Bloated Belly And Other Gut Trouble
Ive seen many patients who complain of bloating after having their IUD placed. We are just at the cusp of understanding how our gut, microbiota and hormones interact, but we do know they are all intimately linked.
In my practice, Ive reviewed womens timelines and found that all their digestive symptoms began following the IUD placement. Some of these patients have gone on to be diagnosed with SIBO, yeast overgrowth and bacterial dysbiosis.
While we can not say definitely that the IUD causes digestive issues, it is definitely a symptom I tell my patients to be on the lookout for.
Mirena Migration & Perforation
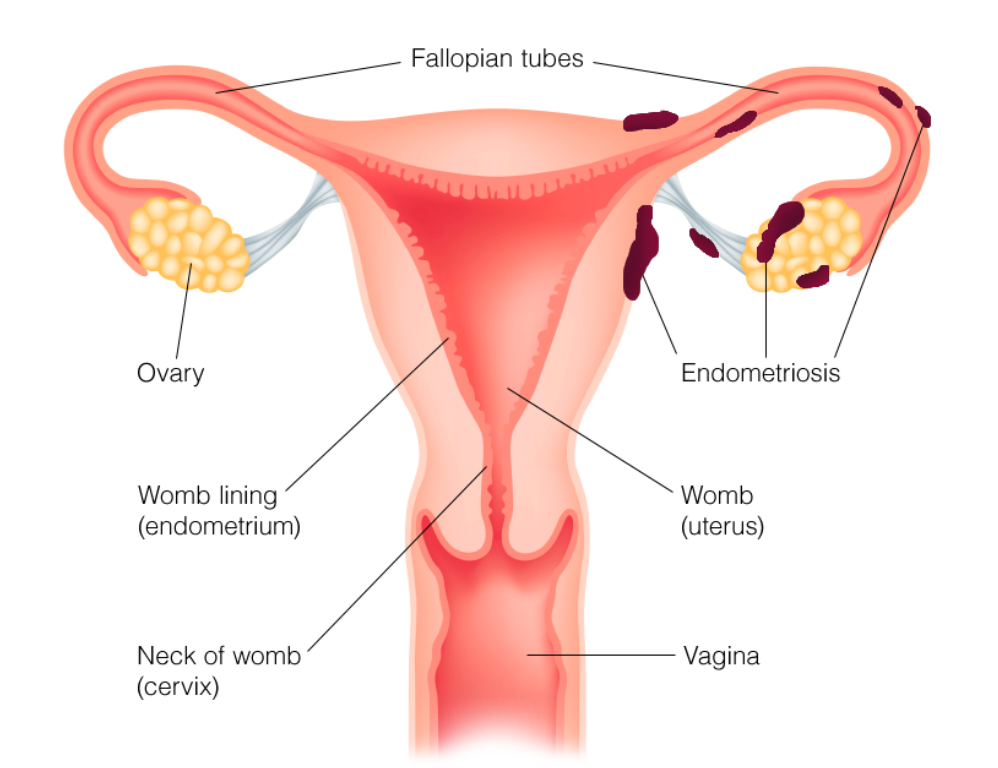
One of the more troublesome complications associated with Mirena is the risk of device migration. Migration occurs when the implanted device loosens from its intended location and moves freely to other locations inside the body. This, in turn, can cause the perforation of surrounding tissues and organs. Aside from being extremely painful, perforation can cause serious long-term effects and also increases the risk of infection to the area it has damaged. Uterine perforation in particular has been particularly dangerous because it can lead to infertility in some women.
There have been reports of Mirena devices found implanted in the uterine wall or ovaries. Additionally, devices have migrated and became lodged in the bladder, pelvic region, and even the abdominal cavity.
these are the most common signs that Migration, when the IUD has moved out of place, either further up your uterus causing perforation, or fallen out has occurred:
Does Roundup Link To Breast Cancer
In regards to what kind of cancer does Roundup cause, the most commonly reported type is non-Hodgkin lymphoma. With that said, there isnt much conclusive evidence available to the public to support the question, does Roundup cause breast cancer. There has not been prominent research on Roundup nor the probable Roundup cancer causing agent, glyphosate regarding the mammary glands. Nevertheless, there have been a few, sporadic studies with significant findings that linked Roundup to breast cancer, with the main ingredient glyphosate being the likely breast cancer-causing agent. A 2005 French study found that glyphosate disrupts aromatase activity. Aromatase is an enzyme often used in new drugs as an inhibitor to treat breast cancer.
Read Also: Stage 3 Advanced Breast Cancer
Too Many People Seem To Be Uninformed About A Drug They Take Every Day
Perhaps the biggest issue here isnt how novel these results are or what small bit of new information we gleaned, but the fact that many seem surprised to find out what doctors have known for literal decades. About 10 million people rely on oral contraception, and each and every one of them should have been informed about the risks they were taking on when they opted to take the pill. Thats not to say that the added risk should have dissuaded them, but just that they should have been allowed to make a truly informed decision.
If you are one of the many people for whom going off hormonal birth control would be a burden, try not to feel scared by this new study. The increased risk you take on is small, and you may be far better off trying to minimize your risk by staying physically active and limiting your alcohol intake. If you are still worried, talk to a medical professional before you make any decisions. Your gynecologist should be able to walk you through the available options and should listen to how you feel about birth control.
Causes Of Breast Asymmetry

During puberty, the left and right breast often develop at a slightly different pace. Breasts may appear asymmetrical until they have finished growing, or they may remain different shapes and sizes throughout a person’s life.
Hormonal changes can cause one or both breasts to change at any point in a person’s life, for example:
- at specific points in the menstrual cycle
- during or near menopause
- during pregnancy or breast-feeding
- when using a hormonal contraceptive, such as birth control pills
Breasts that change size or shape because of hormones often return to normal. Hormonal changes can also cause breasts to feel lumpy or lose fat and tissue. However, if these changes do not go away, it is a good idea to visit the doctor to who will check for any possible health problems.
Some underlying conditions that can affect breast size and shape include:
- Tubular breasts: Also called breast hypoplasia, tubular breasts can develop in one or both breasts during puberty.
- Amastia or amazia: A condition that causes problems in the development of breast tissue, the areola, or nipple.
- Poland Syndrome: Where a chest muscle does not develop properly, which can affect the breast on one side of the body.
Don’t Miss: Breast Cancer Symptom Checker
Should You Avoid Mirena
Based on what we know now, itâs probably a good idea for women with progestin-sensitive breast cancer to choose a different type of birth control. In this type of cancer, cancer cells have substances called receptors that attach to progestin. The progestin helps cancer cells grow.
You may also want to skip Mirena, and any other hormonal birth control, if you have a strong family history of breast cancer. Itâs one small step you can take to help protect yourself.
There are more important steps you can take. These well-studied strategies have been shown time and again to reduce breast cancer risk:
- Reach and maintain a healthy weight
- Get regular exercise
- Limit or skip alcohol
Hormone Dependent Cancers Including Breast Cancer
Although the Mirena coil only releases a small amount of levonorgestrel, we are not sure how much of it, if any, goes to other parts of the body. Because of this, the manufacturers don’t recommend using the Mirena coil if you have had hormone dependent cancers, including breast cancer.
Currently, there is no strong evidence to show whether or not the Mirena coil could cause cancers that depend on hormones to grow. There has been research looking at whether there is a link between the Mirena coil and the risk of breast cancer. The findings from these studies have been mixed.
A recent Norwegian study didnt find a link between this type of coil and breast cancer, but some other studies have found a link. However, studies often have limitations. For example, they sometimes cannot account for other factors that we know are linked to a woman’s risk of breast cancer such as weight or how much alcohol they drank.
If you are concerned you can talk to your GP or specialist about what contraception is best for you.
You May Like: Stage 3 Breat Cancer
Can You Get Cancer From An Iud
IUDs do not cause cancer in otherwise healthy women, but confirmed or suspected cancer of the genital tract is a contraindication to IUD use, because the increased risk of infection, perforation, and bleeding at insertion may make the condition worse.
Similarly, which IUD makes you gain weight?
Hormonal IUDs also list weight gain as a possible side effect. However, according to the Mirena website, fewer than 5 percent of women using it experience weight gain. If you choose to use an IUD, your doctor will have to insert it.
What is a major disadvantage of using an IUD?
Disadvantages. Despite the obvious benefits of an IUD, it has minor and major drawbacks, such as: There is a slight risk of acquiring uterine infection during IUD insertion within 20 days of the procedure. This is increased if the woman is prone to STIs.
How do you know if your IUD is working?
When checking your IUD strings, first wash your hands. If you feel the strings, then your IUD is in place and should be working. If the strings feel longer or shorter than the last time you checked them, or if you feel the hard part of the IUD against your cervix, your IUD may have moved.
What Are Oral Contraceptives
Oral contraceptives are hormone-containing medications that are taken by mouth to prevent pregnancy. They prevent pregnancy by inhibiting ovulation and also by preventing sperm from penetrating through the cervix.
By far the most commonly prescribed type of oral contraceptive in the United States contains synthetic versions of the natural female hormones estrogen and progesterone. This type of birth control pill is often called a combined oral contraceptive. Another type of oral contraceptive, sometimes called the mini pill, contains only progestin, which is a man-made version of progesterone.
Don’t Miss: Stage 3 Breast Cancer Prognosis
Roundup Linked To Cancer
Agribusiness Monsanto has found itself in the middle of a series of lawsuits filed by individuals claiming to have gotten ill with cancer due to Roundup. Roundup is an herbicide used to kill weeds, including annual broadleaf weeds and grasses that compete with crops. St. Louis-based agribusiness, Monsanto, is the manufacturer of Roundup and it has been on the market ever since the 1970s. A study conducted by the International Agency for Research on Cancer found the Roundup cancer causing agent to likely be its main ingredient, glyphosate. Researchers regarded glyphosate as a probable human carcinogen and performed lab tests on animals, concluding the chemical damaged DNA in human cells.
On the contrary, Monsanto has detested those research findings and have argued that their product is safe. The United Nations Food and Agriculture Organization , and the WHO Joint Meeting on Pesticide Residues also took Monsantos side in the Roundup linked to cancer debate, stating that glyphosate is unlikely to pose a risk to human health. With that said, critics, including Greenpeace, have wondered if the UN/JMPRs conclusion was biased due to some of their members having prior involvement with Monsanto.
The Strom Law Firm Defends Consumers Against Dangerous Devices Like The Mirena Iud
Since the Mirena IUD was originally approved for use, numerous exceptions to its use have been discovered. Bayer claimed the Mirena IUD should be used in women who have at least one child and only one sexual partner, but reportedly, some doctors in the Boston area say that the device is only safe for women who have never had children. The Mirena device is also not recommended for use in women with uncontrolled pelvic inflammation, breast, cervical, or uterine cancers , liver disease, or a weak immune system.
If you or a loved one have used the Mirena IUD for contraception and have experienced pain, infection, bleeding, ovarian cysts, intrauterine pregnancy, kidney stones, pelvic inflammatory disease, or organ perforation due to the device, you are not alone. The Strom Law Firm offers free, confidential consultations to discuss the facts of your Mirena personal injury case. Contact us today for a free consultation. .
Also Check: Cancer Is Fungus And Curable With Baking Soda
Assessment Of Risk Of Bias Of The Included Studies
Two independent reviewers assessed the methodological quality of the studies using the Downs and Black instrument. This quality assessment checklist comprises 27 questions, with a maximum possible score of 28 points for randomized studies and 25 points for non-randomized studies. The reviewers assessed the methodological quality of each study and the risk of bias for the following domains: reporting bias , external validity bias , internal validity bias , confounding bias , and power of studies . We gave scores of 0 or 1 for each risk of bias domain and the associated specific questions, except for one item in reporting the subscale for the analysis of the distribution of confounders, which was scored 0, 1, or 2. Finally, the overall quality of evidence for each study was rated depending on the final score: excellent , good , fair , or poor .
Highly Effective Reversible Contraception
There are currently two types of IUDs available in the United States: the copper T 380A and levonorgestrel-containing IUD . The copper-containing IUD contains no hormones, which may make it a preferred option for some women who have survived cancer. The copper T 380A IUD is labeled for use for 10 years, but studies have shown good efficacy of a single IUD used for 12 years to 20 years. While generally well tolerated, some women who have a copper-containing IUD inserted experience increased menstrual cramping and vaginal bleeding.
Don’t Miss: Does Nipple Piercing Cause Breast Cancer
Research That Found No Link
Mirena has been available for more than 15 years. Research has not yet provided a conclusive answer about its possible link to breast cancer.
One of the earliest studies about a link between Mirena and breast cancer appeared in the journal Obstetrics & Gynecology in 2005. The results of that study concluded that there was not an association between the use of Mirena and increased breast cancer risk.
Another study from 2011 in the journal Contraception also did not find an increased risk of breast cancer in people using Mirena.
Hormonal Birth Control And The Risk Of Breast Cancer
Low-dose methods of contraception, such as birth control pills, IUDs, and implant, have been found to increase the risk of breast cancer in women. Dr. Kirtly Parker Jones talks about these new findings from a Denmark study, the benefits and risks of hormonal birth control, and what it could mean for you.
Dr. Jones:
Announcer:
Dr. Jones:
So what did they find? First, the extra risk of breast cancer in women of this age group who took hormonal birth control of any type during this time period was 13 extra breast cancers per 100,000 women per year. That’s a very small number, 13, out of a pretty big number, 100,000. That is, for every 100,000 women using hormonal birth control, there are 68 cases of breast cancer annually compared to 55 cases a year among non-users. Another way to crunch these numbers is to say there was one extra breast cancer for every 7,690 women using hormonal contraception.
Of course, the details are a little more interesting. For the users of hormonal patches, the extra breast cancers were 5 per 100,000, but it ranged from 1 fewer and 11 more, and essentially it wasn’t different from women not using hormonal birth control. Maybe there are just weren’t as many women taking it. It’s not clear, because the hormonal patch is kind of like the hormonal pill.
For women using vaginal rings, there were two fewer breast cancers. But the statistical range was 32 fewer to 28 more. So there wasn’t any increased risk in this group.
Announcer:
You May Like: Youngest Age To Have Breast Cancer
The History Of Mirena Iuds
In the 1960s and 70s, copper IUDs were developed however, it was soon afterwards found that hormonal IUDs would better protect women from unwanted pregnancies. After several other models were made and released, Finnish doctor Jouri Valter Tapani Luukkainen developed the Mirena IUD, which released levonorgestrel into a womans body and was made available to the public in 1990 through Bayer, Inc.With a lifespan of 5 years, a failure rate of only .2% in the first year of use, and completely reversible effects, Mirena was originally thought to be highly effective and became quite popular. Additionally, it was also used for treating women who experienced heavy menstrual bleeding after having given birth.
Gestational Trophoblastic Tumours Such As Molar Pregnancy
The manufacturers recommend that you do not use the Mirena coil if you have recently been diagnosed with a gestational trophoblastic tumour , such as a molar pregnancy or choriocarcinoma. They say you should not use this type of coil while your HCG levels are still raised.
Your specialist will advise you about this.
-
A case-control study on hormone therapy as a risk factor for breast cancer in Finland: Intrauterine system carries a risk as wellHK Lyytinen and othersInternational Journal of Cancer, 2010Volume 126, Issue 2
-
Contemporary Hormonal Contraception and the Risk of Breast CancerL Mørch and othersNew England Journal of Medicine 2017 Volume 377 pages 2228-2239
-
Cancer risk in women using the levonorgestrel-releasing intrauterine system in FinlandT Soini and others
-
Levonorgestrel-releasing and copper intrauterine devices and the risk of breast cancerJ Dinger and othersContraception, 2011 Volume 83, Issue 3
-
Levonorgestrel-releasing intrauterine system use is associated with a decreased risk of ovarian and endometrial cancer, without increased risk of breast cancer. Results from the NOWAC StudyM Jareid and others
Recommended Reading: Metastatic Breast Adenocarcinoma
How To Choose The Right Birth Control For You
Discuss all your birth control options with your doctor. Here are some ideas for how to get that conversation started:
- Be sure to mention if you have a personal or family history of breast cancer or any other type of cancer.
- If you decide on an IUD, ask about the different types and the pros and cons of each. Compare the copper IUD to hormonal IUDs.
- There are many oral contraceptives to choose from. Ask about the benefits and risks of each.
- Other options include the sponge, patches, and shots. There are also diaphragms, condoms, and spermicides.
- No matter what method you ultimately choose, make sure you understand how to use it correctly.
Besides your health, you should also consider your personal preferences and how well each method fits into your lifestyle.
If you choose an IUD, youll need a doctor to insert it and remove it, which you can have done at any time.
Can Other Iuds Increase Your Risk For Breast Cancer Or Other Cancers
Other brands of hormonal IUDs currently on the market are Liletta, Skyla, and Kyleena.
All three labels carry the same warning as Mirena: that you shouldnt use them if you currently have, previously had, or suspect breast cancer.
All acknowledge reports of breast cancer in women using hormonal IUDs. All three say theres no conclusive evidence.
The level of hormones varies slightly with each product. Most studies investigating the link to breast cancer reference levonorgestrel-releasing IUDs in general, not specific brand names.
If you want to avoid hormones altogether, you still have the option of using an IUD.
The copper T380A, marketed under the brand name ParaGard, is hormone-free. It works by triggering an immune response that creates a hostile environment for sperm.
Oral contraceptives also contain hormones. Some have estrogen, some have progestin, and some are a combination of both.
This is another area where studies are inconsistent, according to the National Cancer Institute .
Overall, it appears that oral contraceptives may increase your risk of breast and cervical cancer, while decreasing your risk for endometrial, ovarian, and colorectal cancer.
When considering the association between hormone-based contraceptives and cancer, its important to remember that the risks arent the same for everyone.
Here are a few other things that factor in to your breast cancer risk:
Read Also: What Are The Symptoms Of Stage 1 Breast Cancer