What Factors Affect My Mammogram
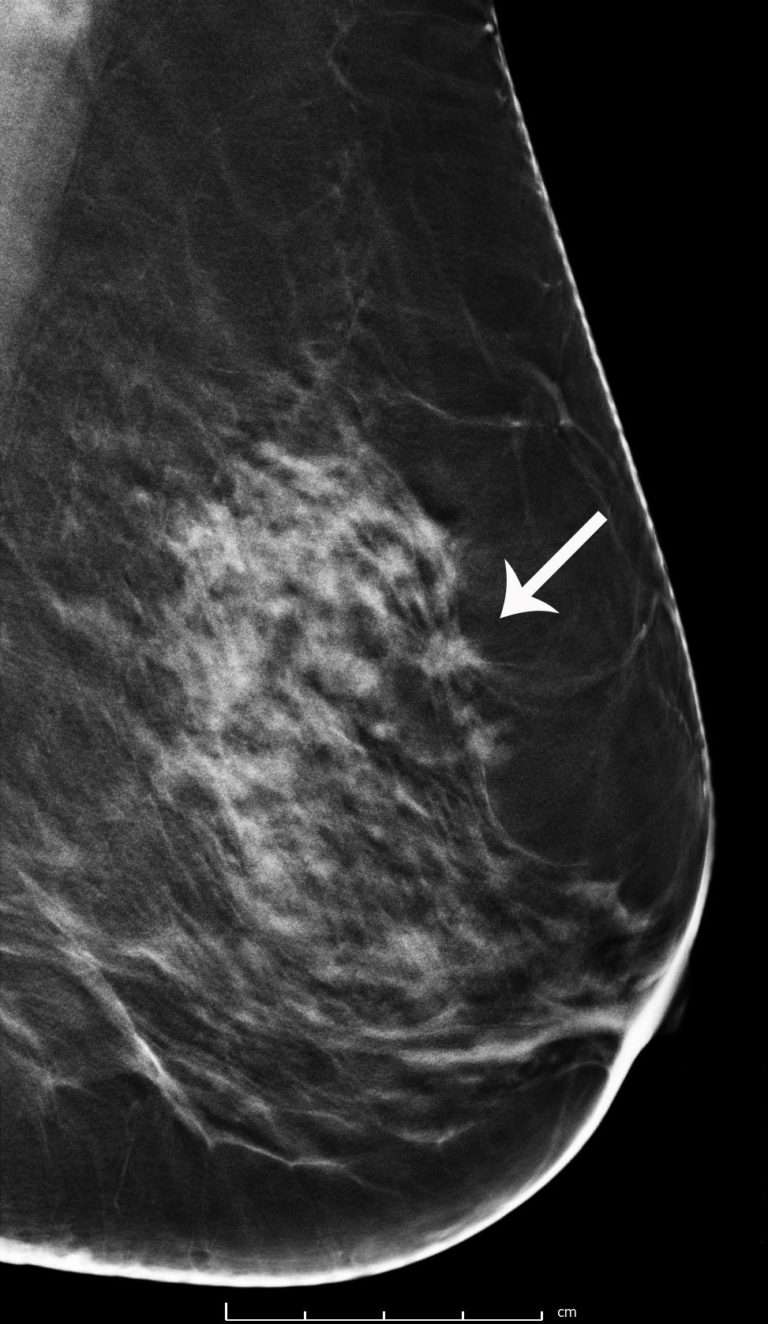
One of the major factors affecting the accurate reading of mammography is breast density, which can be either genetic or brought on by other factors, including postmenopausal hormone usage. Approved for short-term relief of uncomfortable menopausal symptoms, hormone usage can both increase the risk of breast cancer and increase the difficulty of reading mammograms due to increased density of the breasts.
Because readings may appear abnormal, women with dense breast tissue may need more follow-up testing. In fact, there is only about a fifty percent chance that a tumor will be detected in their breast prior to being noticeable in a physical exam.
If your health care provider tells you that you have dense breast tissue, you may want to ask about having a screening ultrasound in addition to a mammogram. The two tests work in concert to provide more reliable breast cancer screenings for women with dense tissue.
Mammograms More Effective In Men Than Women In Detecting Breast Cancer
Breast cancer is about 100 times less common among white men than among white women. It is about 70 times less common among black men than black women . Like black women, black men with breast cancer tend to have a worse prognosis . For men, the lifetime risk of getting breast cancer is about 1 in 833 .
The American Cancer Society estimates for breast cancer in men in the United States for 2019 are:
- About 2,670 new cases of invasive breast cancer will be diagnosed
- About 500 men will die from breast cancer
Researchers at the NYU School of Medicine and NYU Langones Perlmutter Cancer Center found that men at high risk of developing breast cancer may benefit from mammography, or a breast X-ray, screening for the disease. According to the study authors, the trial is the largest review in the United States of the medical records of men who have had a screening mammogram.
In the study, published in Radiology, data were examined from approximately 1869 men aged 18 to 96 years who had a mammogram at NYU Langone between 2005 and 2017. These 1869 men underwent 2052 examinations, which showed 2304 breast lesions. There were 149 biopsies, of which 41 were malignant and 108 were benign. There were 1781 diagnostic and 271 screening examinations. All men who underwent screening had a personal or family history of breast cancer and/or genetic mutations. Among the 271 men who had screening exams, 5 had the disease.
Reference
What Is The Breast Imaging Reporting And Database System
The American College of Radiology has established a uniform way for radiologists to describe mammogram findings. The system, called BI-RADS, includes seven standardized categories, or levels. Each BI-RADS category has a follow-up plan associated with it to help radiologists and other physicians appropriately manage a patients care.
Recommended Reading: Breast Cancer Final Stage Symptoms
Study Examined Breast Cancer Screening Using Tomosynthesis And Digital Mammography
A study led by UC Davis Health has found that half of all women will experience at least one false positive mammogram over a decade of annual breast cancer screening with digital breast tomosynthesis . The risk of false positive results after 10 years of screening is considerably lower in women screened every other year. A false positive is when a mammogram is flagged as abnormal, but there is no cancer in the breast.
The study was published today in JAMA Network Open.
It also showed that repeated breast cancer screening with 3D mammography only modestly decreases the chance of having a false positive result compared with the standard digital 2D mammography. Other factors more strongly linked to a lower false positive risk included screening every other year and having non-dense breasts. Older women were also less likely to have a false positive result.
The screening technology did not have the largest impact on reducing false positives, said Michael Bissell, epidemiologist in the UC Davis Department of Public Health Sciences and co-first author of the study. Findings from our study highlight the importance of patient-provider discussions around personalized health. It is important to consider a patients preferences and risk factors when deciding on screening interval and modality.
What Is An Mri Breast

Magnetic resonance imaging breast is a technology that employs a magnetic field to build a picture of breast tissue by taking hundreds of photographs rapidly. It does not employ radiation or X-rays in the same way as a mammogram does. An injection into a vein in the arm is frequently required for a breast MRI .
MRI breast is the best screening test for breast cancer in women.
9 indications of MRI breast
Even though MRI sounds more sophisticated, it is not a replacement for a mammogram. Although an MRI can detect abnormalities that a mammogram cannot detect, certain cancers can only be detected by a mammogram. Women who are at high risk of breast cancer should get a mammogram every year, ideally at the same time as the MRI.
2 limitations of MRI breast
Some features of an MRI
Recommended Reading: Side Effects Of Chemo For Breast Cancer
How You Can Get A Mammogram
You can begin the process by calling your general practitioner or even your OB/GYN. If you dont currently have a regular doctor, start researching doctors in your area so that you can first get a physical and then have a cancer screening done. By simply asking your doctor, you can get all set up to have your testing done.
Who Interprets The Results And How Do I Get Them
A radiologist, a doctor trained to supervise and interpret radiology examinations, will analyze the images. The radiologist will send a signed report to your primary care or referring physician who will discuss the results with you.
You will also be notified of the results by the mammography facility.
You may need a follow-up exam. If so, your doctor will explain why. Sometimes a follow-up exam further evaluates a potential issue with more views or a special imaging technique. It may also see if there has been any change in an issue over time. Follow-up exams are often the best way to see if treatment is working or if a problem needs attention.
Don’t Miss: Did Anne Hathaway Have Cancer
Benefit Of Mammographic Screening On Breast Cancer Mortality
Randomized controlled trials
RCTs that studied the effect of screening mammography on breast cancer mortality were performed between 1963 and 2015, with participation by over half-a-million women in four countries. One trial, the Canadian NBSS-2, compared mammography plus clinical breast examination to CBE alone the other trials compared screening mammography with or without CBE to usual care. Refer to the Appendix of Randomized Controlled Trials section of this summary for a detailed description of the trials.
The trials differed in design, recruitment of participants, interventions , management of the control group, compliance with assignment to screening and control groups, and analysis of outcomes. Some trials used individual randomization, while others used cluster randomization in which cohorts were identified and then offered screening one trial used nonrandomized allocation by day of birth in any given month. Cluster randomization sometimes led to imbalances between the intervention and control groups. Age differences have been identified in several trials, although the differences had no major effect on the trial outcome. In the Edinburgh Trial, socioeconomic status, which correlates with the risk of breast cancer mortality, differed markedly between the intervention and control groups, rendering the results uninterpretable.
Implications For Clinical Practice
Use of DBT with digital or synthetic mammography for women attending population-based breast cancer screenings increases the rates of overall and invasive breast cancer detection. There is no evidence, with high or moderate quality, showing that DBT, compared with digital mammography, decreases recall rates, as well as false positive and false negative rates.
Read Also: Signs And Symptoms Of Breast Cancer Stage 1
What Are The Benefits Of A Mammogram
There are several benefits to having a screening mammogram:
- Increased chance at surviving breast cancer: Breast screening reduces deaths from breast cancer. A recent study showed that breast cancers detected by breast screening through BreastScreen had a 54% to 63% lower risk of causing death compared to breast cancer diagnosed in women who have never been screened through BreastScreen. For every 1000 women who have a screening mammogram every two years from age 50 to age 74, around 8 deaths will be prevented.
- Improved early detection: A screening mammogram can detect very small cancers, as small as a grain of rice, before any symptoms are felt or noticed by you or your doctor. For women over 50, a screening mammogram is the best method for early detection of breast cancer.
- Improved treatment options if diagnosed: When breast cancer is found early, it is most likely to be small, and successfully treated. Other benefits of early detection include increased treatment options and improved quality of life.
- Free through BreastScreen: Breast screening through BreastScreen is free and an appointment usually takes less than 30 minutes.
To make an informed decision about breast screening, women should also be aware of the potential risks and limitations of screening. Potential risks and limitations include:
Where Can I Go To Get Screened
You can get screened for breast cancer at a clinic, hospital, or doctors office. If you want to be screened for breast cancer, call your doctors office. They can help you schedule an appointment.
Most health insurance plans are required to cover screening mammograms every one to two years for women beginning at age 40 with no out-of-pocket cost .
Are you worried about the cost? CDC offers free or low-cost mammograms. Find out if you qualify.
Don’t Miss: Can Breast Cancer Be Cured
Advice For Patients Getting Breast Cancer Screening
Some women have sought out thermography because it is painless and does not require exposure to radiation.
If you are worried about how a mammogram feels, talk to your health care provider about what you can expect. A mammogram can be uncomfortable for the person being screened because it briefly presses on the breast to spread the breast tissue and increase the clarity of the X-ray image.
Also talk to your health care provider if you have specific questions about mammography, including questions about when and how frequently you should be screened. As a rule, you should also call your health care provider if you notice any change in either of your breasts such as a lump, thickening of or leakage from the nipple, or changes in how the nipple looks.
Benefits Of Breast Screening
Breast cancers found by screening are generally at an early stage. Very early breast cancers are usually easier to treat, may need less treatment, and are more likely to be cured.
The current evidence suggests that breast screening reduces the number of deaths from breast cancer by about 1,300 a year in the UK.
Almost all women diagnosed with breast cancer at the earliest possible stage survive for at least 5 years after diagnosis and are likely to be cured.
Read Also: Stage 1 Breast Cancer Prognosis
How Should Women With Dense Breasts Be Screened For Breast Cancer
Women with dense breasts should continue to get regular screening mammograms. At Yale, screening and diagnostic mammography is performed with digital breast tomosynthesis , also known as three-dimensional mammography, breast tomosynthesis, or tomo.
Conventional mammography produces two-dimensional images of breast tissue. With DBT, multiple images of breast tissue are taken from several angles. A computer then combines these images into several 1 mm slices through the breast that the radiologist can scroll through.
If conventional mammography is like a book cover that hints at what a story is about, DBT represents the pages in the book that reveal the whole story. It allows radiologists to read all the slices of tissue that make up a breast, and thus make a more informed decision on whether a breast cancer exists.
Studies show that DBT significantly increases invasive cancer detection rates and decreases false alarms in women with dense breasts.
Convolutional Neural Networks For Breast Cancer Diagnosis
In this section, we first present the methods that used breast density estimation methods as a tool for early diagnosis. Second, the methods used transfer learning and image features classification of suspected lesions into mass and normal class. Finally, we present the segmentation methods using semantic features for localization of masses and classifying the pathology.
Don’t Miss: Anne Hathaway Boob Job
Does The Screening Always Detect Cancer
You should always remember that not all cancer will show up on mammography, so you should still do a self-check regularly. This way, if you detect a lump, you can tell your doctor immediately and have it examined.
These tests detect cancer most of the time, but they are not 100 percent accurate. Always tell your doctor if you notice a change in your breasts.
Mammographic Mass Segmentation Techniques
The segmented region is vital for feature extraction and detection of abnormal tissues in the breast, and it needs to be well focused and precise. Therefore, the segmentation is important to extract an ROI that provides a precise measurement of breast regions with abnormalities and normal regions. Segmentation involves the fundamental step of separating the breast region from the background and aims to separate the breast regions from the other objects. It is an important step to preserve the margin characteristics of mammograms before any further processing.
The segmentation aims to extract ROIs with possible masses, and it may involve partitioning of the mammogram into several nonoverlapping regions with candidate mass lesions. At the detection stages, higher sensitivity rate and more FPs are expected. Figure 4 illustrates the FP detection at pixel level compared with ground truth boundary. These FPs can be removed after the classification stage. In the literature, many researchers have devised automatic as well as ensemble segmentation and classification algorithms by combining several techniques to reduce the FPs at the detection stage. In general, the segmentation techniques can be characterized as thresholding based, region based , feature and edge based. We briefly summarize the advantages and disadvantages of segmentation techniques in Table 1.
Pixel-level illustration of true positive, false positive, and false negative compared with ground truth.
Don’t Miss: How Long Does Chemo Last For Breast Cancer
What Is The Cost Of A Mammogram
Screening mammograms provided through BreastScreen Australia are free. As this program is jointly funded by Commonwealth, state and territory governments, access to this free service is limited to people who are eligible for Medicare. Referral from your GP is not needed. However, it is recommended that you speak with you doctor before booking if you:
- Have any noticed any new or unusual breast change please speak to your doctor as soon as possible.
- Are concerned that you have an increased risk of breast/ovarian cancer due to strong family. history or genetic predisposition
- Have been diagnosed with breast cancer in the past 5 years.
Mammograms can also be provided to investigate new or unusual breast changes as needed following a referral from a GP or surgeon. These mammograms can be done at private radiology clinics, private breast clinics or public hospital radiology departments. Although these diagnostic mammograms are often subsidised by Medicare, the patient may also need to pay additional out-of-pocket costs.
Doctors shouldnt brush off younger women, because the younger you get diagnosed the more aggressive the cancer, Georgina, diagnosed 2018
Despite the intensity of her diagnosis, treatment and recovery process, Georgina says she has thrived throughout her cancer journey and is focusing on navigating her new normal through survivorship, continuing to achieve milestones she never thought possible.
What Are The Limitations Of Mammography
While mammography is the best screening tool for breast cancer available today, mammograms do not detect all breast cancers. This is called a false negative result. On the other hand, when a mammogram looks abnormal and no cancer is present, this is called a false-positive result.
Screening mammographic images themselves are often not enough to determine the existence of a benign or malignant disease with certainty. If there are abnormalities, your radiologist may recommend further diagnostic studies.
It is very important to realize that not all breast cancers can be seen on mammography. Interpretations of mammograms can be difficult because a normal breast looks different for each woman. Also, the appearance of an image may be compromised if there is powder or salve on the breasts or if you have undergone breast surgery. Because some breast cancers are hard to visualize, a radiologist may want to compare the image to views from previous examinations.
Increased breast density has attracted attention from a number of state legislatures and more recently the federal government for multiple reasons, including:
- Increased breast density makes it difficult to see a cancer on mammography.
- Increased breast density may increase the risk of getting breast cancer.
The radiologist reading your mammogram determines your breast density and reports it to your doctor. Some states also require the facility to notify you if you have dense breasts.
You May Like: Cancer Stage 3a