Genomic Tests To Predict Recurrence Risk
Doctors use genomic tests to look for specific genes or proteins, which are substances made by the genes, that are found in or on cancer cells. These tests help doctors better understand the unique features of each patients breast cancer. Genomic tests can also help estimate the risk of the cancer coming back after treatment. Knowing this information helps doctors and patients make decisions about specific treatments and can help some patients avoid unwanted side effects from a treatment that may not be needed.
The genomic tests listed below can be done on a sample of the tumor that was already removed during biopsy or surgery. Most patients will not need an extra biopsy or more surgery for these tests.
For patients age 50 or younger
-
Recurrence score less than 16: Hormonal therapy is usually recommended, but chemotherapy is generally not needed
-
Recurrence score of 16 to 30: Chemotherapy may be recommended before hormonal therapy is given
-
Recurrence score of 31 or higher: Chemotherapy is usually recommended before hormonal therapy is given
For patients older than 50
The tests listed above have not been shown to be useful to predict risk of recurrence for people with HER2-positive or triple-negative breast cancer. Therefore, none of these tests are currently recommended for breast cancer that is HER2 positive or triple negative. Your doctor will use other factors to help recommend treatment options for you.
Response To Public Comment
A draft recommendation statement was posted for public comment on the USPSTF Web site from 21 April through 18 May 2015. In response to the comments received, the USPSTF clarified certain terminology , updated or added references , and provided additional context around the potential risks of radiation exposure due to mammography screening. Additional discussion of the public comments is below.
Benefits of Contemporary Screening Mammography
Screening Mammography in Women Aged 40 to 49 Years
Some commenters incorrectly believed that the C recommendation for women aged 40 to 49 years represented a change from what the USPSTF had recommended in the past. Others thought that the C recommendation meant that the USPSTF was recommending against screening in this group of women. As noted previously, the recommendation for women aged 40 to 49 years was also a C in 2009 . This update clarifies the language around what the C recommendation means. It is not a recommendation against screening but a statement that the decision to undergo screening mammography for women in their 40s should be an informed, individual one, after she weighs the potential benefit against the potential harms.
Screening Mammography in Women Aged 70 to 74 Years or Older
Definition of Overdiagnosis
DBT
Comparison of the USPSTFs Recommendations With Those of Other Organizations
Insurance Coverage and Access to Mammography
What Happens If Something Is Detected On My Screening Exam
Lumps, other abnormalities or questionable findings in the breast are often detected by screening tests. However, it is not always possible to tell from these imaging tests whether a finding is benign or cancerous. To determine whether there is a cancer present, your doctor may recommend that one or more of the following imaging tests may be performed:
- diagnostic mammography
- breast ultrasound
- breast MRI
If a finding is proven to be benign by its appearance on these exams, no further steps may need to be taken. If these tests do not clearly show that the finding is benign, a biopsy may be necessary. In a biopsy, a small amount of tissue is removed under local anesthesia so that it can be examined in a laboratory. One of the following image-guided procedures is used during a breast biopsy:
A pathologist examines the removed tissue specimen and makes a final diagnosis. Depending on the facility, the radiologist or your referring physician will share the results with you.
With early detection and improved treatments, more women are surviving breast cancer. If cancer is diagnosed, your doctor will discuss your treatment options and together you will determine your course of treatment. Today, women have more treatment options than ever before. For more information on treatment, see the Breast Cancer Treatment page.
Recommended Reading: Does Breast Cancer Make You Cough
Women At Higher Risk Of Breast Cancer
Factors that greatly increase breast cancer risk include :
- A BRCA1 or BRCA2 inherited gene mutation
- A personal history of invasive breast cancer or ductal carcinoma in situ
- A personal history of lobular carcinoma in situ or atypical hyperplasia
- Radiation treatment to the chest area between ages 10-30
- Li-Fraumeni, Cowden/PTEN or Bannayan-Riley-Ruvalcaba syndrome
- An ATM, BARD1, BRIP1, CDH1, CHEK2, NBN, NF1, PALB2, PTEN, RAD51C, RAD51D, STK11 or TP53 inherited gene mutation
- A greater than 20 percent lifetime risk of invasive breast cancer based mainly on family history
Figure 3.5 below outlines the National Comprehensive Cancer Network breast cancer screening guidelines for women at higher than average risk up to age 75.
The NCCN recommends women older than 75 talk with their health care providers about a breast cancer screening plan thats right for them.
Figure 3.6 below outlines the American Cancer Society breast cancer screening guidelines for women at higher than average risk .
|
Figure 3.5: NCCN breast cancer screening recommendations for women at higher than average risk |
|
Risk factor |
|
Every year starting at age 30 or age recommended by health care provider |
Every year starting at age 30 or age recommended by health care provider |
|
Adapted from ACS materials . |
Where Can I Go To Get Screened

You can get screened for breast cancer at a clinic, hospital, or doctors office. If you want to be screened for breast cancer, call your doctors office. They can help you schedule an appointment.
Most health insurance plans are required to cover screening mammograms every one to two years for women beginning at age 40 with no out-of-pocket cost .
Are you worried about the cost? CDC offers free or low-cost mammograms. Find out if you qualify.
Also Check: What Happens After Breast Cancer Surgery
Breast Cancer Screening Recommendations
The United States Preventive Services Task Forceexternal icon is an organization made up of doctors and disease experts who look at research on the best way to prevent diseases and make recommendations on how doctors can help patients avoid diseases or find them early.
The USPSTFexternal icon recommends that women who are 50 to 74 years old and are at average risk for breast cancer get a mammogram every two years. Women who are 40 to 49 years old should talk to their doctor or other health care professional about when to start and how often to get a mammogram. Women should weigh the benefits and risks of screening tests when deciding whether to begin getting mammograms before age 50.
Loesje Kessels Writes An Open Letter About Her Experience With Breast Cancer
Eleven years ago my sister got sick. A brain tumor with only given months to live. We went from being young and wild, traveling and partying, working hard to pursue our dreams to chemotherapies and daily radiation. She then had to undergo two brain surgeries. For seven and a half months I stayed with her nearly 24/7 in the hospital, during her treatments and we even slept in the same bed every night. It wasnt until that devastating night of July 14, 2011 when she peacefully passed away in my arms.
Moving forward in life without her was, and still is, a difficult task for my myself, my brother and most of all my parents. After this entire ordeal I felt, with every fibre in my body, that I never wanted to have anything to do with cancer again for the rest of my life. Of course, this was simple unrealistic.
But then there was me. This meant I had a 50% chance of carrying the BRCA gene too. The first two years I did not proceed with the genetic tests. Something about it being very expensive in Dubai but honestly, I think I was just not ready to hear it. The next two years saw many MRIs, mammograms, ultrasounds and blood tests. And every time I underwent any of these, I was reminded of my sister.
It has made me appreciate and love life more than I ever did before. I am determined to not let the big, bad C outshine my life and to make the most of every day be passionate, love hard, chase dreams, make unforgettable memories and have fun along the way.
Read Also: Does Breast Cancer Show In Blood Work
Your Genes Can Say A Lot About Your Riskbut They Dont Tell The Whole Story
While these gene mutations clearly play a critical role in breast cancer risk, its also important to know that only 5-10 percent of breast cancer cases are related to genetic history. Not having BRCA1 or BRCA2 gene mutations doesnt mean youre not at risk for breast cancer, and you still should talk with your health care professional about the right breast cancer screening for you.
Want to learn more about BRCA1 and BRCA2? Read this fact sheet from the National Cancer Institute. You can talk with your health care professional about whether this test makes sense for you.
For more information about breast cancer prevention and early detection, visit preventcancer.org/breast.
Breast Mri And Breast Cancer Screening
Breast MRI is not routinely used in breast cancer screening for most women. There are some downsides to breast MRI.
Breast MRI in combination with mammography is better than mammography alone at finding breast cancer in certain women at higher than average risk .
The NCCN recommends screening with mammography plus breast MRI for some women at higher risk of breast cancer, including those with :
- A first-degree relative with a BRCA1/2 gene mutation, but have not been tested for BRCA1/2 mutations themselves
- Radiation treatment to the chest area between ages 10-30
- Li-Fraumeni, Cowden/PTEN syndrome or Bannayan-Riley-Ruvalcaba syndrome
- A PALB2, PTEN or TP53 inherited gene mutation
- A greater than 20 percent lifetime risk of invasive breast cancer based mainly on family history
The NCCN recommends women with an ATM, BARD1, CDH1, CHEK2 or NF1 inherited gene mutation, consider breast MRI as part of their breast cancer screening .
Women at higher risk who are recommended breast MRI as part of breast cancer screening, but cannot have one for medical reasons, may consider breast ultrasound or contrast-enhanced mammography .
Talk with your provider about breast cancer screening. Together, you can make a screening plan thats right for you.
Learn about emerging research on breast cancer screening with breast MRI plus mammography in women at higher than average risk.
Recommended Reading: What Medications Are Used For Breast Cancer
How Can A Person Who Has Inherited A Harmful Brca1 Or Brca2 Gene Variant Reduce Their Risk Of Cancer
Several options are available for reducing cancer risk in individuals who have inherited a harmful BRCA1 or BRCA2 variant. These include enhanced screening, risk-reducing surgery , and chemoprevention.
Enhanced screening. Some women who test positive for harmful BRCA1 and BRCA2 variants may choose to start breast cancer screening at younger ages, have more frequent screening than is recommended for women with an average risk of breast cancer, or have screening with magnetic resonance imaging in addition to mammography.
No effective ovarian cancer screening methods are known. Some groups recommend transvaginal ultrasound, blood tests for the CA-125 antigen , and clinical examinations for ovarian cancer screening in women with harmful BRCA1 or BRCA2 variants. However, none of these methods appear to detect ovarian tumors at an early enough stage to improve long-term survival .
The benefits of screening men who carry harmful variants in BRCA1 or BRCA2 for breast and other cancers are not known. Some expert groups recommend that such men undergo regular annual clinical breast exams starting at age 35 . The National Comprehensive Cancer Network guidelines recommend that men with harmful germline variants in BRCA1 or BRCA2 consider having a discussion with their doctor about prostate-specific antigen testing for prostate cancer screening starting at age 40 .
Common Symptoms Of Male Breast Cancer What To Look Out For
The most common symptom of breast cancer in men is a firm lump in the breast tissue deep to the nipple. This is nearly always painless and other symptoms may include:
- Oozing from the nipple that may be blood stained.
- Swelling of the breast.
- A sore in the skin of the breast.
- A nipple that is pulled into the breast .
- Lumps under the arm.
If you are showing any of the common symptoms listed above, please call us on to book a OneStop Breast Clinic appointment.
Were pleased to cancel and re-schedule any appointments without penalty or administration fees up to 24 hours before your appointment. However, with less than 24 hours notice of cancellation, re-scheduling or non-attendance on the day does incur a 100% cancellation fee as well be unable to re-use the time to support other clients. New appointments will be charged at the self-pay rate of £250 .
Read Also: What Is The Survival Rate For Stage 0 Breast Cancer
You May Like: Can I Die From Breast Cancer
Guidelines For Elective Surgical Options
Women with BRCA1 or BRCA2 mutations face a significant risk of breast and ovarian cancer. Prophylactic removal of the fallopian tubes and ovaries is recommended by about age 40. Many women with BRCA1 or BRCA2 mutations will also elect to have their breasts removed. Nipple-sparing mastectomy is an effective option for these women.
Making the decision to have an elective preventive double mastectomy and removal of the ovaries is personal and should be based on many life factors. You must balance where you are in your childbearing years, what your future choices may be, and whether you would prefer to follow a rigorous screening schedule instead of making such a life-altering choice.
Whatever your decision, we encourage you to make an informed choice. If you do elect to have a preventive double mastectomy, our breast specialists will guide you in the appropriate breast surgery reconstruction to help restore your body image after treatment.
If you are interested in discussing ovary removal surgery , we will refer you to one of our gynecological oncologists.
Show me more…
What Is Breast Cancer
Breast cancer is a disease that attacks the tissue in one or both of your breasts. Breast cancer happens when cells stop working correctly, creating abnormal cells that grow uncontrollably. These cancer cells can form tumors and if left untreated, can spread to other parts of your body.
While its possible for anyone to be diagnosed with breast cancer, the disease occurs almost entirely in cisgender women.
Recommended Reading: Can Breast Cancer Cause Stomach Pain
Breast Cancer Screening Patient Version
On This Page
Screening is looking for signs of disease, such as breast cancer, before a person has symptoms. The goal of screening tests is to findcancer at an early stage when it can be treated and may be cured. Sometimes a screening test finds cancer that is very small or very slow growing. These cancers are unlikely to cause death or illness during the person’s lifetime.
Scientists are trying to better understand whichpeople are more likely to get certain types of cancer. For example, they look at the person’s age, their family history, and certain exposures during their lifetime. Thisinformation helps doctors recommend who should be screened for cancer, whichscreening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarilythink you have cancer if he or she suggests a screening test. Screeningtests are done when you have no cancer symptoms. Women who have a strong family history or a personal history of cancer or other risk factors may also be offered genetic testing.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests, rather than screening tests.
See the following PDQ summary for more information about cancer screening:
The Harms Of Mammography Include The Following:
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. A false-positive test result is usually followed by more tests , which also have risks.
When a breast biopsy result is abnormal, getting a second opinion from a different pathologist may confirm a correct breast cancer diagnosis.
Most abnormal test results turn out not to be cancer. False-positive results are more common in the following:
False-positive results are more likely the first time screening mammography is done than with later screenings. For every ten women who have a single mammogram, one will have a false-positive result. The chance of having a false-positive result goes up the more mammograms a woman has. Comparing a current mammogram with a past mammogram lowers the risk of a false-positive result.
The skill of the radiologist also can affect the chance of a false-positive result.
False-positive results can lead to extra testing and cause anxiety.
If a mammogram is abnormal, more tests may be done to diagnose cancer. Women can become anxious during the diagnostic testing. Even if it is a false-positive test and cancer is not diagnosed, the result can lead to anxiety anywhere from a few days to years later.
False-negative test results can delay diagnosis and treatment.
You May Like: Can You Be An Organ Donor After Breast Cancer
Also Check: Can You Get Breast Cancer In Both Breast
For Women Who Have Had Mantle Radiation:
- a clinical breast exam every six months beginning at the time of your radiation treatment
- an annual mammogram starting eight years after your radiation treatment
- possible annual breast MRI
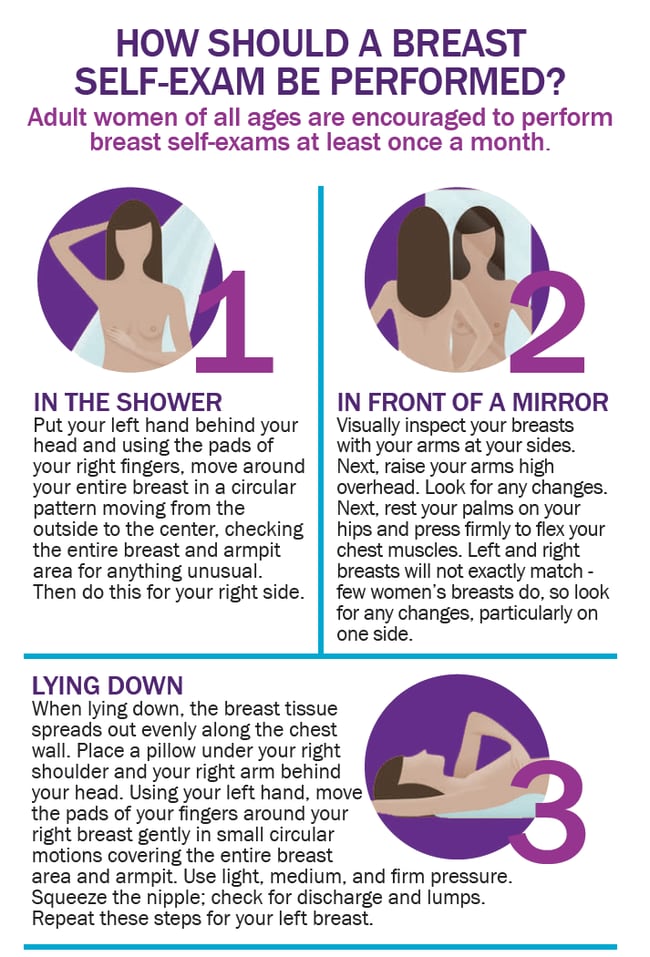
All women at above-average breast cancer risk should speak with their doctor about additional screening tests, perform a monthly self breast exam, and become familiar with their breasts so they are better able to notice changes.
MSK offers a comprehensive program for women at increased breast cancer risk, including regular breast exams and imaging. It allows any developments to be identified and dealt with right away.