How Is The Stage Determined
The staging system most often used for breast cancer is the American Joint Committee on Cancer TNM system. The most recent AJCC system, effective January 2018, has both clinical and pathologic staging systems for breast cancer:
- The pathologic stage is determined by examining tissue removed during an operation.
- Sometimes, if surgery is not possible right away or at all, the cancer will be given a clinical stage instead. This is based on the results of a physical exam, biopsy, and imaging tests. The clinical stage is used to help plan treatment. Sometimes, though, the cancer has spread further than the clinical stage estimates, and may not predict the patients outlook as accurately as a pathologic stage.
In both staging systems, 7 key pieces of information are used:
- The extent of the tumor : How large is the cancer? Has it grown into nearby areas?
- The spread to nearby lymph nodes : Has the cancer spread to nearby lymph nodes? If so, how many?
- The spread to distant sites : Has the cancer spread to distant organs such as the lungs or liver?
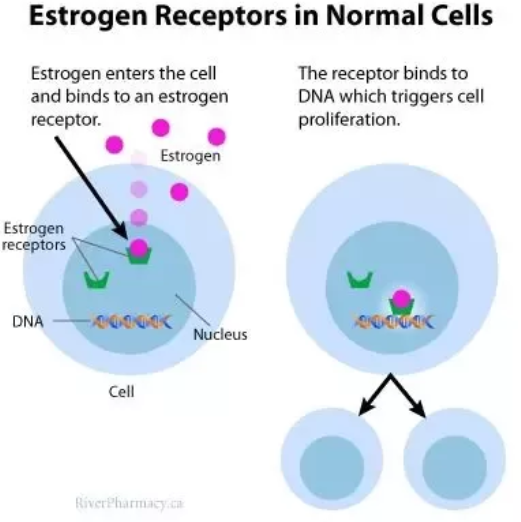
- Estrogen Receptor status: Does the cancer have the protein called an estrogen receptor?
- Progesterone Receptor status: Does the cancer have the protein called a progesterone receptor?
- HER2 status: Does the cancer make too much of a protein called HER2?
- Grade of the cancer : How much do the cancer cells look like normal cells?
In addition, Oncotype Dx® Recurrence Score results may also be considered in the stage in certain situations.
Dna Damage Response Inhibitors
DNA damage response detecting and repairing damaged genes through a variety of ways is a vital protective mechanism to maintain genome stability and prevent breast cancer. DNA single-strand break is mainly repaired by three ways: base excision repair , nucleotide excision repair , and mismatch-repair , and the more serious DNA double-strand break is repaired through two additional pathways: homogeneous recombination and non-homologous end joining .
HR is an error-free repair process, depending on the availability of homologous DNA templates and mainly playing a role in the G2/M phase of the cell cycle. Although NHEJ is more error-prone compared to HR, it is considered to be the main way of DSB repair and works in all phases of the cell cycle .
Mutations in the DDR gene occur in all kinds of breast cancer. Deletion or mutation of BRCA1/2 is present in 10% of patients . DNA dependent protein kinase catalytic subunit , a member of the phosphatidyl inositol-3-kinase-like kinase family that is involved in NHEJ and maintains the structural stability of telomeres, is down-regulated in 57% of early breast cancer cases . In TNBC, BRCA, nonâBRCA HR, and nonâHR DDR genes have mutations , and quite a few proteins involved in DDR including PARP-1 are overexpressed .
A large number of studies have represented that DDR targeted drugs have the potential to treat breast cancer. As shown in Figure 2, an overview of the DNA damage response and repair pathways is detailed below.
Breast Cancer Cell Lines
Part of the current knowledge on breast carcinomas is based on in vivo and in vitro studies performed with cell lines derived from breast cancers. These provide an unlimited source of homogenous self-replicating material, free of contaminating stromal cells, and often easily cultured in simple standard media. The first breast cancer cell line described, BT-20, was established in 1958. Since then, and despite sustained work in this area, the number of permanent lines obtained has been strikingly low . Indeed, attempts to culture breast cancer cell lines from primary tumors have been largely unsuccessful. This poor efficiency was often due to technical difficulties associated with the extraction of viable tumor cells from their surrounding stroma. Most of the available breast cancer cell lines issued from metastatic tumors, mainly from pleural effusions. Effusions provided generally large numbers of dissociated, viable tumor cells with little or no contamination by fibroblasts and other tumor stroma cells.Many of the currently used BCC lines were established in the late 1970s. A very few of them, namely MCF-7, T-47D, MDA-MB-231 and SK-BR-3, account for more than two-thirds of all abstracts reporting studies on mentioned breast cancer cell lines, as concluded from a Medline-based survey.
Metabolic markers
Recommended Reading: What Is Radiation Treatment For Breast Cancer
How Do Hormone Therapies Work
Hormone therapies slow or stop the growth of hormone receptor-positive tumors by preventing the cancer cells from getting the hormones they need to grow.
They work in a few ways:
- Some hormone therapies, such as tamoxifen, attach to the hormone receptor in the cancer cell and block estrogen from attaching to the hormone receptor.
- Some hormone therapies, such as aromatase inhibitors and ovarian suppression, lower the level of estrogen in the body so the cancer cells cant get the estrogen they need to grow.
Cumulative Incidences And Hazard Ratios Of Death From Any Cause And Metachronous Breast Cancer
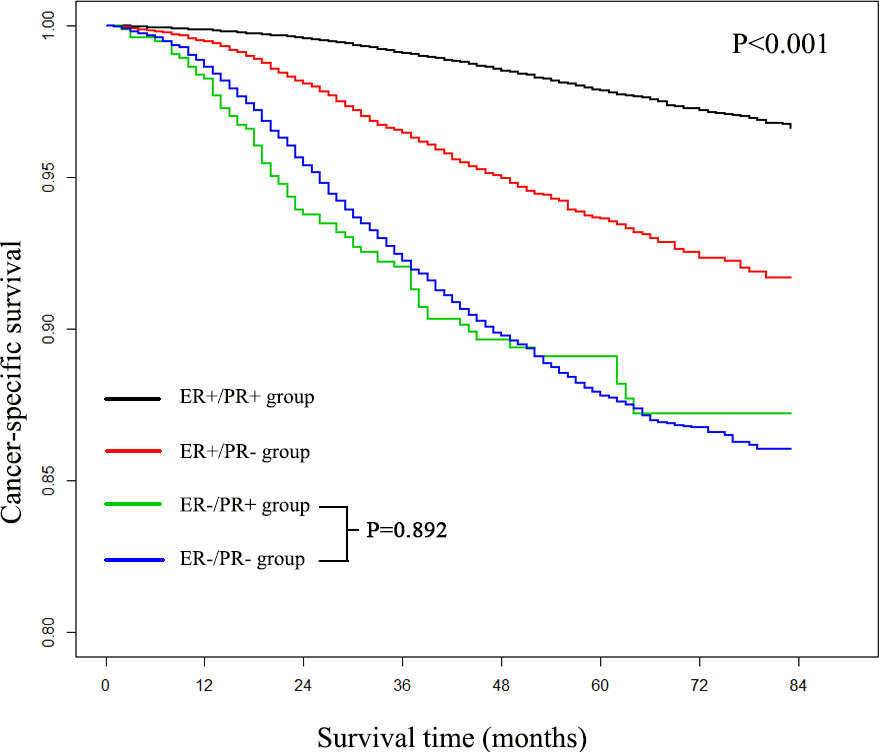
Supplementary Table 12 shows cumulative incidences and hazard ratios for death from any cause. During follow-up, 5416 women died of any cause. In the full regression models, old age at diagnosis , being postmenopausal vs premenopausal at diagnosis , and higher tumor grade were associated with a higher risk of death from any cause . The pattern of better shorter-term but similar longer-term prognosis for ER-positive vs ER-negative tumors was evident also when death from any cause was the outcome . None of the patient or tumor characteristics were associated with risk of metachronous breast cancer .
Recommended Reading: Can Breast Cancer Cause Stomach Pain
Is There A Vaccine For Her2
Nearly a third of HER2-positive patients develop resistance to all the therapies available to treat this cancer. In the hopes of remedying this situation, researchers are working on vaccines for HER2-positive cancer.
This type of cancer is thought to be a good candidate for a vaccine, as its one of the few cancers that provokes an immune response. Researchers are hoping to harness this reaction and train it to help prevent the cancer from developing or returning, or to treat existing tumors.
No vaccine has been approved yet by the FDA, but there are dozens of clinical trials underway.
Activation Of Her2 Through Other Growth Factor Receptors
A role for HER4 in heterodimerizing with HER2 to promote oncogenic signaling is less well studied than that of EGFR or HER3. During mammary development, specifically pregnancy and lactation, HER4 plays a prominent role in inducing alveolar differentiation. HER4 also activates the STAT5 pathway to promote cell survival of these alveolar differentiated cells . In ER+/HER2 breast cancer cells, intracellular HER4 has been shown to promote growth in an ER-dependent manner . Overall, HER4 is one of the more interesting HER family members as it appears to serve both tumor suppressive and tumor promoting functions in the normal mammary gland. Similarly, in breast cancer samples from patients, there is conflicting evidence regarding a role for HER4 in survival outcomes: while many studies have shown associations with better outcome, a few studies suggest the opposite . Further investigation into the role of HER4, either alone, or in combination with HER2, in regulating breast cancer phenotypes and treatment response remains to be conducted.
Don’t Miss: Best Breast Cancer Surgeon Nyc
Will I Need Surgery And What Kind Should I Have
This is an important question but the answer may be less than definitive. It will vary from patient to patient and you may have more than one choice.
According to the American Cancer Society, most women with breast cancer have some type of surgery. But some breast cancers cant initially be surgically removed. In other cases, whether to operate and the type of surgery may depend on the cancers stage, the tumors size and location, the size of your breast and your personal preference.
In women whose breast cancers are operable, the choices are breast-conserving surgery or mastectomy. Mastectomy is the removal of most or all breast tissue and possibly nearby lymph nodes. Within each of those two broad categories are further options. Talk with your oncologist and breast surgeon. If you have any doubts, you may choose to seek a second opinion.
What Does It Mean To Test Her2 Status In Breast Cancer
After a breast cancer diagnosis, the oncologist may recommend testing the tumor for HER2 protein levels. HER2 plays a role in cancer cell growth, and high levels of this protein may indicate the presence of a fast-growing tumor likely to spread. Your care team may use medicines that target HER2 to fight tumors. The American Cancer Society recommends testing all invasive breast cancer tumors for HER2 status, either with tissue from the initial biopsy or when the tumor is removed.
You May Like: Is Stage Two Breast Cancer Curable
What Is Her2 Breast Cancer Testing
HER2 stands for human epidermal growth factor receptor 2. It is a gene that makes a protein found on the surface of all breast cells. It is involved in normal cell growth.
Genes are the basic units of heredity, passed down from your mother and father. In certain cancers, especially breast cancer, the HER2 gene mutates and makes extra copies of the gene. When this happens, the HER2 gene makes too much HER2 protein, causing cells to divide and grow too fast.
Cancers with high levels of the HER2 protein are known as HER2-positive. Cancers with low levels of the protein are known as HER2-negative. About 20 percent of breast cancers are HER2-positive. HER2 positive cancers tend to grow and spread faster than other types of breast cancer. But treatments that specifically target HER2-positive breast cancer can be very effective.
HER2 testing looks at a sample of tumor tissue to find out whether you have HER2-positive breast cancer.
Other names: human epidermal growth factor receptor 2, ERBB2 amplification, HER2 overexpression, HER2/neu tests
What Are The Survival Rates For Her2
The prognosis for HER2-positive cancer has improved greatly with the advent of targeted treatments.
But even with these developments, HER2-positive cancer is still more likely to recur than other cancer types of cancer. Its been estimated that cancer will come back and spread in about 30 percent of people who receive trastuzumab, which is the most commonly used targeted therapy.
Life expectancy after diagnosis can be affected by your hormone receptor status.
According to the National Cancer Institute, the five-year survival rate for those whose breast cancers are both HER2 and HR-positive is 90.7 percent. This means that 90.7 percent of women diagnosed with that cancer subtype will still be alive five years after diagnosis. The five-year survival rate for those whose cancers are HER2-positive but HR-negative is 84.8 percent. This means that 84.8 percent of women diagnosed with that cancer subtype will still be alive five years after diagnosis.
You May Like: What Causes Male Breast Cancer
Understanding Her2 Status In Breast Cancer
Sharing is caring!
HER2 is a protein receptor. Normally, this protein helps breast cells to grow, divide, and repair themselves. But sometimes, some changes occur in the genes that controls the HER2 protein and make the cells grow in a cancerous manner.
If your healthcare provider suspects cancer presence in your mammogram, biopsy or breast MRI, they will first try to identify the type of breast cancer. This information will be the key to understand cancer behaviour and in determining treatment plans.
Read Also: Estrogen Receptor Negative Breast Cancer Prognosis
Chemotherapy For Early Tnbc
Early TNBC is treated with chemotherapy. People with TNBC tend to get more treatment benefit from chemotherapy than people with hormone receptor-positive breast cancers do .
Some people get chemotherapy before breast surgery. This is called neoadjuvant chemotherapy.
For people with TNBC who have cancer remaining in their breast after neoadjuvant chemotherapy, treatment with the chemotherapy drug capecitabine may lower the risk of recurrence and improve survival .
Learn more about chemotherapy.
Read Also: What Is Stage 3a Breast Cancer
You May Like: Breast Cancer Treatment Stage 1
New Advances In Targeted Therapy Of Her2
- 1Key Laboratory of Drug-Targeting and Drug Delivery System of the Education Ministry and Sichuan Province, Sichuan Engineering Laboratory for Plant-Sourced Drug and Sichuan Research Center for Drug Precision Industrial Technology, West China School of Pharmacy, Sichuan University, Chengdu, China
- 2State Key Laboratory Southwestern Chinese Medicine Resources, Chengdu University of Traditional Chinese Medicine, Chengdu, China
There Are Two Ways To Measure The Her
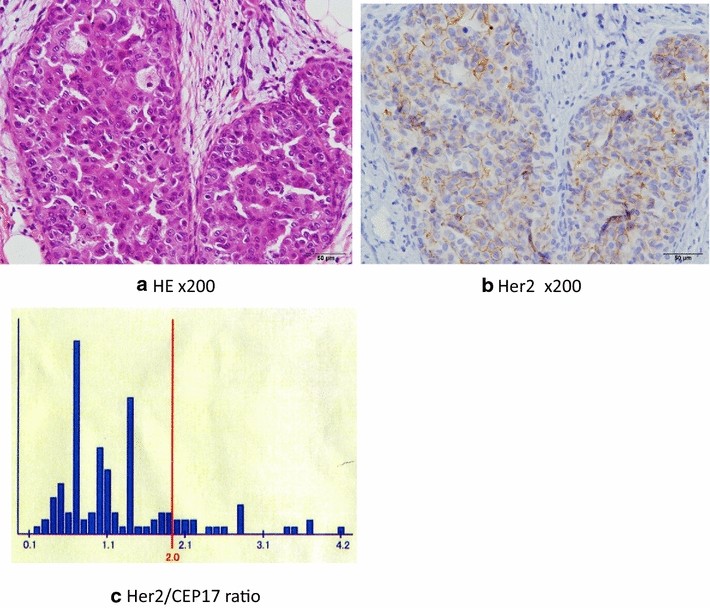
The most common way to measure the HER-2 status of a potential breast cancer tumor is through an immunohistochemistry test. This will likely be part of an overall histological/pathological evaluation of the tumor.
Various tumor markers, including the HER-2 status indicators, give the pathologist a characterization of the tumor. This helps to predict the future behavior and probable responses, of the tumor to different types of treatments.
The immunohistochemistry test of the HER-2 status measures the over-expression of a particular protein and is typically given a score of 0 to +3.
The pathologist actually counts the number of receptors on the surface of the cancer cells. Indeed, the pathologist can see the cells microscopically because they are receptive to certain protein-based dyes and change color.
Scores of 0 and +1 are indicative of a negative status , whilst +2 and +3 are HER-2 positive . There is no in-between state.
Recommended Reading: What Is Estrogen Breast Cancer
Do I Need Genetic Counseling And Testing
Your doctor may recommend that you see a genetic counselor. Thats someone who talks to you about any history of cancer in your family to find out if you have a higher risk for getting breast cancer. For example, people of Ashkenazi Jewish heritage have a higher risk of inherited genetic changes that may cause breast cancers, including triple-negative breast cancer. The counselor may recommend that you get a genetic test.
If you have a higher risk of getting breast cancer, your doctor may talk about ways to manage your risk. You may also have a higher risk of getting other cancers such as ovarian cancer, and your family may have a higher risk. Thats something you would talk with the genetic counselor about.
Links with this icon indicate that you are leaving the CDC website.
- The Centers for Disease Control and Prevention cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination websiteâs privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance on other federal or private website.
Are There Any Risks To The Test
You may have a little bruising or bleeding at the biopsy site. Sometimes the site gets infected. If that happens, you will be treated with antibiotics. A surgical biopsy may cause some additional pain and discomfort. Your health care provider may recommend or prescribe medicine to help you feel better.
There is very little risk to having a blood test. You may have slight pain or bruising at the spot where the needle was put in, but most symptoms go away quickly.
Don’t Miss: What To Buy For Breast Cancer Patient
Her2 Activation Through Crosstalk With Nongenomic Er Signaling
ER has nuclear and non-nuclear functions . While its genomic functions are well studied and its transcriptional role in promoting mitogenic signaling is well understood, its nongenomic functions are less studied. Schiff and colleagues have shown that ligand-bound ER persists in the cytoplasm at low levels, where it directly activates mitogenic signaling from receptor tyrosine kinases including the HER family . This role for nongenomic ER can be initiated by binding with either estrogen or tamoxifen, a commonly used endocrine treatment in premenopausal ER+ breast cancer patients . This cross-activation is amplified in ER+ breast cancer cells with higher RNA and protein levels of HER family members . This avenue of research remains understudied especially in the HER2 subset of ER+ breast cancer, where it could potentially have the most impact in identifying predictive biomarkers for HER2 activation in response to endocrine treatment.
What Does It Mean To Have Her2
When you were diagnosed with breast cancer, the tissue taken during your biopsy was likely tested for several biologic markers. Those results helped your doctor tailor your treatment. If the tissue was diagnosed as HER2-positive, that means that your cancer produced too much of a growth-promoting protein. About 15% of the 268,000 women living in the U.S. diagnosed with breast cancer each year fall into this group.
Don’t Miss: How Do You Diagnose Inflammatory Breast Cancer
What Are The Side Effects Of Treatment
Generally, the side effects of hormonal therapies tend to be mild and fairly well tolerated, says Brufsky. The most common side effects are menopausal symptoms , achiness in the joints and bones, and fatigue. AIs can cause some bone loss , but that can typically be well controlled with bone-modifying medications, Brufsky notes. CDK4/6 inhibitors may cause low white blood cell counts as well as some nausea and diarrhea.
M Categories For Breast Cancer
M followed by a 0 or 1 indicates whether the cancer has spread to distant organs — for example, the lungs, liver, or bones.
M0: No distant spread is found on x-rays or by physical exam.
cM0: Small numbers of cancer cells are found in blood or bone marrow , or tiny areas of cancer spread are found in lymph nodes away from the underarm, collarbone, or internal mammary areas.
M1: Cancer has spread to distant organs as seen on imaging tests or by physical exam, and/or a biopsy of one of these areas proves cancer has spread and is larger than 0.2mm.
Also Check: What Does Cancer Feel Like In Breast
How Are Breast Tumors Tested For Her2
Either a test called an immunohistochemistry test or fluorescence in situ hybridization test is used to find out if cancer cells have a high level of the HER2 protein.
See Testing Biopsy and Cytology Specimens for Cancer and Understanding Your Pathology Report: Breast Cancerto get more details about these tests.