Subgroup Analysis Of Her3+ And Survival Time
Breast cancer
Three articles concerned breast cancer. There was no significant heterogeneity among the studies , so the fixed-effects model was applied. The HER3+ was not a risk factor predicting death in patients with breast cancer .5). No significant publication bias was determined by Begg’s test or Egger’s test .
Breast cancer subgroup analysis of HER3+ and survival time
Digestive tumors
Eight articles concerned digestive tumors . There was significant heterogeneity among these studies , so the random-effects model was applied. Merged effects values showed that the risk of death in HER3+ patients was 1.78-fold than that of HER3 patients .6). No significant publication bias was determined by Begg’s test and Egger’s test .
Digestive tumors subgroup analysis of HER3+ and survival
The gastric cancer subgroup analysis suggested that HER3+ status was an excellent predictive risk factor for death .5). No significant publication bias was determined by Begg’s test and Egger’s test .
The colorectal subgroup analysis showed that HER3+ status was not a predictive risk factor for death .5). No significant publication bias was determined by Begg’s test and Egger’s test .
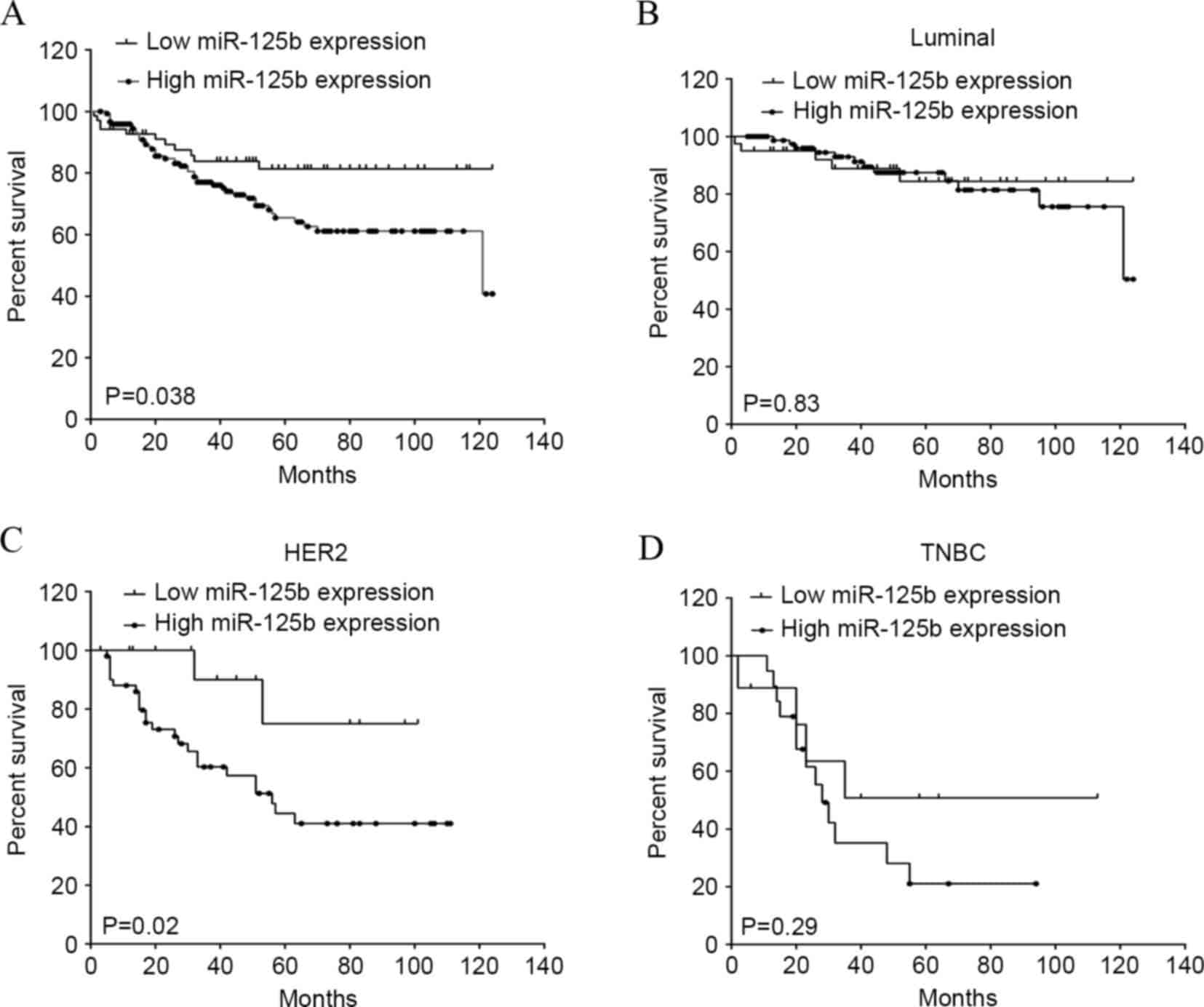
Efficacy In Lung Cancer
In December 2021, the FDA granted a breakthrough therapy designation to patritumab deruxtecan for the treatment of patients with metastatic or locally advanced EGFR-mutated nonsmall cell lung cancer with disease progression on or after treatment with a third-generation TKI and platinum-based therapies.3 Investigators evaluated a dose of 5.6 mg/kg, patritumab deruxtecan in the dose-escalation portion and 2 expansion cohorts of the 3-cohort phase 1 U31402-A-U102 study .4
The agent induced a confirmed ORR of 39% in 57 patients with prior exposure to a TKI and platinum-based chemotherapy. The disease control rate was 72% and a median PFS of 8.2 months .
Among 44 patients in the study who received prior osimertinib and platinum-based chemotherapy, the confirmed ORR was 39% , with a DCR of 68% and a median PFS of 8.2 months .
What Does Her2 Mean In Cancer
Can you tell me what this means? HER2-positive breast cancer is a breast cancer that tests positive for a protein called human epidermal growth factor receptor 2 . This protein promotes the growth of cancer cells. In about 1 of every 5 breast cancers, the cancer cells have extra copies of the gene that makes the HER2 protein.
Also Check: What Is Stage 3c Breast Cancer
How Are Breast Tumors Tested For Her2
Either a test called an immunohistochemistry test or fluorescence in situ hybridization test is used to find out if cancer cells have a high level of the HER2 protein.
See Testing Biopsy and Cytology Specimens for Cancer and Understanding Your Pathology Report: Breast Cancerto get more details about these tests.
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
06 March 2020
François Bertucci, Pascal Finetti, Daniel Birnbaum
13 December 2019
Dong-Yu Wang, Zhe Jiang, Eldad Zacksenhaus
26 July 2018
Yoon-Sim Yap, Angad P. Singh, Derek Y. Chiang
06 October 2020
Fresia Pareja, Britta Weigelt & Jorge S. Reis-Filho
volume 10, Article number: 3009
You May Like: When Is Chemo Necessary For Breast Cancer
What Does Hr Mean In Cancer
What HR-positive means. HR is short for hormone receptor. Breast tumors are tested for both estrogen receptors and progesterone receptors . Each status appears separately on your pathology report. Approximately 80 percent of breast cancers test positive for ER. About 65 percent of those are also positive for PR.
Stage 3 Breast Cancer
Stage 3 breast cancer has spread outside the breast but not to distant sites. The cancer is typically in nearby lymph nodes or skin.
Stage 3 breast cancer is typically harder to treat than earlier stages. This, however, ultimately depends on several factors, including:
- hormone receptivity
A doctor can help a person better understand the stage of cancer and how that will affect treatment options and their outlook.
Healthcare professionals distinguish between the following stages of stage 3 breast cancer:
Don’t Miss: Is Male Breast Cancer Deadly
Analysis Of Parp1 By Ihc
Nuclear non-cleaved PARP1 H-scores in pre-treatment FFPE resection samples were available from TNBC patients in the Nottingham cohort who ultimately received adjuvant chemotherapy, the staining and scoring of which have previously been described by Green et al.. PARP1 H-scores were compared between low/high HER3-EGFR groups by a two-tailed Mann Whitney U test using SPSS.
Outlook For People With Stage 3 Breast Cancer
Its natural to want to know your outlook, but statistics dont tell the whole story. Your breast cancer type, overall health, and many more factors beyond your control may affect treatment outcomes.
Establishing open communication with your treatment team can help you best assess where you are in your cancer journey.
Support groups can be a great source of comfort as you navigate your diagnosis through your treatment and beyond. Your doctors office or hospital can offer some suggestions and resources in your area.
Don’t Miss: Breast Cancer Early Detection Survival Rate
What Does Triple Negative Mean In Terms Of Breast Cancer
Normal breast cells have receptors that respond to hormones such as estrogen and progesterone, which allows them to grow and regress in response to the hormone level. Hormone receptors may or may not be present in breast cancer. About two-thirds of breast cancers are positive and contain these receptors like normal breast cells do. These are less aggressive cancers that are less likely to need chemo and are often treated with hormone therapy and surgery. Radiation may or may not be needed.
HER2/neu , is a protein molecule that has a role in cell proliferation in normal cells. In some breast cancers, this protein is overly produced or positive. For HER2-positive tumors, there a specific medication that targets this protein.
Triple-negative breast cancers are not positive for estrogen receptors, progesterone receptors or HER2 protein. Since these targets are absent in triple-negative breast cancer, chemotherapy is needed, Sun says. Triple-negative breast cancer is often very sensitive to chemotherapy, which, despite the side effects, is an effective treatment that can save lives. Because this is an aggressive cancer, treatment is aggressive also. But there are several ways we can address it.
What Are The Symptoms Of Her2
Its not possible to self-determine whether you have HER2-positive breast cancer. If your doctor suspects cancer, further testing will reveal whether you are HER2-positive.
Overall, its important to see your doctor right away if you notice any of the following symptoms:
- any new or changing lumps in your breast or armpit areas
- clear, colored, or bloody nipple discharge
- unexplained pain in your breasts
- changes in your nipples or breast skin, such as dimpling, reddening, or scaliness
- nipples that turn inward
Don’t Miss: What Questions Should I Ask My Oncologist About Breast Cancer
Detecting Breast Cancer With Screening And Awareness
One of the best ways to improve your chances of surviving breast cancer is to be vigilant about getting routine screenings for the disease. The earlier cancer is found, the better the outlook. According to the ACS, screening reduces breast cancer deaths by 20%. The ACS says that women at average risk for breast cancer should have the option of starting annual screening mammograms between ages 40 to 44 years, while women ages 45 to 54 years should have annual mammograms. Starting at age 55, women should have the option of receiving a mammogram every year or every two years, the ACS says.
Dr. Cairoli points out that younger women who arent covered by screening recommendations should not assume theyre not susceptible to breast cancer. Unfortunately, theres no such thing as too young. Breast cancers can occur in patients even in their 20s. He recommends that all women, especially those not yet of screening age, perform monthly breast self-examinations.Monthly breast self-exams havent been shown to improve outcomes for the population at large, but by knowing your body youll be able to alert your physician if you notice a change, Dr. Cairoli says. And if you do find something unusual, he adds, insist on a physical examination or screening even if your doctor tries to tell you youre too young for breast cancer.
Breast cancer symptoms to be alert for include:
*******
To learn more about RCCA, call 844-928-0089 or visitRCCA.com.
Breast Cancer Survival By Age
Five-year survival for female breast cancer shows an unusual pattern with age: survival gradually increases from 85% in women aged 15-39 and peaks at 92% in 60-69 year olds survival falls thereafter, reaching its lowest point of 70% in 80-99 year-olds for patients diagnosed with breast cancer in England during 2009-2013.
Breast Cancer , Five-Year Net Survival by Age, Women, England, 2009-2013
Read Also: Breast Cancer That Has Spread To Lymph Nodes
Recommended Reading: What Happens With Stage 4 Breast Cancer
What Is The Prognosis For Triple
A good treatment result depends on several factors. Chemotherapy is what can really make a difference in the outcome. The size of the invasive part of the tumor, and the number of involved lymph nodes can also greatly influence your prognosis, Sun says, but adds that if the cancer has spread , the prognosis is less certain.
There is hope, even with this serious diagnosis, and staying optimistic is essential. It can be stressful and scary to go through chemo, but positive thinking can make a difference. You have to believe that its doing you good, and for most people, it does.
Why Is Her2 Testing Done
Experts recommend that every invasive breast cancer be tested for the presence of HER2 because the results significantly impact treatment recommendations and decisions. HER2 testing is not done routinely for ductal carcinoma in situ, except as part of a clinical trial. Whenever breast cancer recurs or spreads, the cancer cells should be retested
Don’t Miss: Does Putting Money In Your Bra Cause Breast Cancer
Inclusion Criteria And Category
All the articles reporting the HRs for HER3+ predicting overall survival using multivariate analysis were included in the systematic assessment. All the articles detected HER3 via IHC. The diagnostic criteria and cut-off of HER3+ expression were depicted and summarized in Table Table2.2. The diagnostic criteria were divided into three categories, and the cutoff values were divided into four categories. . HER3+ was categorized by staining intensity as 0, 1+, 2+, and 3+. 0, samples with no staining at all, or in < 10 % of the tumor cells 1+, a faint or barely perceptible incomplete staining in > 10 % of tumor cells 2+, weak-to-moderate staining in > 10 % of tumor cells 3+, strong staining in > 10-30 % of tumor cells. One cutoff value was Negative = scores 0 Positive = scores 1 + scores 2+ and 3+ another cutoff value was Negative = scores 0 and 1+ Positive = scores 2+ and 3+. . HER3+ was categorized by the percentages of positive cells × staining intensity. . HER3+ was categorized by /the numbers of tumor cores evaluated. The patients were classified into subgroup I, II, III, IV according to the diagnostic criteria and the cutoff values.
Signs And Symptoms To Know
The signs and symptoms of triple-negative breast cancer are the same as with all breast cancers. It may present as a lump, which is more commonly hard, painless and irregular, but can also be soft, round and painful. Other signs include:
- Breast swelling
- A nipple that turns inward
- Skin changes on the breast or nipple, including redness, dryness, thickening or flaking
Recommended Reading: Who Is Considered High Risk For Breast Cancer
What Is The Treatment For Triple Negative Breast Cancer
Healthcare providers and researchers are making significant progress on TNBC treatments. Recent clinical trials are testing new combinations of drugs and new approaches to existing treatments. Some existing treatments are:
- Chemotherapy: Providers might combine chemotherapy and surgery, with chemotherapy being used to shrink your tumor before surgery or after surgery to kill cancer cells throughout your body.
- Surgery: This could be a lumpectomy to remove an individual lump, or a mastectomy to remove an entire breast. Providers then perform a sentinel node biopsy or axillary node surgery to look for signs your breast cancer has spread to your lymph nodes.
- Radiation therapy: Post-surgery radiation therapy helps reduce the chances your cancer will return or recur.
- Immunotherapy: This treatment stimulates your immune system to produce more cancer-fighting cells or help healthy cells identify and attack cancer cells. Immunotherapy can be added to chemotherapy to before surgery to shrink the tumor. You might also receive immunotherapy for about a year after your surgery and post-surgery radiation therapy.
What Are The Treatment Options For Stage 3 Breast Cancer
Another way a doctor may describe stage 3 breast cancer is if its operable or inoperable. This will determine further treatments.
If a cancer is operable, this means a doctor believes most or all of the cancer can be removed with surgery.
Inoperable cancer is still treatable with systemic therapy, but surgery isnt the right option because doctors feel they cant remove enough cancerous cells.
Treatment options for stage 3 breast cancer may include:
- Surgery: known as a mastectomy, to remove cancerous tissue and also to remove lymph nodes
- Hormone therapy: to slow or stop the growth of cancerous cells, if hormones are driving their growth
- Chemotherapy: involves taking medications to kill fast-growing cancer cells
- Targeted therapy: uses your genes to attack cancer cells without harming healthy cells
Your doctor may also recommend a combination of two or more treatments.
Read Also: One Lymph Node Positive Breast Cancer
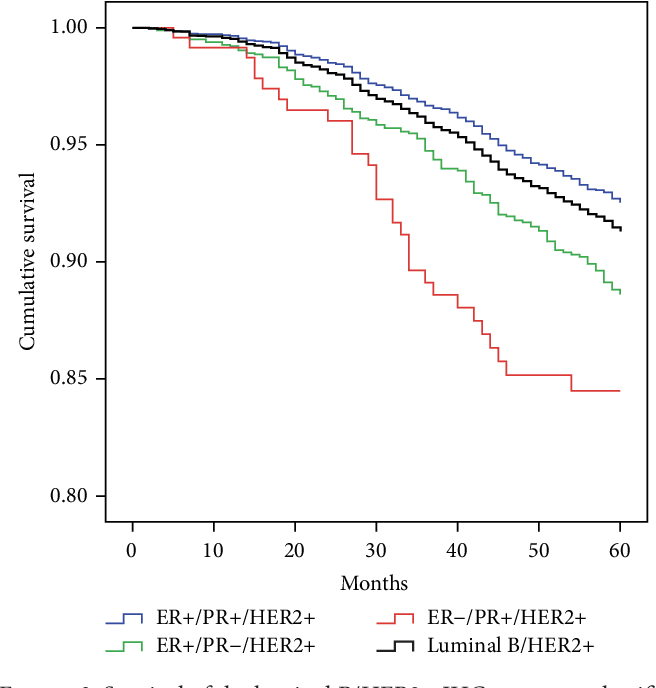
Understanding Her2+ Status And Survival
Doctors use three markers to help define breast cancers and guide treatment. One of those is the HER2 protein. The other two are hormone receptors . When a cancer has none of these, doctors call it triple negative. Until recently, there wasnât much information about how these markers changed survival rates for breast cancer.
A recent study looked at the National Cancer Institute data to see if there were differences in survival for women based on these markers. The study shows there are. Overall, women who have HR+ and HER2- breast cancer do best. But in the later stages, those who have the HER2+ type have better survival rates than those with HER2-. Breast cancers that are triple negative have the lowest survival rates. The 4-year survival rates are as follows:
- HR+/HER2-: 92.5%
- HR-/HER2-: 77.0%
Evaluation And Expression Of Her3
A description of the antibodies used in the included studies is shown in . Various antibodies were used for the evaluation of HER3 expression, although four studies used antibody C-17 and two studies used antibody MS-725-P . The cutoff for overexpression depended on the staining score and the method used. Among the group determined as HER3 overexpressed, the median overexpression of HER3 staining was 42.2%. Melanoma, cervical, and ovarian tumors had the highest expression of HER3, with more than 50% of tumors considered overexpressed. Levels of overexpression in colorectal, gastric, and breast cancer ranged 20% to 60%. Most studies used a combined evaluation of cytoplasmic and membrane staining for determination of expression status . Takikita et al. and Witton et al. used only membranous staining, Spears et al. used a kit evaluating HER2:HER3 dimers, and Begnani and Tanner used the Rajkumar score, a scoring system based on the fraction of positively stained tumor cells .
Read Also: What Are The Chances Of Her2 Positive Breast Cancer Returning
Can Breast Cancer Be Detected By Mammogram
Mammograms can detect a lump or an abnormal growth in the breast that may indicate breast cancer. However, if breast tissue is dense, a small tumor may be missed. In addition to a mammogram, doctors may recommend other imaging tests such as a breast ultrasound, MRI scan, or surgical biopsy to confirm a diagnosis of breast cancer.
Relative Survival Rates For Breast Cancer
The National Cancer Institute gives 5-year relative survival rates for breast cancer based on how far the disease had spread before a doctor found it.
- Localized : 99%
- Unknown stage: 55%
- All stages: 90%
While these numbers can give you a general idea, they are an average for women with any type of breast cancer. They arenât specific to the HER2+ type. They also come from data that researchers collected from 2010 to 2016, so they donât reflect more recent treatment advances.
Recommended Reading: Breast Cancer Stage 4 Metastatic
When Breast Cancer Spreads Should The Cancer Cells Be Retested For Her2
Whenever breast cancer recurs or spreads, the cancer cells should be retested for HER2 as well as for hormone receptor status, as these can change from the original diagnosis. Yamauchi H, et al. HER2 and predicting response to therapy in breast cancer. https://www.uptodate.com/contents/search. Accessed Feb. 23, 2020.
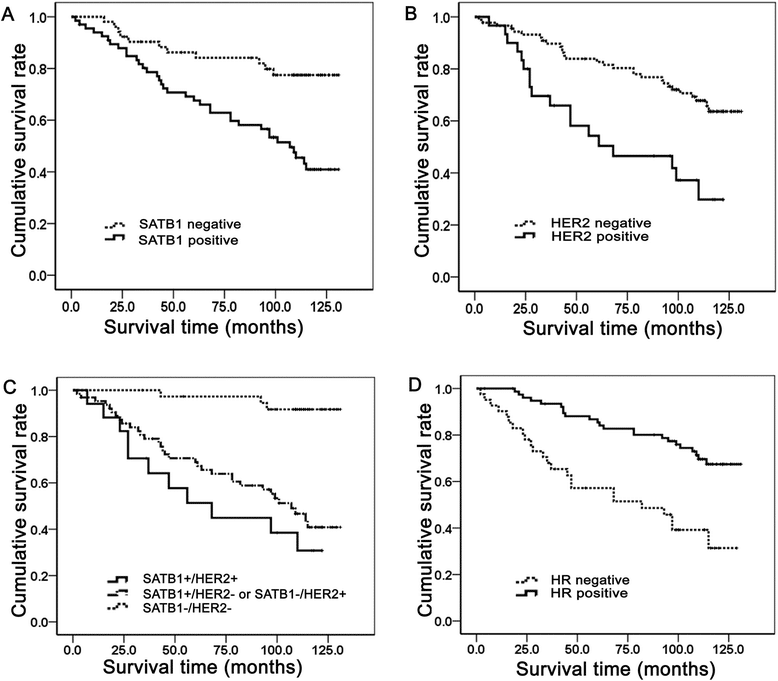
Team Identifies How Certain Immune Cells Contribute To Worse Survival Rates In Her2
Patients with a type of breast cancer called HER2-positive are less likely to survive if their initial treatment fails to eradicate the tumor completely and they have high levels of immune cells called tumor infiltrating lymphocytes in the residual disease.
Dr. Federica Miglietta told the 13th European Breast Cancer Conference that normally tumor infiltrating lymphocytes help the body’s immune system to fight cancer cells. However, for this particular breast cancer, which is driven by human epidermal growth factor 2 receptors on the surface of the cancer cells, post-treatment TILs seemed to be counter-productive if any disease remained after patients had received chemotherapy and anti-HER2 therapy before surgery .
“In patients with HER2-positive breast cancer undergoing neoadjuvant treatment, higher levels of tumor infiltrating lymphocytes when patients are first diagnosed are known to be associated with a greater likelihood of the cancer disappearing from the breast and the axillary lymph nodes and with improved survival,” said Dr. Miglietta, who is a research fellow at the University of Padua and a medical oncologist at the Istituto Oncologico Veneto, Italy. “However, there have been conflicting data on the role of TILs in patients who still have residual disease after neoadjuvant treatment.”
Sixty-eight percent of patients with high levels of TILs in their residual disease were alive after five years compared to 84% of patients with low levels of TILs.
More information:
Recommended Reading: Who Is More Likely To Get Breast Cancer