If You Have A Normal Result
You will receive a letter to let you know your mammogram does not show any signs of cancer. Your next screening appointment will be in 3 years time. Do contact your GP or local screening unit if you havent received an appointment and think you are due one.
It is important to see your GP If you notice any symptoms between your screening mammograms.
Breast Cancer Risk Factors
Family history of breast cancer, ovarian cancer, or other hereditary breast and ovarian syndrome- associated cancer
Known deleterious gene mutation
Prior breast biopsy with specific pathology
Atypical hyperplasia
Lobular carcinoma in situ
Prolonged interval between menarche and first pregnancy
Menopausal hormone therapy with estrogen and progestin
Not breastfeeding
Certain ethnicities
Higher body mass index
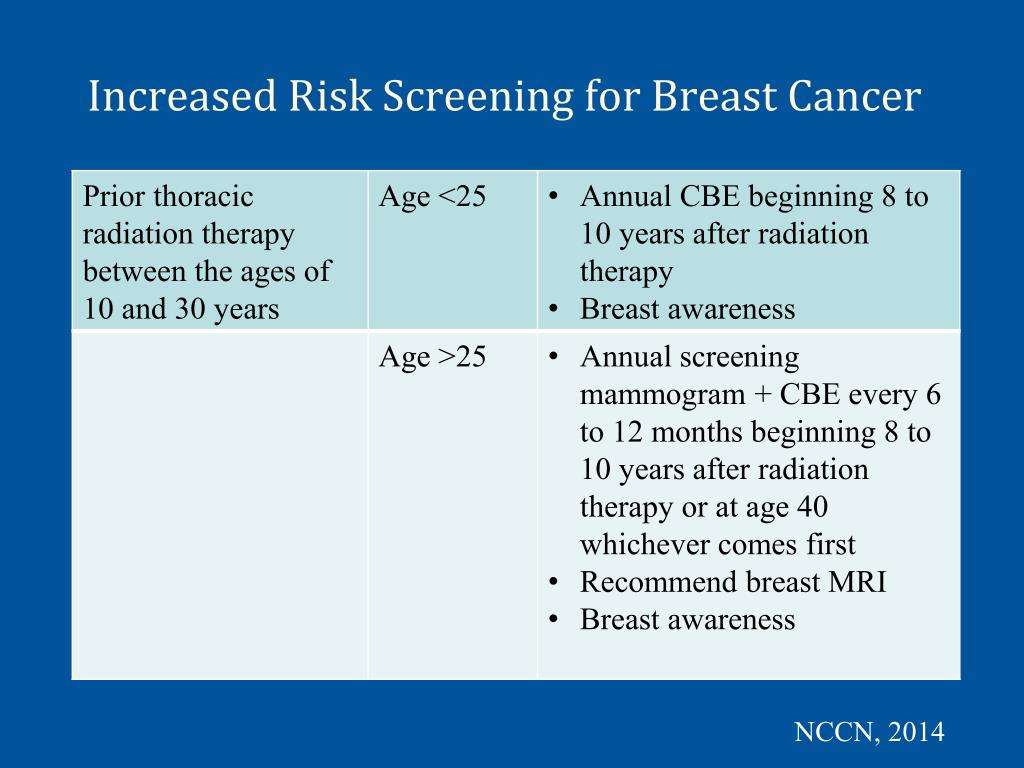
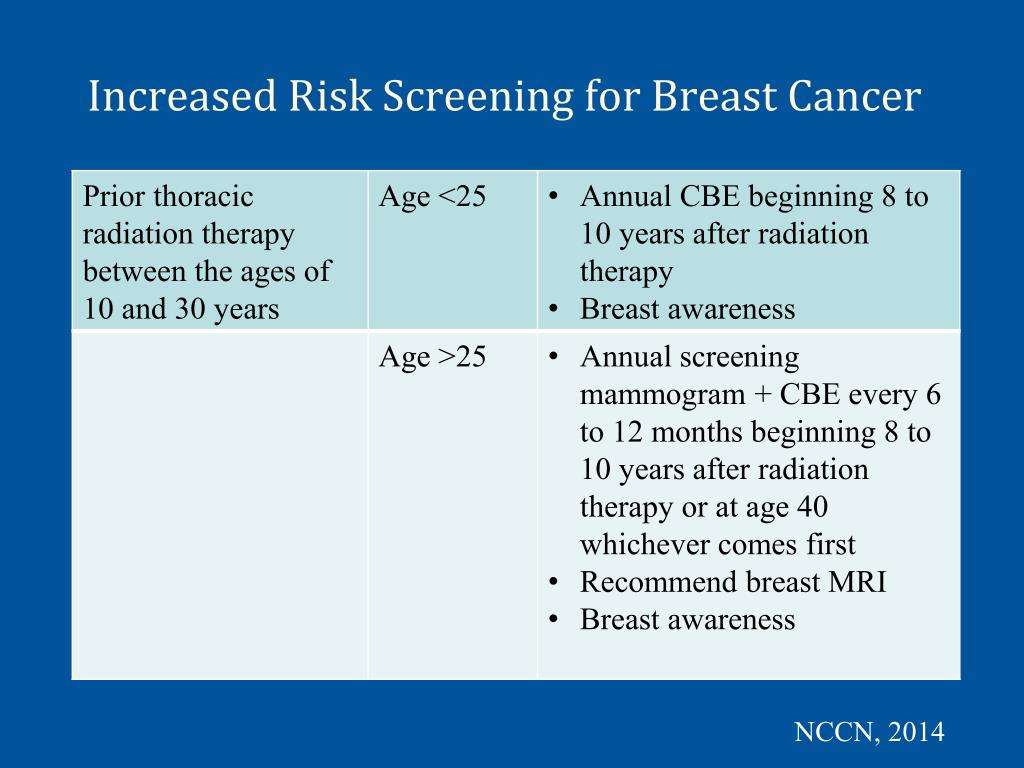
Prior exposure to high-dose therapeutic chest irradiation in young women
How Are Potentially High Risk Women Identified If They Are Currently In The Obsp Being Screened By Mammography
Women who are currently being screened through the Ontario Breast Screening Program may self-identify as being potentially at high risk for breast cancer. OBSP site staff should encourage these women to make an appointment with their healthcare provider. Their healthcare provider will review the OBSP Requisition for High Risk Screening form to determine if they meet the referral criteria for the High Risk OBSP under Category B.
If a woman already has a mammogram booked with the OBSP and is referred to the High Risk OBSP, she should proceed with screening while her genetic assessment is being completed.
You May Like: What’s The Worst Stage Of Breast Cancer
Why Should Women At High Risk For Breast Cancer Receive Screening Magnetic Resonance Imaging
Women at high risk have a greater estimated lifetime risk of developing breast cancer than the general population . For women at high risk, screening with mammography alone has limitations:
- Younger women have greater breast density than older women
- Mammography is less sensitive for women with deleterious genetic mutations due to the faster growth of cancer among these women
Magnetic resonance imaging technology addresses some of the screening limitations of mammography for women at high risk. When used in combination, mammography and MRI find more cancers in women at high risk for breast cancer than using mammography or MRI alone.
Estimate Of Magnitude Of Net Benefit
Digital breast tomosynthesis is an emerging technology for breast cancer screening. Preliminary evidence suggests that it can reduce recall rates for false-positive results and detect more cancer compared with conventional digital mammography. However, it may increase breast biopsy rates, and as currently practiced in most settings, DBT exposes women to more radiation than conventional 2-dimensional mammography. It is not clear whether all of the extra cancer cases detected by DBT actually represent a benefit . Most importantly, no studies assessed the effect of DBT on important health outcomes for women, such as quality of life, morbidity, or mortality. Finally, increased breast density is a common condition that imparts some increased risk for breast cancer, and it reduces the test performance characteristics of mammography as well. Current evidence on the use of adjunctive screening in women with increased breast density is not sufficient to recommend a specific screening strategy. These are important areas for future research.
Read Also: How Often Does Breast Cancer Return
Benefits Of Mammographic Screening
The ACS systematic review also examined the effect of screening mammography on life expectancy. Although the review concluded that there was high-quality evidence that mammographic screening increases life expectancy by decreasing breast cancer mortality, the authors were not able to estimate the size of the increase 23.
What Does The Task Force Recommend For Breast Self Examination And Clinical Breast Exam
The Task Force recommends against routine BSE and CBE , after their review found that neither reduced breast cancer or related deaths in women aged 4074. Furthermore, two large studies identified no reduction in deaths from breast cancer associated with teaching BSE to women aged 31 to 64, but found evidence of increased harm.
Read Also: Does Cheese Cause Breast Cancer
Recommendations On Screening For Breast Cancer In Women 40
This guideline updates the Canadian Task Force on Preventive Health Cares previous recommendations, published in 2011, on breast cancer screening for women aged 40 to 74 years not at increased risk of breast cancer.
This guideline does not apply to women at increased risk of breast cancer including women with a personal or family history of breast cancer, women who are carriers of gene mutations such as BRCA1 or BRCA2 or have a first-degree relative with these gene mutations, and women who had chest radiation therapy before 30 years of age or within the past eight years.
How Will I Be Kept Informed Of My Patients Results
Genetics clinics are responsible for communicating genetic results to women and for sending these results to the referring physician. Please note that wait times for genetic assessment vary across the province it may take up to several months for a woman to receive the results of her genetic testing.
The High Risk OBSP site is responsible for communicating all imaging results to women and for sending these results to the referring physician.
Don’t Miss: What Questions To Ask When Diagnosed With Breast Cancer
Breast Mri For Screening
Breast MRI is not recommended as a routine screening tool for all women. However, it is recommended for screening women who are at high risk for breast cancer, usually due to a strong family history and/or a mutation in genes such as BRCA1 or BRCA2. If you are considered high-risk, you would have breast MRI in addition to your annual mammograms .
Breast MRI is not a perfect tool. Although it is generally considered more sensitive for picking up breast cancer than mammography, it also can miss some cancers that would be detected by mammography. That is why breast MRI is recommended only in combination with other tests, such as mammogram or ultrasound.
Yearly mammograms plus breast MRI screening are typically recommended for women who are at higher-than-average risk of developing breast cancer in other words, at greater than the average 13% risk most women have over the course of an entire lifetime.
The American Cancer Society recommends that all high-risk women those with a greater than 20% lifetime risk of breast cancer have a breast MRI and a mammogram every year. For most women, these combined screenings should start at age 30 and continue as long as the woman is in good health. According to ACS guidelines, high-risk women include those who:
For more information about breast cancer risk, visit the Know Your Risk section.
MRI is also more expensive than mammography, and dedicated breast MRI screening equipment is not widely available.
Response To Public Comment
A draft recommendation statement was posted for public comment on the USPSTF Web site from 21 April through 18 May 2015. In response to the comments received, the USPSTF clarified certain terminology , updated or added references , and provided additional context around the potential risks of radiation exposure due to mammography screening. Additional discussion of the public comments is below.
Benefits of Contemporary Screening Mammography
Screening Mammography in Women Aged 40 to 49 Years
Some commenters incorrectly believed that the C recommendation for women aged 40 to 49 years represented a change from what the USPSTF had recommended in the past. Others thought that the C recommendation meant that the USPSTF was recommending against screening in this group of women. As noted previously, the recommendation for women aged 40 to 49 years was also a C in 2009 . This update clarifies the language around what the C recommendation means. It is not a recommendation against screening but a statement that the decision to undergo screening mammography for women in their 40s should be an informed, individual one, after she weighs the potential benefit against the potential harms.
Screening Mammography in Women Aged 70 to 74 Years or Older
Definition of Overdiagnosis
DBT
Comparison of the USPSTFs Recommendations With Those of Other Organizations
Insurance Coverage and Access to Mammography
You May Like: When Is Breast Cancer Awareness Week
How Can The High Risk Obsp Navigator Support Women
The High Risk OBSP navigator helps guide women through their eligibility process for high risk screening:
- The navigator receives the completed requisition and facilitates the referral to genetics if appropriate.
- If a woman is found to be eligible for the program, the navigator will support her by booking her screening and breast assessment appointments.
- The navigator arranges follow-up breast assessment services after abnormal screens, informs patients of screening results and provides annual recalls for women who are due to be re-screened.
What Happens If I Have Breast Implants
A mammogram is still the best way to detect early breast cancer, even if you have breast implants. But a small amount of the breast tissue might be hidden by the implant.
This means that it is not as easy to see all the breast tissue, and you may have more x rays taken. This will help the doctor see as much of the breast tissue as possible.
It is useful to let the screening unit staff know that you have implants before your mammogram.
Don’t Miss: Can You Feel If You Have Breast Cancer
What Is Breast Screening
Cancer screening involves testing apparently healthy people for signs that could show that a cancer is developing.
Breast screening uses a test called mammography which involves taking x-rays of the breasts. Screening can help to find breast cancers early when they are too small to see or feel. These tiny breast cancers are usually easier to treat than larger ones.
It is important to remember that screening will not prevent you from getting breast cancer but aims to find early breast cancers.
Overall, the breast screening programme finds cancer in around 9 out of every 1,000 women having screening.
Referrals By Clinical Genetics Services Or Oncology Centres
Women who meet the very high risk criteria should be referred to their local breast screening service.
Typically, you should refer to a named high risk coordinator or director of breast screening. Referrals should contain all the necessary information to demonstrate the individual meets the very high risk criteria and should be made using an NHS BSP referral form.
On receipt, each referral must be reviewed to make sure the inclusion criteria have been evidenced. This review must be completed by a consultant radiologist, consultant practitioner or breast clinician experienced in the full range of triple assessment.
Once a referral has been accepted, the woman needs to be appropriately identified as very high risk on BS Select and NBSS. You should scan and upload documentation on to her BS Select record. See more detailed information regarding these processes.
Don’t Miss: What Are Some Symptoms For Breast Cancer
When Very High Risk Screening Stops
Screening should be performed as specified in this guidance.
When a woman reaches 71 years of age routine invitations for very high risk screening will stop. At this stage she is entitled to self-refer for screening. For women in the very high risk programme, this will be annual screening in accordance with her routine screening protocol.
These women should be informed they will need to ask their local screening service directly or their GP can arrange screening for them.
Younger women treated with radiotherapy due to breast cancer are excluded from the NHS BSP very high risk programme.
When To Start Screening
Clinical trials, observational studies, and modeling studies all demonstrate that the likelihood of avoiding a breast cancer death with regular screening mammography increases with age, and this increase in benefit likely occurs gradually rather than abruptly at any particular age. In contrast, the harms of screening mammography either remain constant or decrease with age. For example, about the same number of breast biopsies are performed as a result of screening mammography in women aged 40 to 49 years as in those aged 60 to 69 years, but many more of these biopsies will result in a diagnosis of invasive cancer in the older age group. Thus, the balance of benefit and harms improves with age .
It is, however, a false dichotomy to assume that the only options are to begin screening at age 40 or to wait until age 50 years. As women advance through their 40s, the incidence of breast cancer rises. The balance of benefit and harms may also shift accordingly over this decade, such that women in the latter half of the decade likely have a more favorable balance than women in the first half. Indeed, the CISNET models suggest that most of the benefit of screening women aged 40 to 49 years would be realized by starting screening at age 45.7, 8
Read Also: What Causes Estrogen Positive Breast Cancer
Outside The Screening Population
High risk screening population: women ages 30 to 69
Women 70 to 74 years of age identified as high risk should be screened every year with mammography only at any Ontario Breast Screening Program site.
Women over age 74 can be screened within the Ontario Breast Screening Program however, they are encouraged to make a personal decision about breast cancer screening in consultation with their healthcare provider. The Ontario Breast Screening Program will not recall women over age 74 to participate in the program. To continue screening through the OBSP, a referral is required from a womans healthcare provider.
Accessing Very High Risk Screening
Referrals into the NHS BSP should be through:
- a genetics service by a consultant clinical geneticist, genetic counsellor or an appropriately trained individual nominated by them
- the treating clinician for cancer patients found to carry a genetic mutation that meets the eligibility criteria for very high risk screening
- an oncologist for women who received radiotherapy to sites involving breast tissue to confirm eligibility for very high risk screening)
- BARD for women who received radiotherapy to sites involving breast tissue during treatment for lymphoma
Read Also: How Much Does It Cost To Treat Breast Cancer
American Cancer Society Recommendations For The Early Detection Of Breast Cancer
Finding breast cancer early and getting state-of-the-art cancer treatment are two of the most important strategies for preventing deaths from breast cancer. Breast cancer thats found early, when its small and has not spread, is easier to treat successfully. Getting regular screening tests is the most reliable way to find breast cancer early. The American Cancer Society has screening guidelines for women at average risk of breast cancer, and for those at high risk for breast cancer.
Revisions To Previous Guidance
This guidance has been revised to clarify:
- how very high risk is defined in the NHS BSP and how that relates to the NICE definitions
- what is risk equivalent to carriers of germline BRCA1 and BRCA2 pathogenic variants
- which women aged 25 to 29 should be included in the very high risk screening programme
- who is entitled to a baseline MRI scan
- who is entitled to very high risk screening following radiotherapy to sites involving breast tissue
- when the very high risk screening programme ends
You May Like: How Deadly Is Stage 4 Breast Cancer
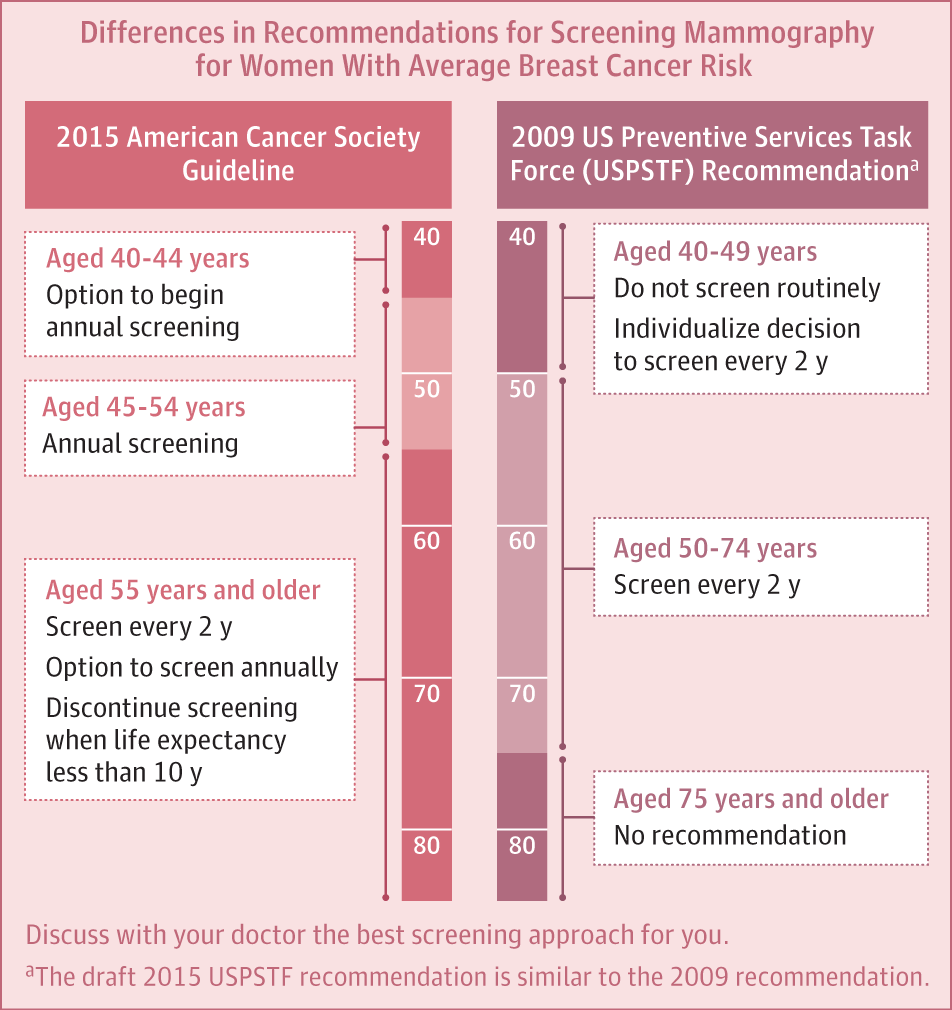
American Cancer Society Guidelines
The 2015 update of the American Cancer Society guidelines includes the following recommendations :
- Women with an average risk of breast cancer should undergo regular screening mammography starting at age 45 years .
- Women aged 45 to 54 years should be screened annually .
- Women 55 years and older should transition to biennial screening or have the opportunity to continue screening annually .
- Women should have the opportunity to begin annual screening between the ages of 40 and 44 years .
- Women should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer .
- The ACS does not recommend clinical breast examination for breast cancer screening among average-risk women at any age .
Women Previously Treated With Total Body Irradiation
Women who have previously received total body irradiation are at an elevated risk of breast cancer in the years following treatment. However, there is insufficient evidence to show that the risk reaches the threshold to qualify this cohort of women for screening in the very high risk programme.
See Tests and frequency of tests for women at very high risk.
Don’t Miss: Is Metastatic Breast Cancer Genetic
Women With Breast Implants
Women with breasts augmented by implants may pose a special challenge. Specific 4-view mammograms may be performed to evaluate the breasts MRI may be especially useful for detecting breast cancer and silicon implant rupture in this group of patients.
See Postsurgical Breast Imaging for more information.
For more information, see Magnetic Resonance Mammography.
American Cancer Society Screening Recommendations For Women At Average Breast Cancer Risk
The COVID-19 pandemic has resulted in many non-emergency procedures being put on hold. This has led to a substantial decline in cancer screening. Health care facilities are providing cancer screening during the pandemic with many safety precautions in place. Learn how you can talk to your doctor and what steps you can take to plan, schedule, and get your regular cancer screenings in Cancer Screening During the COVID-19 Pandemic.
These guidelines are for women at average risk for breast cancer. For screening purposes, a woman is considered to be at average risk if she doesnt have a personal history of breast cancer, a strong family history of breast cancer, or a genetic mutation known to increase risk of breast cancer , and has not had chest radiation therapy before the age of 30.
- Women between 40 and 44 have the option to start screening with a mammogram every year.
- Women 45 to 54 should get mammograms every year.
- Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
- All women should understand what to expect when getting a mammogram for breast cancer screening what the test can and cannot do.
Clinical breast exams are not recommended for breast cancer screening among average-risk women at any age.
Don’t Miss: How Serious Is Grade 3 Breast Cancer