is trained in treating the disease.
The Rare Breast Cancer Program at MSK has that experience. We evaluate and treat about 200 people with early- or advanced-stage rare breast cancer, including male breast cancer, every year.
When men with breast cancer come to MSK, they have access to streamlined, comprehensive care. We offer molecular testing to determine the genetic makeup of each persons tumor. We also provide genetic counseling so we can learn about any cancer predispositions that may affect them or members of their family. Our clinic for men with the BRCA gene ensures that men get the most information they can about their specific disease in an effort to determine which treatments may be best for them. In addition, we have clinical trials just for men based on their specific tumors makeup.
We work with other MSK experts to ensure that you get the care you need beyond medical treatment. Experts in male sexual health, social work, integrative medicine, and other subspecialities can help you manage the stress of breast cancer treatment, as well as its potential side effects, such as chemotherapy-induced nausea, fatigue, loss of appetite, or lymphedema .
We know it is overwhelming to be diagnosed with male breast cancer, but we have the expertise and experience needed to give you the highest quality of care.
What Is The Survival Rate Of Male Breast Cancer
Percent means how many out of 100. The 5-year survival rate for men with breast cancer is 84%. Individual survival rates depend on different factors, including the stage of the disease when it is first diagnosed. If the cancer is located only in the breast, the 5-year survival rate of men with breast cancer is 97%.
You May Like: How To Know If You Have Breast Cancer Male
Where Can I Go To Get Screened
You can get screened for breast cancer at a clinic, hospital, or doctors office. If you want to be screened for breast cancer, call your doctors office. They can help you schedule an appointment.
Most health insurance plans are required to cover screening mammograms every one to two years for women beginning at age 40 with no out-of-pocket cost .
Are you worried about the cost? CDC offers free or low-cost mammograms. Find out if you qualify.
Who Should Have The Exams*
- Pap Tests: All women age 21 and older, especially if they are active sexually, should have regular Pap tests and pelvic exams.
- Breast Exams: All women should have their breasts examined by a doctor or other health professional once a year.
- Mammograms: Women age 40 and older should have regular mammograms, as recommended by their doctor or health professional.
- Prostate Tests: Men age 50 and older should talk with their doctor or other health care professional about prostate cancer screening tests. Screening tests include Prostate Screening Antigen test, and Digital Rectal Exam
- Colorectal Tests: Men and women age 50 and older should have regular colorectal cancer screening tests, as recommended by their doctor or health care professional. These tests may include colonoscopy, sigmoidoscopy, or home-test kits .
- Lung Test: Men and women who are 55-80 years of age may be eligible for a lung cancer screening if they: currently smoke or have quit smoking during the past 15 years and smoke or smoked a pack a day for 30 or more years, or two packs a day for 15 or more years.
*Talk with your doctor about individual screening recommendations. If you have a family history of cancer or are experiencing certain symptoms, you may qualify for screening at an earlier age.
Recommended Reading: Can You Have Breast Cancer At 21
Targeted Cancer Drug Therapy
Your doctor will check your cancer cells for proteins called HER2 receptors. But these are rarely found in male breast cancer. If your cancer cells have a lot of these receptors, your doctor will prescribe a targeted drug treatment for you.
The most common targeted drug for breast cancer is trastuzumab .
Whether A Woman Should Be Screened For Breast Cancer And The Screening Test To Use Depends On Certain Factors
Women with risk factors for breast cancer, such as certain changes in the BRCA1 or BRCA2 gene or certain genetic syndromes may be screened at a younger age and more often.
Women who have had radiation treatment to the chest, especially at a young age, may start routine breast cancer screening at an earlier age. The benefits and risks of mammograms and MRIs for these women have not been studied.
Breast cancer screening has not been shown to benefit the following women:
- Elderly women who, if diagnosed with breast cancer through screening, will usually die of other causes. Screening mammograms for those aged 66 to 79 years may find cancer in a very small percentage of women, but most of these cancers are low risk.
- In women with an average risk of developing breast cancer, screening mammography before age 40 has not shown any benefit.
- In women who are not expected to live for a long time and have other diseases or conditions, finding and treating early stage breast cancer may reduce their quality of life without helping them live longer.
Recommended Reading: Can Estradiol Cause Breast Cancer
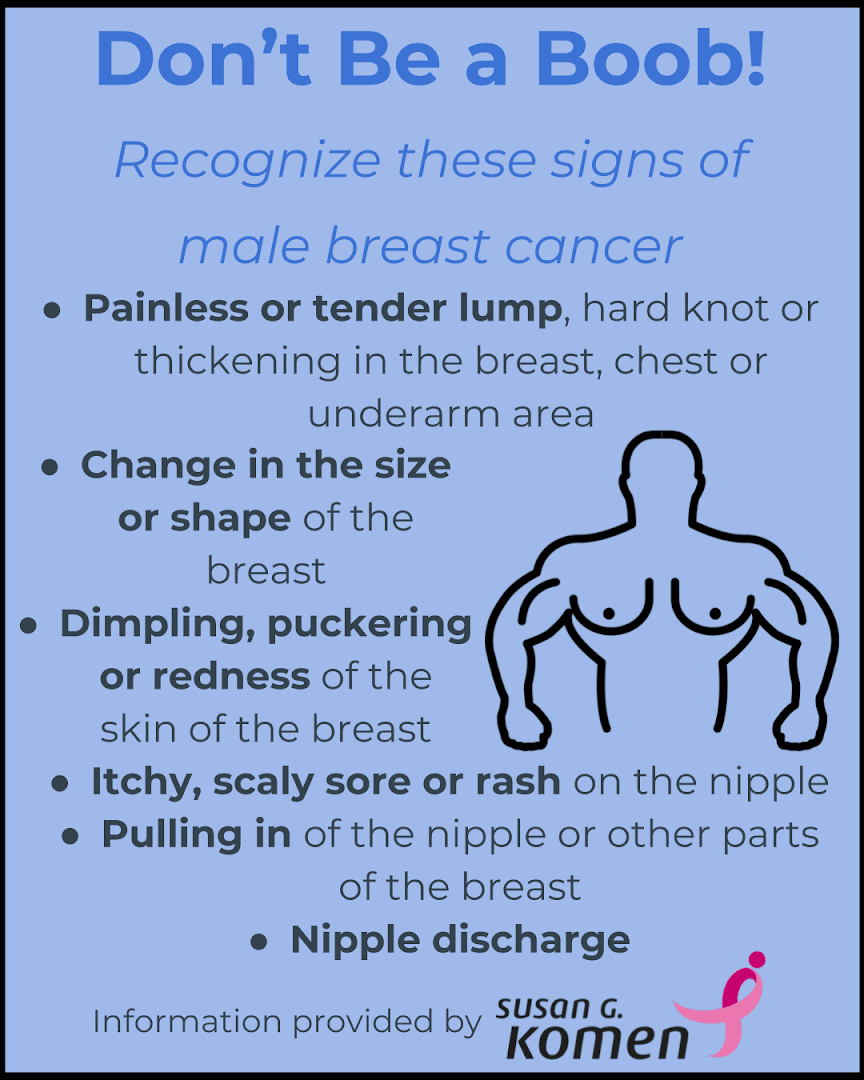
What Are The Symptoms Of Male Breast Cancer
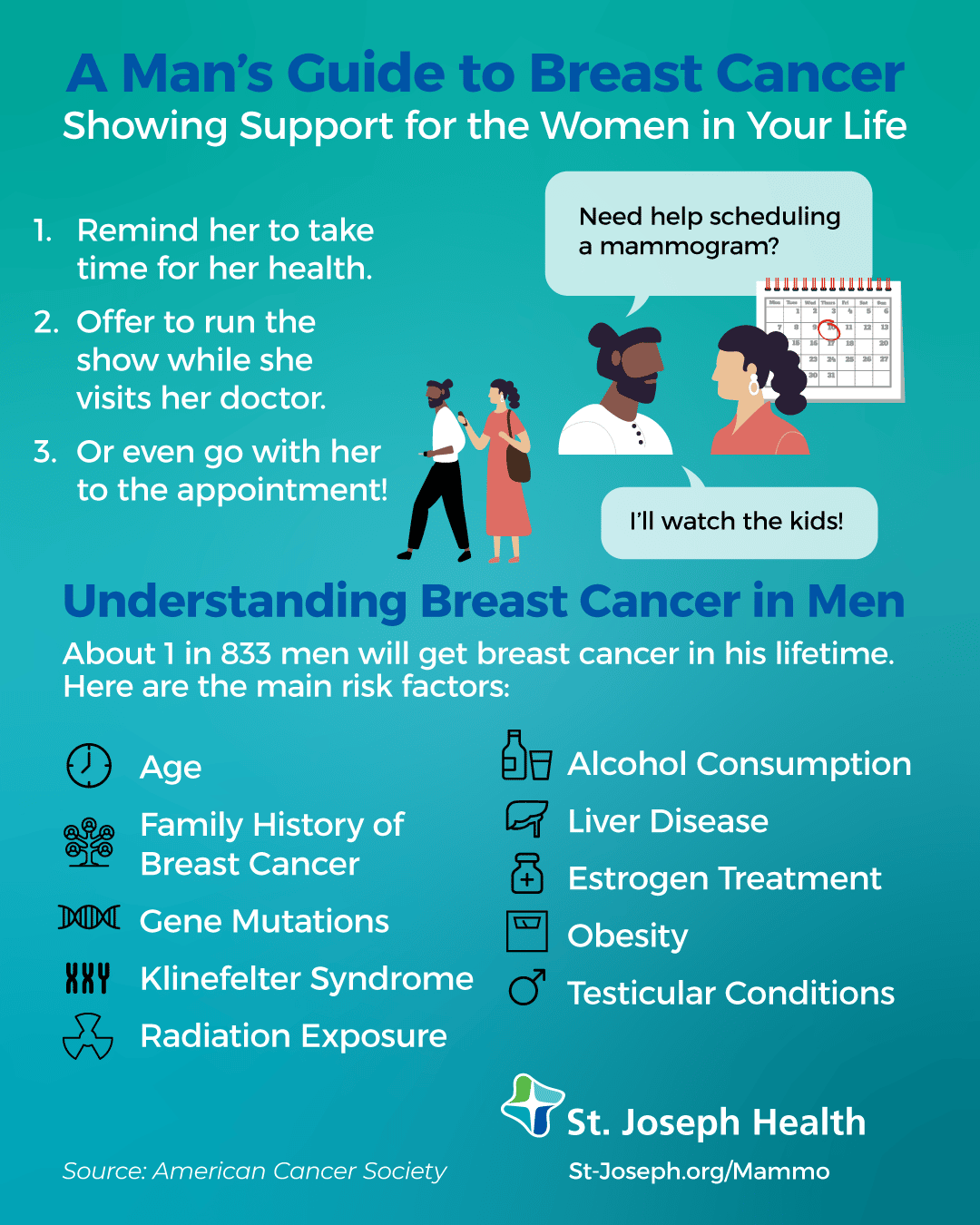
There is no routine breast cancer screening for men, so many men with the disease find a lump in their breast or armpit on their own. Other changes to look for include:
- Unexplained swelling or shrinkage of the breast, particularly on one side only
- Nipple discharge
- Changes to breast skin, such as redness, flaking, thickening, or pitting that looks like the skin of an orange
- A nipple that becomes sunken , red, thick, or scaly
What Is Breast Cancer In Men
Both men and women have breast tissue. In men, most breast tissue is located behind the nipple. Women have a lot more breast tissue than men – and a much higher rate of breast cancer. Cancers can, however, occur in male breast tissue.
Breast cancer is uncommon in men. Around 150 men are diagnosed with breast cancer each year in Australia, mostly over the age of 50. As our population ages, we are likely to see a gradual increase in the number of Australian men diagnosed with breast cancer each year. It is therefore increasingly important to provide information and support to affected men and their families.
Don’t Miss: When Do Breast Cancer Symptoms Start
Lack Of Mammography Screening Guidelines For Men
Yet screening mammography has no role in the general screening of men. In fact no general guidelines exist for breast cancer screening in men. However, the current National Comprehensive Cancer Network guidelines for male carriers of BRCA1 or BRCA2 mutations include annual clinical breast examination and self-examination to begin at 35 years old and prostate cancer screening to begin at 45 years old.
Mammography screening is not currently recommended for men though male carriers of BRCA 1 or BRCA 2 mutations may pursue screening if it is recommended by their physicians.
New research indicates that as genetic testing becomes more accessible and we are better able to identify men at risk for breast cancer screening mammography may offer benefits to these groups.
This brief focuses on mammography guidelines for men, but we will focus on transgender screening guidelines in an upcoming article.
- 180 North Dean Street, Englewood, NJ 07631
- info@BergenImagingCenter.com
Possible Drawbacks Of Screening High Risk Men
There is no established screening regimen for males, and no research has been conducted to determine the optimal screening strategy in this population as men are not typically screened. Although there is interest in improving research to inform prevention, early detection and management of male breast cancer , there have been no studies evaluating the impact of image-based screening on survival or disease-specific mortality. In regards to mammography, one potential confounder of mammographic screening in men is the presence of gynecomastia, seen in approximately 50% of asymptomatic males, and in up to 60% of men presenting with a symptom however, this is not typically a diagnostic challenge. The presence of gynecomastia may, however, increase rate of false positives, a known limitation of screening in women. In addition, when considering any screening program, which utilizes ionizing radiation, the potential risks associated with increased radiation exposure must be considered.
Read Also: What Does Inflammatory Breast Cancer Look Like
N Categories For Breast Cancer
N followed by a number from 0 to 3 indicates whether the cancer has spread to lymph nodes near the breast and, if so, how many lymph nodes are involved.
Lymph node staging for breast cancer is based on how the nodes look under the microscope, and has changed as technology has improved. Newer methods have made it possible to find smaller and smaller collections of cancer cells, but experts haven’t been sure how much these tiny deposits of cancer cells affect outlook.
Its not yet clear how much cancer in the lymph node is needed to see a change in outlook or treatment. This is still being studied, but for now, a deposit of cancer cells must contain at least 200 cells or be at least 0.2 mm across for it to change the N stage. An area of cancer spread that is smaller than 0.2 mm doesn’t change the stage, but is recorded with abbreviations that indicate the type of special test used to find the spread.
If the area of cancer spread is at least 0.2 mm , but still not larger than 2 mm, it is called a micrometastasis . Micrometastases are counted only if there aren’t any larger areas of cancer spread. Areas of cancer spread larger than 2 mm are known to affect outlook and do change the N stage. These larger areas are sometimes called macrometastases, but are more often just called metastases.
NX: Nearby lymph nodes cannot be assessed .
N0: Cancer has not spread to nearby lymph nodes.
N1c: Both N1a and N1b apply.
N3: Any of the following:
N3a: either:
N3b: either:
Colon And Rectal Cancer Screening
Most men and women over the age of 45-50 should undergo routine screening for colon and rectal cancer, up until age 75. The American Cancer Society suggests starting screening at age 45, whereas the United States Preventive Services Task Force suggests starting at age 50. Insurance may not cover screening before the age of 50 so you should talk with your provider and insurance company before screening. Testing may be appropriate for younger people with a high-risk personal or family health history.
Options for colon cancer screening can be divided into those that screen for both cancer and polyps, and those that just screen for cancer. Tests that screen for cancer and polyps include flexible sigmoidoscopy, colonoscopy, double-contrast barium enema, or CT colonography . Tests that screen mainly for cancer include stool testing for blood, or stool DNA testing. Learn more about colorectal cancer screening options on OncoLink.
The “preferred screening” recommended by the American College of Gastroenterologists is a colonoscopy every 10 years. The ACS recommends screening beginning at age 45 , using one of the following testing schedules:
Tests that find polyps and cancer:
- Flexible sigmoidoscopy every 5 years, or
- Colonoscopy every 10 years, or
- CT colonography every 5 years.
Tests that primarily test for cancer:
- Yearly guaiac-based fecal occult blood test *, or
- Yearly Highly sensitive fecal immunochemical test *, or
- Multi-targeted stool DNA test , every 3 years*.
Read Also: What To Do If Breast Cancer Runs In Your Family
Male Breast Cancer Screening In High
Mammograms are more effective at detecting breast cancer in high-risk men than in women who are at average risk of developing the disease, and could provide potentially lifesaving early detection of male breast cancer.
Thats according to a new study researchers are calling the first of its kind and the largest review in the United States of the medical records of men who have had a screening mammogram.
This is important research, as no prior study has been done in males about screening with mammography, said University of Ottawa radiology professor Dr. Jean Seely, who was not involved in the study.
Male breast cancer has a poor prognosis and has not benefited from same improvements in mortality as women in the past 30 years, so improved study of how to improve male breast cancer survival is desirable, Seely said.
A lot of male survivors of breast cancer will develop a second cancer later in life, and if we can just detect them earlier it can really improve their outcome said study lead Dr. Yiming Gao, a diagnostic radiologist at NYU School of Medicines Perlmutter Cancer Center.
Yet theres no data to show whether mammogram screening is useful or not, Gao said. So we looked at this particular subgroup that underwent screening to see if it was.
Should You Get Genetic Testing
Byrne leads a genetics clinic at the OSU Comprehensive Cancer Center Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. As a licensed genetic counselor, she helps patients decide whether to undergo genetic screening, how to interpret results, and next steps.
That includes prostate cancer.
I think there hasnt been enough messaging to say: prostate cancer is something you should have genetic testing . There is a lot of media and coverage about breast cancer and genetics, but the message was not as strong for prostate cancer until recently, she said.
Certain people may want to consider genetic screening based on their ethnicity. While only one in 400 individuals in the general population has a harmful BRCA mutation, that statistic rises to about one in 50 among Ashkenazi Jews, who trace their ancestry to central and eastern Europe.
Don’t Miss: Can You Get Disability For Breast Cancer
Transgender Breast Cancer Screenings
Transgender people have a different gender identity than the sex they were assigned at birth. It is believed that 0.5 percent of the population is transgender. The word transgender is sometimes abbreviated to trans. A transgender man is someone with a male gender identity but a female sex assigned at birth . A transgender woman is someone with a female gender identity but a male sex assigned at birth .
Transgender women and men can develop breast cancer. Therefore, each patient should talk with their health care provider about their breast cancer screening options. Below are the current screening recommendations for transgender women and men.