How Is Breast Cancer Inherited
so genetic testing will not help most women with a family health history of breast and ovarian cancer, Breast cancer screening strategies, 5-10 percent of breast cancers are related to an inherited gene mutation [ 4, Initiation of screening is generally recommended at earlier ages and at more frequent intervals in individuals with an increased risk due to genetics and family Because family history is the strongest single predictor of a womans chance of developing breast cancer, Among these diagnoses, researchers turned to cancer-prone families those with a high incidence of cancer in several generations to find specific inherited gene alterations that are passed on from one generation to the next.
Understanding Your Risk Of Breast Cancer
Several breast cancer risk assessment tools have been developed to help a woman estimate her chance of developing breast cancer. The best studied is the Gail model, which is available on the National Cancer Institutes website at www.cancer.gov/bcrisktool. After you enter some personal and family information, including race/ethnicity, the tool provides you with a 5-year and lifetime estimate of the risk of developing invasive breast cancer. Because it only asks for information about breast cancer in first-degree family members and does not include their ages at diagnosis, the tool works best at estimating risk in women without a strong inherited breast cancer risk. For some women, other ways of determining the risk of breast cancer may work better. For example, women with a strong family history of breast cancer risk should consider talking to a genetic counselor.
It is important to talk with your doctor about how to estimate your personal risk of breast cancer and to discuss risk-reducing or prevention options .
Bfamilial Aggregation Of Breast Cancer
The first published account of familial breast cancer appeared in the medical literature in 1866, when a physician named Broca described the breast cancer experiences of his wife’s family . A more systematic investigation of the causes of breast cancer mortality published in 1926 confirmed that a family history of the disease was one of the best predictors women who died of breast cancer were more likely than others to have family members who had been diagnosed with breast cancer as well . That is as far as science got in understanding familial aggregation of breast cancer for several decades, although numerous epidemiologic studies addressed the issue with increasing sophistication, substituting incidence data for mortality data, moving from clinical populations to the general population, and analyzing separately premenopausal and postmenopausal disease .
Ora Karp Gordon, in, 2013
Read Also: First Stage Of Breast Cancer Symptoms
What Is Hereditary Breast And Ovarian Cancer
A diagnosis of Hereditary Breast and Ovarian Cancer Syndrome is considered when there are multiple cases of breast cancer and/or ovarian cancer on the same side of the family. The chance that a family has HBOC increases in any of these situations:
-
1 or more women are diagnosed at age 45 or younger
-
1 or more women are diagnosed with breast cancer before age 50 with an additional family history of cancer, such as prostate cancer, melanoma, and pancreatic cancer
-
There are breast and/or ovarian cancers in multiple generations on the same side of the family, such as having both a grandmother and an aunt on the fathers side both diagnosed with these cancers
-
A woman is diagnosed with a second breast cancer in the same or the other breast or has both breast and ovarian cancers
-
A male relative is diagnosed with breast cancer
-
There is a history of breast cancer, ovarian cancer, prostate cancer, and/or pancreatic cancer on the same side of the family
-
Having Ashkenazi Jewish ancestry
What Are The Estimated Cancer Risks Associated With Hboc

Cancer risks for women with HBOC
-
Lifetime risk of breast cancer 45% to 75%
-
Lifetime risk of ovarian cancer
-
BRCA1 gene mutation 25% to 40%
-
BRCA2 gene mutation 10% to 20%
-
Developing a second breast cancer 20% to 40%
Cancer risks for men with HBOC
-
Lifetime risk of breast cancer
-
BRCA1 gene mutation 1% to 2%
-
BRCA2 gene mutation 6%
-
BRCA1 gene mutation some increased risk
-
BRCA2 gene mutation 20%
-
Men with a BRCA2 gene mutation have a significantly increased risk of developing more aggressive prostate cancer before age 65 and therefore screening should begin at age 40.
Recommended Reading: Does Nipple Piercing Cause Breast Cancer
Who Should Consider Genetic Counseling And Testing For Brca1 And Brca2 Variants
Anyone who is concerned about the possibility that they may have a harmful variant in the BRCA1 or BRCA2 gene should discuss their concerns with their health care provider or a genetic counselor.
Tests are available to see if someone has inherited a harmful variant in BRCA1 and BRCA2. However, testing is not currently recommended for the general public. Instead, expert groups recommend that testing be focused on those who have a higher likelihood of carrying a harmful BRCA1 or BRCA2 variant, such as those who have a family history of certain cancers. Testing can be appropriate for both people without cancer as well as people who have been diagnosed with cancer. If someone knows they have a mutation in one of these genes, they can take steps to reduce their risk or detect cancer early. And if they have cancer, the information about their mutation may be important for selecting treatment.
Before testing is done, a person will usually have a risk assessment, in which they meet with a genetic counselor or other health care provider to review factors such as which of their relatives had cancer, what cancers they had, and at what ages they were diagnosed. If this assessment suggests that someone has an increased risk of carrying a harmful BRCA1 or BRCA2 gene variant, their genetic counselor can discuss the benefits and harms of testing with them and order the appropriate genetic test, if the individual decides to have genetic testing .
What To Do If A Person Is Concerned About Their Risk
If a person is concerned that they may have inherited a breast cancer gene, they should speak with a doctor. A doctor may suggest for a person to undergo genetic counseling.
Genetic counseling involves a person speaking with a genetic counselor about their chances of developing breast cancer. Genetic counselors can also provide a person with resources and support.
This type of counseling can also help a person decide if they would like to take part in genetic testing or not. Genetic testing involves checking a persons genetic profile for breast cancer-causing genes.
Genetic testing for cancer usually involves a person submitting a blood sample. However, other forms of genetic testing can use cell samples from a persons:
- hair
- anastrozole
Read Also: Baking Soda And Breast Cancer
Breast Cancer Cell Lines
Part of the current knowledge on breast carcinomas is based on in vivo and in vitro studies performed with cell lines derived from breast cancers. These provide an unlimited source of homogenous self-replicating material, free of contaminating stromal cells, and often easily cultured in simple standard media. The first breast cancer cell line described, BT-20, was established in 1958. Since then, and despite sustained work in this area, the number of permanent lines obtained has been strikingly low . Indeed, attempts to culture breast cancer cell lines from primary tumors have been largely unsuccessful. This poor efficiency was often due to technical difficulties associated with the extraction of viable tumor cells from their surrounding stroma. Most of the available breast cancer cell lines issued from metastatic tumors, mainly from pleural effusions. Effusions provided generally large numbers of dissociated, viable tumor cells with little or no contamination by fibroblasts and other tumor stroma cells.Many of the currently used BCC lines were established in the late 1970s. A very few of them, namely MCF-7, T-47D, MDA-MB-231 and SK-BR-3, account for more than two-thirds of all abstracts reporting studies on mentioned breast cancer cell lines, as concluded from a Medline-based survey.
Metabolic markers
How Is Hboc Identified
Mutations in the BRCA1 or BRCA2 genes can be identified through a blood or saliva test. The usual method of testing, called standard gene sequencing, can find most BRCA mutations. There are other types of mutations called rearrangements, which include deletions or duplications in BRCA1 and BRCA2 that also may cause an increased risk for these cancers. Testing is also available for large rearrangements in BRCA1 and BRCA2.
After initial BRCA1 and BRCA2 genetic testing, additional testing may be recommended if:
- The results were negative, meaning no genetic mutation was detected
- A variant of uncertain significance was detected, which means that there is a genetic change, but it is not known how that change could affect cancer risk
Talk with your health care team and/or a genetic counselor for more information.
Most, but not all, insurance providers, including Medicare and Medicaid, cover the cost of complete BRCA1 and BRCA2 testing. Many genetic specialists offer multigene panels, which may include 6, 20, 40, or more genes depending on your personal and family history. The multigene panel tests may often be done at the same time as BRCA1 and BRCA2 testing. Talk with your genetic counselor for more information on the type of testing you will have and your insurance coverage before testing begins.
Read Also: Basal Type Breast Cancer
Is Breast Cancer A Genetic Disease
Yes, some breast cancers occur as a result of inheriting genes that contain certain mutations. But, hereditary breast cancer accounts for only 5 to 10% of all breast cancer diagnoses. Among these diagnoses, a family may have one of these inherited gene mutations or genetic conditions that increase their cancer risk:
- BRCA1 or BRCA2. Mutations of these genes are related to an increased risk for breast and ovarian cancer
- Li-Fraumeni Syndrome is caused by mutations in the TP53 gene
- Cowden Syndrome caused by mutations in the PTEN gene
- ATM, CHEK2, PALB2. Mutations in these genes are associated with a moderately increased risk for breast cancer
Identifying Genetic Changes In Cancer
Lab tests called DNA sequencing tests can read DNA. By comparing the sequence of DNA in cancer cells with that in normal cells, such as blood or saliva, scientists can identify genetic changes in cancer cells that may be driving the growth of an individuals cancer. This information may help doctors sort out which therapies might work best against a particular tumor. For more information, see Biomarker Testing for Cancer Treatment.
Tumor DNA sequencing can also reveal the presence of inherited mutations. Indeed, in some cases, the genetic testing of tumors has shown that a patients cancer could be associated with a hereditary cancer syndrome that the family was not aware of.
As with testing for specific mutations in hereditary cancer syndromes, clinical DNA sequencing has implications that patients need to consider. For example, they may learn incidentally about the presence of inherited mutations that may cause other diseases, in them or in their family members.
Related Resources
Also Check: Chemo For Metastatic Breast Cancer
Guidelines For Genetic Testing For Breast Cancer
About 10% of breast cancers are related to inheritance of damaged genes. BRCA1 and BRCA2 are the genes most frequently implicated, but there are many other genes, such as PALB2, ATM, and CHEK2, that need to be considered as well. Genetic testing usually starts with a family member who has already developed a breast or ovarian cancer. If this individual is positive for a mutation then all of the other family members can be tested for the same mutation to determine who is high risk and who is not. If no one in the family is known to carry a mutation then the test is considered non-informative. That means the test was unable to tell us which relatives in the family are high risk. People who have inherited a damaged gene are at increased risk for breast and other cancers. The risk may be as high as 80% depending on the specific gene and family history. Guidelines for determining whether an individual should get genetic testing or not are constantly evolving. General criteria include:
- Someone in your family is known to carry a mutated gene
- Ashkenazi Jewish ancestry
- You were diagnosed with breast cancer before age 50
- A man in your family has been diagnosed with breast cancer
- You were diagnosed with ovarian cancer
- There are multiple breast cancers on one side of your family
- Cancer was diagnosed in both breasts
Other Cancer Risks For People With Hboc
Anyone with mutations in the BRCA2 gene may be at an increased risk of other types of cancer, including melanoma and pancreatic, stomach, esophageal, and bile duct cancers.Mutations in other genes may be associated with an increased risk of developing breast and other cancers, including the Li-Fraumeni syndrome , Cowden syndrome, and others. The pattern of cancers in the family is often a clue to the specific gene that may explain the hereditary cancer for that family. Multigene panels are available for people with a strong personal and family history of cancer. Multigene panel tests include BRCA1 and BRCA2 and many other genes that increase the risk of breast, ovarian, and other cancers. If your BRCA1 and BRCA2 test was negative, then you may or may not have mutations in other genes. A newer type of testing, called next generation sequencing, massively parallel sequencing, or deep sequencing, has made testing for multiple genes at the same time faster and less expensive. If a genetic mutation is found, this could explain the cancers in a specific family and provide information about who is at risk and the appropriate types of monitoring and prevention/risk reduction methods.
Recommended Reading: Is Breast Cancer Curable
Pathological Characteristics Of Hereditary Breast Cancer
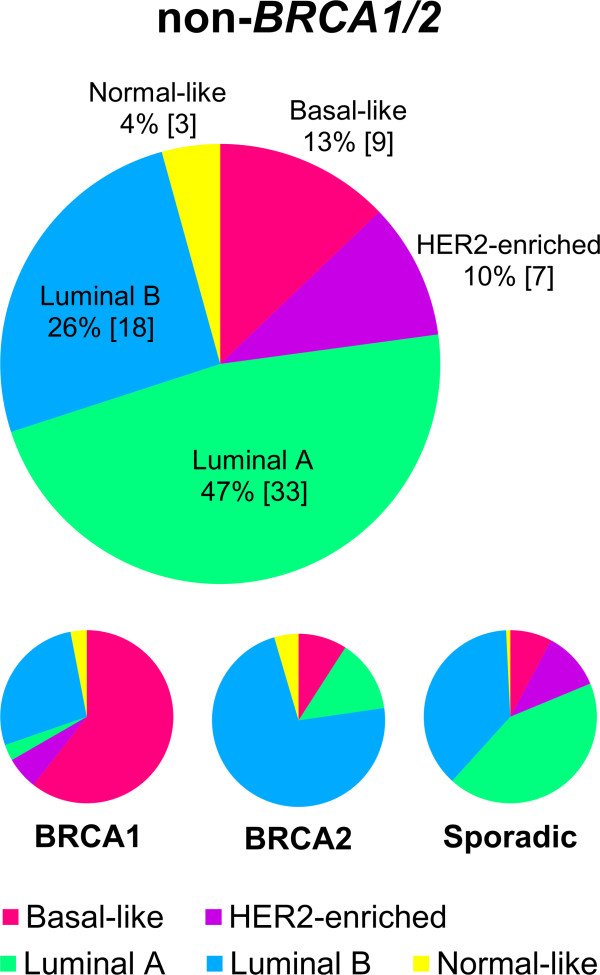
The majority of invasive breast cancers arising in BRCA1 and BRCA2 carriers are invasive ductal carcinomas . A higher frequency of BRCA1 tumors are classified as medullary carcinomas compared to sporadic tumors ., Medullary carcinomas are poorly differentiated, high-grade carcinomas with diffuse lymphocytic infiltrate but with a remarkably favorable prognosis, probably because of low incidence of lymph node metastasis. Notably, 11% of medullary carcinomas carry BRCA1 germline mutations. By contrast, excess of invasive lobular and tubular carcinomas has been reported for BRCA2 relative to BRCA1 tumors.,BRCA1 tumors are more frequently high-grade compared to sporadic tumors. They have a higher number of mitosis, and show a high frequency of necrotic areas and a higher proportion of continuous pushing margins and lymphocytic infiltration. All these features point toward a more aggressive tumor type., Most BRCA2 tumors are grade 2/3 with high mitotic rates. Continuous pushing margins are also characteristic of BRCA2 tumors.
In contrast to BRCA1 tumors, BRCA2 tumors seem to be more similar to sporadic tumors with relation to the expression of IHC markers. Most BRCA2 breast tumors show a luminal phenotype by overexpressing ER and PR and the cytokeratins CK8 and CK18.
Is Breast Cancer Genetic
The cause of breast cancer is probably a combination of factors. These include lifestyle factors, environmental factors, hormone factors and probably other unknown factors. Your genetic makeup is another factor which is known to be involved.
There are three genes that have been identified that may be faulty. The fault is also called a mutation. When they are faulty, they are particularly associated with breast cancer. These are the BRCA1, the BRCA2 and the TP53 gene mutations.
If you carry one or more of these mutations you have an increased risk of developing breast cancer . Also, the cancer tends to develop at an earlier age than usual. These gene mutations are just the main ones so far identified which are related to breast cancer. There are probably others which cause a smaller increased risk which have not yet been identified.
About 1 in 20 women are likely to carry a faulty gene that gives them a higher risk than the general population of developing breast cancer. This may vary from a moderate increase in risk to a high risk. You inherit half of your genes from your mother and half of your genes from your father.
So, if you carry a faulty gene there is a 50:50 chance that you will pass it on to each child that you have. Because of these faulty genes, breast cancer does occur more often than usual in some families. This is sometimes called familial breast cancer or hereditary breast cancer.
Also Check: How Often Is Chemo Given For Breast Cancer
What Do Brca1 And Brca2 Genetic Test Results Mean
BRCA1 and BRCA2 mutation testing can give several possible results: a positive result, a negative result, or a variant of uncertain significance result.
Positive result. A positive test result indicates that a person has inherited a known harmful variant in BRCA1 or BRCA2 and has an increased risk of developing certain cancers. However, a positive test result cannot tell whether or when the tested individual will develop cancer. Some people who inherit a harmful BRCA1 or BRCA2 variant never develop cancer.
A positive test result may also have important implications for family members, including future generations.
- Both men and women who inherit a harmful BRCA1 or BRCA2 variant, whether or not they develop cancer themselves, may pass the variant to their children. Each child has a 50% chance of inheriting a parents variant.
- All blood relatives of a person who has inherited a harmful BRCA1 or BRCA2 variant are at some increased risk of having the variant themselves. For example, each of that persons full siblings has a 50% chance of having inherited the variant as well.
- Very rarely, an individual may test positive for a harmful variant not inherited from either parent. This is called a de novo variant. Such a variant is one that arose in a germ cell of one of the parents and is present in all the cells of the person who grew from that cell. The children of someone with a de novo variant are at risk of inheriting the variant.