Thingsthat Stop The Body From Making Essentials Hormones
Whiletalking about hormone therapy for breast cancer your doctor may suggest aromatizingmedicines that can reduce the amount of estrogen in your body. Thesemedications are useful according to medical experts as it is also mentioned on mayo clinic websites you can read there.
Thesemedications are useful for those who undergo menopause symptoms or surgery to prevent estrogen that helping cancer cells to grow.
Youshould know all about hormone therapy before using them for breast cancertreatment. Holistic approaches are most useful for treating them without anysurgery or hormone pills. This system is scientific and tested for breastcancer to uterine cancer treatment without any surgery.
Ovary removal is another condition when your doctor will suggest you use aromatizeinhibitors to use but you should use power hormone for them because they helpyou surgery-free treatment for those types of women health-related issues.
It Will Also Be Important In The Future To Differentiate Prior To Treatment Patients Who Are At High Risk Of Relapse From Those At Lower Risk In Order To Tailor Hormone Treatment This May Be Done To Avoid Escalation Of Anti
The CANTO cohort comprises 12,000 women with breast cancer treated in 26 French centres. It is sponsored by Unicancer and directed by Professor Fabrice André, specialist breast cancer oncologist at Gustave Roussy, Inserm research director and responsible of the lab Predictive Biomarkers and Novel Therapeutic Strategies in Oncology . Its objective is to describe adverse effects associated with treatment, to identify the populations at risk of developing them and to adjust therapy accordingly, so as to afford a better quality of life following cancer.
Watch the video on YouTube :
J Clin Oncol. 2019 Feb 10 37:423-438 : https://doi.org/10.1200/JCO.18.01160
TO CITE THIS POST :
1INSERM Unit 981, Gustave Roussy, Cancer Campus, Villejuif, France
2Breast Unit, Champalimaud Clinical Center, Champalimaud Foundation, Lisbon, Portugal
3Medical Oncology, Gustave Roussy, Cancer Campus, Villejuif
4Department of Supportive Care, Gustave Roussy, Cancer Campus, Villejuif
5Medical Oncology, Centre François Baclesse Caen, Caen
6Unicancer, Paris, France
7Department of Medical Oncology, U.O.C. Clinica di Oncologia Medica, IRCCS Ospedale Policlinico San Martino, Genova
8Department of Internal Medicine and Medical Specialties , School of Medicine, University of Genova, Genova, Italy
9Surgical Oncology, Centre Georges-François Leclerc, Dijon
10Medical Oncology, Institut Curie, Paris
14Surgical Oncology, C.R.L.C Val dAurelle, Montpellier
Rationale For Neoadjuvant Therapy: The Nsabp B
The NSABP B-18 trial was designed to determine whether preoperative treatment with four cycles of doxorubicin/cyclophosphamide would improve overall survival and DFS when compared with the same treatment given postoperatively. At 9 years of follow-up, there was no difference in survival or DFS between the two groups,. A critical observation during this follow-up was that pCR correlated with OS, and this finding became stronger with longer follow up. Primary tumor response graded as pCR, pINV , clinical partial response , or clinical non-responder and was associated with outcome measures of OS , DFS , and RFS . The B-18 trial established that chemotherapy can be given before surgery with no loss of efficacy, opening the way to measuring chemotherapy effect and the testing of novel agents, as in the B-27 trial.
Don’t Miss: Grade 3 Invasive Ductal Carcinoma
How Is Hormone Therapy Used To Treat Breast Cancer
There are three main ways that hormone therapy is used to treat hormone-sensitive breast cancer:
Adjuvant therapy for early-stage breast cancer:Tamoxifen is FDA approved for adjuvant hormone treatment of premenopausal and postmenopausal women with ER-positive early-stage breast cancer, and the aromatase inhibitorsanastrozole, letrozole, and exemestane are approved for this use in postmenopausal women.
Research has shown that women who receive at least 5 years of adjuvant therapy with tamoxifen after having surgery for early-stage ER-positive breast cancer have reduced risks of breast cancer recurrence, including a new breast cancer in the other breast, and reduced risk of death at 15 years .
Until recently, most women who received adjuvant hormone therapy to reduce the chance of a breast cancer recurrence took tamoxifen every day for 5 years. However, with the introduction of newer hormone therapies , some of which have been compared with tamoxifen in clinical trials, additional approaches to hormone therapy have become common .
Some premenopausal women with early-stage ER-positive breast cancer may have ovarian suppression plus an aromatase inhibitor, which was found to have higher rates of freedom from recurrence than ovarian suppression plus tamoxifen or tamoxifen alone .
Men with early-stage ER-positive breast cancer who receive adjuvant therapy are usually treated first with tamoxifen. Those treated with an aromatase inhibitor usually also take a GnRH agonist.
How And When To Take Letrozole
Letrozole comes as 2.5mg tablets. The usual dose is 1 tablet, taken once a day.
Try to take your letrozole at the same time each day. You can choose a time that suits your everyday routine. This will make it easier to remember to take your medicine.
Swallow the tablet whole with a drink of water. Do not crush or chew it. You can take letrozole with or without food.
You May Like: Stage 3 Ductal Carcinoma Prognosis
What If I Forget To Take It
If you forget a dose take it as soon as you remember, unless your next dose is due in 2 or 3 hours. In this case skip the missed dose and take your next one at the usual time.
Do not take a double dose to make up for a forgotten dose.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice about other ways to help you remember to take your medicine.
Progesterone Receptor Positive Breast Cancer
On the other hand, a PR-positive breast cancer is induced by cells that are more responsive to progesterone. Progesterone is a steroid hormone found in the ovaries and it is essential in the development of breasts during puberty. It also assists in preparing the body for lactation and breastfeeding. It also shows symptoms that are similar to the ER-positive cancer type.
Don’t Miss: Baking Soda Honey Cancer
Can Hormonal Therapy Reduce The Risk Of Developing Breast Cancer
Drugs that block the effects of estrogen have been shown to reduce the risk of breast cancer in women at high risk of the disease. Two drugs that have been approved for breast cancer risk reduction in certain groups of women are tamoxifen and Evista® . Tamoxifen is approved for breast cancer risk reduction in women who are at high risk of the disease . Evista originally approved for the prevention and treatment of osteoporosis is approved for breast cancer risk reduction in postmenopausal women with osteoporosis or postmenopausal women at high risk of breast cancer.
To directly compare Evista to tamoxifen in the prevention of breast cancer in high-risk women, researchers conducted a clinical trial known to as the STAR trial .24 The study found that Evista is as effective as tamoxifen in reducing the risk of invasive breast cancer in high-risk postmenopausal women, but may be less effective in reducing the risk of noninvasive breast cancers such as ductal carcinoma in situ . Evista carried a lower risk of blood clots and cataracts than tamoxifen, but is not without side effects. Evista has been found to increase the risk of blood clots and fatal strokes in women with coronary heart disease or at risk for coronary heart disease.25
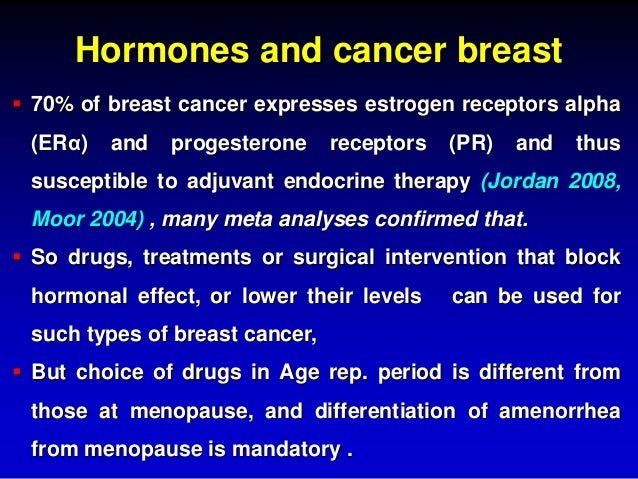
Hormones And Breast Cancer
The hormones estrogen and progesterone make some breast cancers grow. They are called hormone-sensitive breast cancers. Most breast cancers are sensitive to hormones.
Estrogen and progesterone are produced in the ovaries and other tissues such as fat and skin. After menopause, the ovaries stop producing these hormones. But the body continues to make a small amount.
Hormone therapy only works on hormone-sensitive cancers. To see if hormone therapy may work, doctors test a sample of the tumor that has been removed during surgery to see if the cancer might be sensitive to hormones.
Hormone therapy can work in two ways:
Don’t Miss: Stage 3 Her2 Positive Breast Cancer
When Are Hormone Blockers Used
Hormone inhibitors and blocker options may depend on a persons stage of life.
- Hormone inhibitors are only used in postmenopausal women. They can be given to premenopausal women if steps are taken by the treatment team to put the ovaries to sleep by blocking the ovaries from producing estrogen or progesterone.
- Hormonal therapy may also be called anti-hormone treatment. Think of it as the opposite of hormone replacement therapy . If pathology tests show that the tumor in your breast has hormone receptors , then hormonal therapy may be recommended for you after the completion of your acute treatment .
- Hormonal therapy keeps breast cancer cells from receiving or using the natural female hormones in your body which they need to grow. Hormonal therapy also blocks the ability of health breast cells to receive hormones that could stimulate breast cancer cells to regrow again in the form of recurrence of the breast cancer within the breast or elsewhere in the body.
When Should You Start Hormone Therapy
Women can take hormone therapy after receiving surgery to lessen the possibilities of breast cancer returning. This method is known as adjuvant therapy. It is also effective in destroying the cancerous cells that are left behind or to treat the cancer that has returned after the surgery.
Meanwhile, there are patients whod want to take preventative measures and start hormone therapy before surgery and this is known as neoadjuvant therapy. It usually works by shrinking the size of the cancer tumor and killing the cells that have already spread.
The first step to starting hormonal therapy is to consult with an oncologist or licensed HRT provider to determine the right treatment plan that will work for you. There are many factors that can affect the type of HRT medicine that will be recommended such as the cancer stage, menopausal status, medical history , and bone density.
The period of how long a woman stays on hormone replacement therapy depends on whether theyre taking it before or after surgery, and the stage of the cancer they have. For example, postmenopausal women with early stage cancer and are taking HRT after surgery can stay on the treatment for 5 years.
Don’t Miss: Breast Cancer Nodes
Side Effects Of Endocrine Therapy
Side effects of tamoxifen and OFS/OA mimic menopausal symptoms, including hot flashes, sweats, weight gain and sexual dysfunction, which may negatively impact quality of life. In addition, tamoxifen has both estrogen agonist and antagonist properties with different side effect profile depending on the target organ. Hot flashes are the most common side effect of tamoxifen, reported in up to 80% of women . Non-hormonal and non-pharmacological therapies such as phytotherapy or acupuncture can be effective to reduce the intensity of symptoms as well as low-dose antidepressants, pregabalin and gabapentin .
The estrogen-like effect of tamoxifen on the uterus may induce endometrial hyperplasia and endometrial tumors . In the most recent EBCTCG overview, 5 years of tamoxifen were associated with a low overall incidence of uterine cancer only in women aged 55 to 69 years, with no impact on mortality from uterine cancer . To date, no evidence-based recommendations for routine screening in women assuming tamoxifen were published. However, abnormal bleeding should be promptly investigated and expert opinion recommendations suggest annual gynecologic examinations .
As previously mentioned, in the 2011 EBCTCG meta-analysis women who received tamoxifen had an increased thrombo-embolic risk . Similar findings were reported in BC prevention trials . Tamoxifen is therefore contraindicated in women with prior history of deep-vein thrombosis and pulmonary embolism.
Prognosis Following The Use Of Complementary And Alternative Medicine In Women Diagnosed With Breast Cancer
This analysis, by Saquib et al, was a secondary analysis of the Womens Healthy Eating and Living study. It looked at 2562 breast cancer survivors and surveyed for rejection of systemic treatment and use of CAM following surgical resection. All women had to be aged 18-70 and had operable Stage I-IIIa breast cancer. In this group, 177 women were identified who declined systemic treatment. 80% of this group used CAM. Compared to women that took chemotherapy, women that declined systemic treatment had a 90% greater risk of an additional breast cancer event, and the risk of death increased by 70%. CAM use had no effect on this finding. In addition, the lack of effect was consistent between high supplement users and low supplement users. The authors concluded that women that decline systemic treatment are at greater risk for subsequent recurrence and death due to breast cancer. The use of CAM had no measurable effect on the recurrence of breast cancer or on the risk of subsequent death.
Don’t Miss: Is Invasive Breast Cancer Curable
Which Hormonal Therapy Medicine Will I Take
This will depend on many factors, including:
- your menopausal status
- your history, if any, of arthritis
- your personal risk of uterine and ovarian cancer
- any side effects you experience once you start taking a hormonal therapy
The American Society of Clinical Oncologists recommends hormonal therapy medicines based on cancer stage and menopausal status:
- Early-stage breast cancer and postmenopausal: ASCO recommends that postmenopausal women diagnosed with early-stage, hormone-receptor-positive breast cancer consider an aromatase inhibitor as the first hormonal therapy medicine. A woman who has taken tamoxifen for 2 to 3 years may want to consider switching to an aromatase inhibitor. Aromatase inhibitors are sometimes used beyond 5 years of tamoxifen to further reduce the risk of breast cancer recurrence.
- Early-stage breast cancer and premenopausal: ASCO recommends that premenopausal women diagnosed with early-stage hormone-receptor-positive breast cancer consider taking tamoxifen.
- Advanced breast cancer: ASCO recommends that women diagnosed with advanced hormone-receptor-positive breast cancer consider taking an aromatase inhibitor after 2 to 5 years of tamoxifen, or whenever the cancer stops responding to tamoxifen. If the cancer stops responding to an aromatase inhibitor and tamoxifen, consider Faslodex .
You Have More Power Than You Have Been Told
You have more power over your risk of breast cancer than you think. There are many steps you can take to protect yourself. Each one of them has other positive domino effects for your hormonal balance and overall health:
1. Help with Estrogen Metabolism
If theres one trio of supplements I recommend for preventing breast cancer and promoting overall hormone health, its the combination of DIM, sulforaphane, and calcium d-glucarate. Heres a breakdown of these major estrogen metabolizers.
DIM: Also known as diindolylmethane, DIM is a compound generated when the body breaks down cruciferous vegetables such as broccoli, cabbage, and cauliflower. It is best known as a nutrient that supports healthy estrogen metabolism as well as the prevention of hormone-related cancers by its anti-estrogenic and anti-androgenic effects. It supports:
- Phase 1 liver detoxification
- The breakdown of estrogen into clean estrogens, not the antagonistic dirty ones
- A healthy balance of testosterone and estrogen by acting as an aromatase inhibitor, blocking some testosterone from converting to estrogen
- The cells from the damaging effects of oxidation
I personally use and recommend our DIM. The recommended dose is 100 mg to 200 mg per day.
I personally use and recommend our Brocco Power . The recommended dosage is 500 mg a day.
I personally use and recommend our Calcium-D-Glucarate. Recommended dosage of calcium d-glucarate ranges from 150 mg to 300 mg per day, taken with meals.
For Breast Protection:
Also Check: What Is A Malignant Neoplasm Of Breast
Rationale For Neoadjuvant Therapy As A Standard Of Care For Patients With Triple
Notably, two randomized neoadjuvant trials of PD-L1 antibodies, NeoTRIPaPDL1 which tested atezolizumab and chemotherapy and GeparNuevo which tested durvalumab and chemotherapy in TNBC, did not show increase in pCR with addition of this PD-L1 antibody compared to placebo. The GeparNuevo trial did show a significant increase in pCR in a subset of patients who received a window of 2 weeks of durvalumab before beginning chemotherapy .
A further rationale for NAC for TNBC is that subsequent adjuvant therapy can be implemented with the goal of improving outcomes for patients who lack a pCR result. The CREATE-X and GEICAM trials tested these approaches .
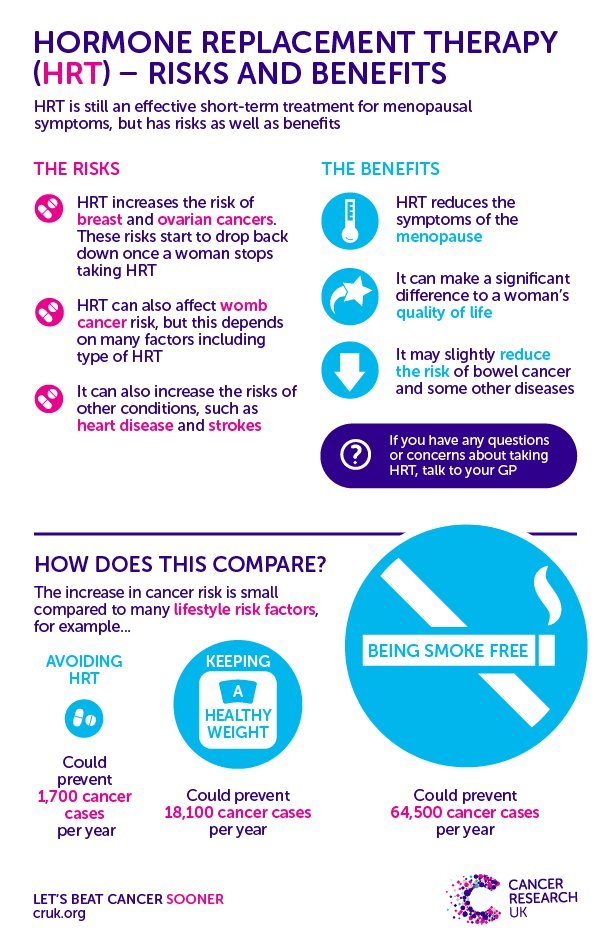
Benefits And Other Risks Of Hrt
Many women decide the benefits of taking HRT outweigh the risks.
While HRT increases breast cancer risk, it also helps to relieve many womens menopausal symptoms. It can also reduce a womans risk of developing osteoporosis in the short term and improve muscle strength.
It has some side effects such as headaches, feeling sick and breast tenderness. These usually happen in the first few months. Taking HRT also slightly increases the risk of having a blood clot or a stroke, and might slightly increase the risk of ovarian cancer.
Read Also: Her2 Stage 3 Breast Cancer
Treating Stage Iii Breast Cancer
In stage III breast cancer, the tumor is large or growing into nearby tissues , or the cancer has spread to many nearby lymph nodes.
If you have inflammatory breast cancer: Stage III cancers also include some inflammatory breast cancers that have not spread beyond nearby lymph nodes. These cancers are treated slightly different from other stage III breast cancers. You can find more details in Treatment of Inflammatory Breast Cancer.
There are two main approaches to treating stage III breast cancer:
Radiation May Be Better Than Anti
Researchers may have identified a treatment alternative for older women with low-risk forms of breast cancer. It could offer fewer adverse side effects than anti-hormonal drug therapies.
The study found slightly higher survival rates for women over 70 with hormone receptor-positive breast cancer and took anti-estrogen medications than those who were treated with a short dose of radiation. All of the patients had undergone a lumpectomy before these treatments, according to a new report published Monday in the International Journal of Radiation Oncology.
Radiation therapy costs $3,800 or more than anti-hormonal therapy over the average patient’s lifetime, the report found.
Still, researchers suggested radiation therapy could be a good alternative to anti-estrogen medications for some women because it could improve their quality of life without higher mortality risks.
“The reality is anti-hormone therapy is not easy to take long-term and doesn’t offer significantly greater benefits. It can dramatically impact quality of life.” said Dr. Frank Vicini, the report’s co-author and principal investigator at 21st Century Oncology, a Florida-based cancer care services operator of 165 centers across 15 states.
Anti-estrogen treatment may be necessary for five to ten years, according to current recommendations. Vicini said as many as 50% of patients who start anti-estrogen treatment had difficulty managing the side effects and end up stopping the treatment during that time.
Also Check: Breast Cancer Stage 3 Symptoms