What Does It Mean When A Breast Cancer Is Her2 Negative
When a breast cancer is HER2-negative, it means that the cancerous cells do not contain high levels of the protein HER2. There are many treatment options available for this type of breast cancer, but the prognosis can vary. HER2 stands for human epidermal growth factor receptor 2. The term HER2 may refer to the HER2 gene or to the protein HER2,
Tests On Your Breast Cancer Cells
After a biopsy or surgery to remove breast tissue, a sample of cells is sent to the laboratory. A doctor called a pathologist does various tests on the cells. This can diagnose cancer and also show which type of cancer it is.
Some tests can also show how well particular treatments might work, such as hormone therapies or targeted cancer drugs.
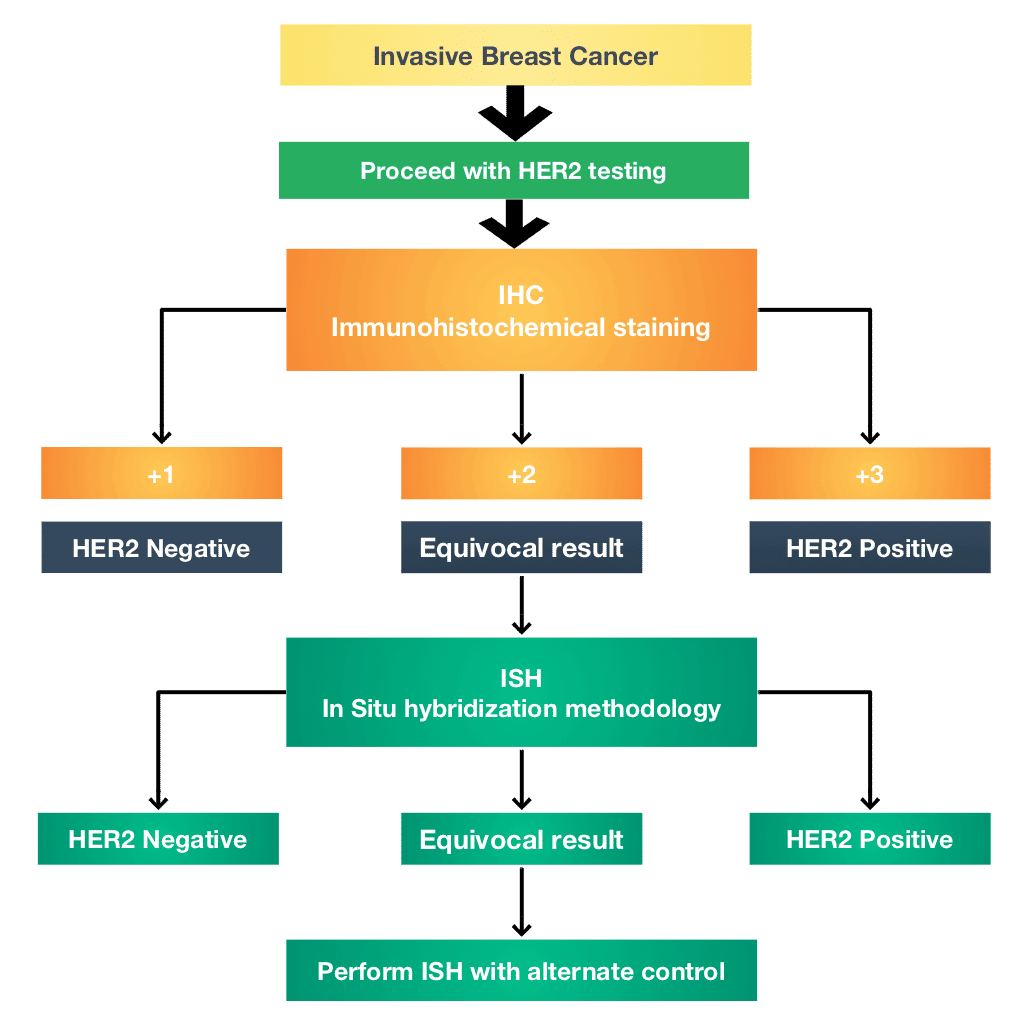
What Is The Best Test For Her2
Two of the most common tests for HER2 status are: IHC test : The IHC test uses a chemical dye to stain the HER2 proteins. The IHC test gives a score of 0 to 3+ based on the amount of HER2 proteins on the surface of cells in a breast cancer tissue sample. If the score is 0 to 1+, its considered HER2-negative.
You May Like: Can You Have Breast Cancer Without Symptoms
Conflict Of Interest Disclosures
We have read and understood Current Oncologys policy on disclosing conflicts of interest, and we declare the following interests: AAJ has previously provided advisory board services to Roche, Novartis, Pfizer, Eisai, and AstraZeneca, and has received educational meeting travel support from Novartis and AstraZeneca . MG and RF have no conflicts to declare. MJC has previously received meeting support from Amgen and Novartis, and has received educational meeting travel support from Novartis .
Treatment Algorithm For 2022
Approximately 40% of patients have PD-L1positive tumors or a high tumor mutational burden and are therefore candidates for immunotherapy with pembrolizumab + chemotherapy. Approximately 10% have BRCA1/2 mutations, where a PARP inhibitor is indicated. The other 50% are eligible to receive sacituzumab govitecan or chemotherapy, or to enroll in a clinical trial. Future strategies will include new antibodydrug conjugates and strategies for augmenting the impact of immunotherapy, Dr. Gradishar said.
Although more and more drugs are becoming available for treatment in HER2-negative breast cancer, the aim is to better identify high-risk patients who need additional therapy, he said. Clinical trials aim to determine these patients and to evaluate strategies for de-escalating treatment in patients with a low risk of recurrence. Asked to cite the key updates to the NCCN Guidelines this year, Dr. Gradishar said, Were getting better at tailoring treatment.
Recommended Reading: When Should You Start Checking For Breast Cancer
Triple Negative Breast Cancer
Triple negative breast cancers don’t have oestrogen receptors, progesterone receptors or HER2 receptors. Around 15 out of 100 women have this type . It is more common in younger women.
Hormone therapies and targeted cancer drugs do not work well for this type of breast cancer. So you are more likely to have chemotherapy.
What Are Gene Activity Tests
Known as molecular assays, genomic assays, or a gene expression profile, these tests look at which genes are active in the cancer cells. The patterns they show help to predict the risk of cancer returning. This can help guide treatment plans.
These tests may be suggested for some early breast cancers to see whether chemotherapy is needed. For example, if the risk of cancer returning is high, chemotherapy may be needed. If the risk is low, hormone therapy, or no extra therapy, may be suggested.
The current molecular assays used include Oncotype DX, EndoPredict, Prosigna and MammaPrint. They are not usually covered by Medicare or private health funds and can cost several thousand dollars.
Ask your medical oncologist if a gene activity test is of use for you. The standard pathology tests done on all breast cancers may be all thats needed for your treatment plan.
Also Check: Breast Cancer Symptoms In Black Females
Immunotherapy In Metastatic Tnbc
Results from Phase I and II clinical trials in metastatic TNBC found that ICIs had the highest activity when given in the first line setting. Clinical activity was increased with increasing PD-L1 expression and when ICIs were given in combination with chemotherapy.22 The Phase III IMpassion130 first line trial randomized 902 patients with metastatic TNBC to treatment with nab-paclitaxel with atezolizumab or placebo.23 The two primary end points were PFS in the intention-to-treat population and PD-L1positive subgroup. Overall survival was according to the study protocol to be tested in the ITT if the finding was significant, then it would be tested in the PD-L1positive subgroup.
In the KEYNOTE-355 trial patients were randomized to pembrolizumab or placebo and could receive any one of a number of chemotherapy options. These options were nab-paclitaxel, paclitaxel, gemcitabine, and carboplatin. The final OS results were presented at ESMO in 2021. In the subset of patients who were PD-L1-positive with a combined positive score of at least 10 , the median overall survival was 23.0 months in the pembrolizumab arm compared to 16.1 months in the control arm . Median progression-free survival was 9.7 months vs 5.6 months, respectively .25
Will I Need Chemotherapy
Typically chemotherapy is a consideration for patients with high-risk breast cancers. Some factors that may indicate the need for chemotherapy are:
- Lymph node involvement.
- Breast cancers in younger patients, especially those below the age of 40.
If you need chemotherapy, it will be given as an outpatient treatment every two to three weeks, delivered either directly into a vein or through a port.
Read Also: Can You Get Breast Cancer Without Brca Gene
Hormone Receptor Status And Early Breast Cancer Prognosis
Hormone receptor status is related to the risk of breast cancer recurrence.
Hormone receptor-positive tumors have a slightly lower risk of breast cancer recurrence than hormone receptor-negative tumors in the first 5 years after diagnosis .
After about 5 years, this difference begins to decrease and over time, goes away .
Recommended Reading: Does Getting Punched In The Breast Cause Cancer
Dna Damage Response Inhibitors
DNA damage response detecting and repairing damaged genes through a variety of ways is a vital protective mechanism to maintain genome stability and prevent breast cancer. DNA single-strand break is mainly repaired by three ways: base excision repair , nucleotide excision repair , and mismatch-repair , and the more serious DNA double-strand break is repaired through two additional pathways: homogeneous recombination and non-homologous end joining .
HR is an error-free repair process, depending on the availability of homologous DNA templates and mainly playing a role in the G2/M phase of the cell cycle. Although NHEJ is more error-prone compared to HR, it is considered to be the main way of DSB repair and works in all phases of the cell cycle .
Mutations in the DDR gene occur in all kinds of breast cancer. Deletion or mutation of BRCA1/2 is present in 10% of patients . DNA dependent protein kinase catalytic subunit , a member of the phosphatidyl inositol-3-kinase-like kinase family that is involved in NHEJ and maintains the structural stability of telomeres, is down-regulated in 57% of early breast cancer cases . In TNBC, BRCA, nonâBRCA HR, and nonâHR DDR genes have mutations , and quite a few proteins involved in DDR including PARP-1 are overexpressed .
A large number of studies have represented that DDR targeted drugs have the potential to treat breast cancer. As shown in Figure 2, an overview of the DNA damage response and repair pathways is detailed below.
Don’t Miss: Will You Die From Stage 4 Breast Cancer
What Is A Mammogram
A mammogram is an X-ray picture of the breast. It can reveal abnormal areas, including cancer, in the breast before they are felt or visible.
Average risk for breast cancer means the following is not present:
- A personal or strong family history of breast cancer
- A genetic mutation that increases breast cancer risk
- A history of radiation to the chest before the age of 30
How Her2 Affects Staging
Your HER2 status helps determine the pathology of your specific breast cancer. Your HER2 status can also help determine how aggressive the cancer is. Your doctor will use this information to evaluate your treatment options.
As of 2018, the breast cancer staging system that the American Joint Committee on Cancer uses now incorporates HER2 status.
Staging is complex and must take various other factors into account, such as:
- the size of the tumors
- the cancers hormone status
- whether the cancer has spread to nearby lymph nodes
- whether the cancer has spread beyond the breast
- whether the cancer cells look abnormal
For example, these two cancers are both classified as stage 1B:
| HER2-negative |
You May Like: Is Soy Bad For Breast Cancer
Addition Of Cyclin Dependent Kinase Inhibitors To Adjuvant Endocrine Therapy
Recently, the phase 3 Palbociclib Collaborative Adjuvant Study and monarchE adjuvant trials testing different CDKis in endocrine receptorpositive/HER2-negative breast cancer have reported results. The PALLAS trial investigated a primary endpoint of invasive DFS for patients who received standard endocrine therapy alone or in combination with the CDK4/6 inhibitor palbociclib for 2 years. PALLAS was a multicenter open-label randomized trial that studied patients with stage II or III breast cancer. A preplanned analysis was performed, and the PALLAS trial was stopped because of futility . The monarchE trial also measured a primary endpoint of IDFS for patients who received standard endocrine therapy alone or in combination with the CDK4/6 inhibitor abemaciclib for 2 years. monarchE is a multicenter open-label randomized trial that studies a population of patients at high risk for recurrence with four or more pathologically positive lymph nodes or one to three lymph nodes and high-risk features such as primary tumor of at least 5 cm, grade 3 tumor, or Ki67 of at least 20%. monarchE showed a significant improvement in IDFS with abemaciclib and endocrine therapy versus endocrine therapy alone with respective IDFS rates of 92.2% versus 88.7% at 2 years. The monarchE paper and the PALLAS trial press release indicate a difference between CDKi types in the adjuvant setting. Whether there are differences between CDKis in the neoadjuvant setting remains to be seen.
Her2 Low Breast Cancer Expert: Precise Diagnosis Can Lead Topersonalized Treatment
As part of a complete breast cancer diagnosis, patients will learn their HER2 status. The human growth receptor 2 or HER2 is something each of us has. It tells cells when to grow and when to stop growing.
When it comes to cancer, too much HER2 can make cells grow out of control, leading to a more aggressive disease. But what happens when the opposite is true?
Naoto Ueno, M.D., Ph.D., is leading groundbreaking research in HER2 low breast cancer, a new subtype designation for which the Food and Drug Administration recently approved the first treatment targeting low levels of HER2.
He explains what it means to have HER2 low breast cancer and how creating more precise diagnoses can lead to more effective treatments for patients.
How is HER2 status classified?
After an initial breast cancer diagnosis, tissue from the tumor will be sent for special testing called an immunohistochemistry test . This test will show how much HER2 is on the surface of the cancer cell.
If the IHC score is more than three, the tumor is HER2 positive. For years, any score lower than three was considered HER2 negative. Now, thanks to more detailed testing, theres a name for HER2 levels between 1-2: HER2 low.
A score of zero is called HER2 negative.
Sometimes, additional testing is necessary to confirm HER2 status. Fluorescence in situ hybridization is a pathology technique that looks at the gene that encodes HER2 to see how many copies are present. Results will either be positive or negative.
Recommended Reading: What Is Primary Breast Cancer
Targeting The Pi3k/akt Pathway
There is evolving recognition that approximately 35% of TNBCs have alterations in the PIK3CA/AKT1/PTEN pathway. Among the targeted drugs in development are the pan-AKT inhibitors ipatasertib and capivasertib, the pan-class I PI3K inhibitors copanlisib and pictilisib, and the dual PI3K/mTOR inhibitor gedatolisib.
Initial trials of the AKT inhibitors provided a mixed signal of efficacy. In the phase II PAKT2 trial, capivasertib + paclitaxel improved median OS from 12.6 months to 19.1 months .20 This benefit was most pronounced in patients with PIK3CA/AKT1/PTEN-altered tumors, with a median PFS of 9.3 months with capivasertib/paclitaxel and 3.7 months with paclitaxel . The AKT inhibitor ipatasertib in combination with paclitaxel similarly improved PFS , with an encouraging OS, in patients with PIK3CA/AKT1/PTEN alterations in the LOTUS trial.21 This was followed, however, by disappointing results from the phase III IPATunity 130 study,22 where the PFS curves were superimposable and overlapping. Targeting AKT is currently being evaluated in the 800-patient phase III Capitello-290 trial of capivasertib .
Cancer And The Female Breast
Figure: Breast and Adjacent Lymph Nodes
Figure: The female breast along with lymph nodes and vessels. An inset shows a close-up view of the breast with the following parts labeled: lobules, lobe, ducts, nipple, areola, and fat.
Inside a woman’s breast are 15 to 20 sections, or lobes. Each lobe is made of many smaller sections called lobules. Fibrous tissue and fat fill the spaces between the lobules and ducts . Breast cancer occurs when cells in the breast grow out of control and form a growth or tumor. Tumors may be cancerous or not cancerous .
Additional Information
Kohler BA, Sherman RL, Howlader N, Jemal A, Ryerson AB, Henry KA, Boscoe FP, Cronin KA, Lake A, Noone AM, Henley SJ, Eheman CR, Anderson RN, Penberthy L. Annual Report to the Nation on the Status of Cancer, 1975-2011, Featuring Incidence of Breast Cancer Subtypes by Race/Ethnicity, Poverty, and State. J Natl Cancer Inst. 2015 Mar 30 107:djv048. doi: 10.1093/jnci/djv048. Print 2015 Jun.
Read Also: Breast Cancer Pac Phone Calls
What Does Her2 Positive Mean
HER2 positivity refers to the tumor cells having extra copies of the HER2 gene and/or increased levels of expression of the HER2 protein. HER2-positive tumors grow more rapidly than HER2-negative tumors. The reason that HER2 testing is done is to determine which patients may benefit from HER2-targeted therapy , such as:
Adjuvant Therapy Guided By Response To Neoadjuvant Therapy In Hr
Determining prognosis after neoadjuvant treatment is complex. Achieving a pCR is associated with a better prognosis particularly in TNBC and HER2-positive breast cancer but less informative in HR-positive, HER2-negative breast cancer. The RCB score is generated by pathological information only obtained post neoadjuvant therapy and can be used to calculate long-term outcome. An additional prognostic scoring system is the Clinical-Pathologic Scoring System incorporating estrogen receptornegative disease and nuclear grade 3 tumor pathology ER, estrogen receptor . This scoring system awards points based on the clinical stage at presentation, pathologic staging parameters post neoadjuvant chemotherapy, ER-negative disease and having a tumor that is high grade to generate a score that predicts prognosis.54
In order to try and improve outcome for patients with HR-positive, HER2-negative and residual disease post neoadjuvant chemotherapy the German Breast Group led the PENELOPE-B trial . The trial identified patients who were at a high risk of relapse based on their CPS-EG score and sought to determine if adding the CDK 4/6-inhibitor, palbociclib for one year to standard endocrine therapy would improve DFS.55 Unfortunately, there was no improvement to DFS with the addition of palbociclib to standard endocrine therapy.
Recommended Reading: Where Does Lobular Breast Cancer Spread
What Are The Different Types Of Breast Cancer
Types. HR-positive and triple-negative are the types of HER2-negative breast cancer. based on the presence or absence of hormone receptors on the surface of cancer cells. These types are called hormone receptor-positive breast cancer and triple-negative breast cancer. Estrogen and progesterone are hormones
How Does Her2 Status Affect Breast Cancer Treatment
HER2-positive result could mean your healthcare provider will treat it with different means than other breast cancer types. The treatment plans are also influenced by the stage of the cancer . Generally, a HER2-positive cancer is metastatic , where it spreads to other parts from its origin. However, early detection can make treatments effective and improve the outlook for cancer and increase survival rates.
Following are some of the treatment options:
HER2-positive result could mean your healthcare provider will treat it with different means than other breast cancer types. The treatment plans are also influenced by the stage of the cancer . Generally, a HER2-positive cancer is metastatic , where it spreads to other parts from its origin. However, early detection can make treatments effective and improve the outlook for cancer and increase survival rates.
Following are some of the treatment options:
Recommended Reading: How To Check For Breast Cancer With Implants
How Do I Know If My Breast Cancer Is Her2 Positive Or Her2 Negative
All invasive breast cancers are tested for HER2 levels. This is done in a hospital laboratory on a sample of breast cancer tissue removed during a biopsy or surgery. The results are usually available between one and three weeks later.
There are various tests to measure HER2 levels. IHC is usually done first. It involves a special staining process performed on a sample of breast cancer tissue.
Its reported as a score of 03. A score of 0 or 1+ means the breast cancer is HER2 negative. A score of 2+ is borderline and a score of 3+ means the breast cancer is HER2 positive.
Breast cancers with a borderline result should be retested using more specialised techniques to determine if they are truly HER2 positive or negative.
Also Check: Stage Iiii Cancer