Why Receptor Status Matters
Breast cancer is not a single disease, and researchers now have the ability to break down breast cancer into different subtypes based on the receptor status of the tumors. Among the variations between different types of breast cancers are the proteins found on cell surfaces, which are involved tumor growth. These proteins are related to the genetic material of cancer cells.
For example, with estrogen receptor-positive breast cancer, estrogen binds to specific receptors on breast cancer cells, stimulating proliferation. Similarly, HER2 receptors on the surface of breast cancer cells are stimulated by HER2 protein, promoting the growth and spread of breast cancer.
It’s important to note, however, that all breast cellsboth cancerous and noncanceroushave HER2 receptors other their surfaces. The difference is that HER2-positive breast cancer cells have 40 to 100 times more receptors than HER2-negative breast cancer cells or normal breast cells. In positive cases, the abundance of receptors fuels the cancer.
Breast Cancer Discussion Guide
Get our printable guide for your next healthcare provider’s appointment to help you ask the right questions.
Determining Your Her2 Status
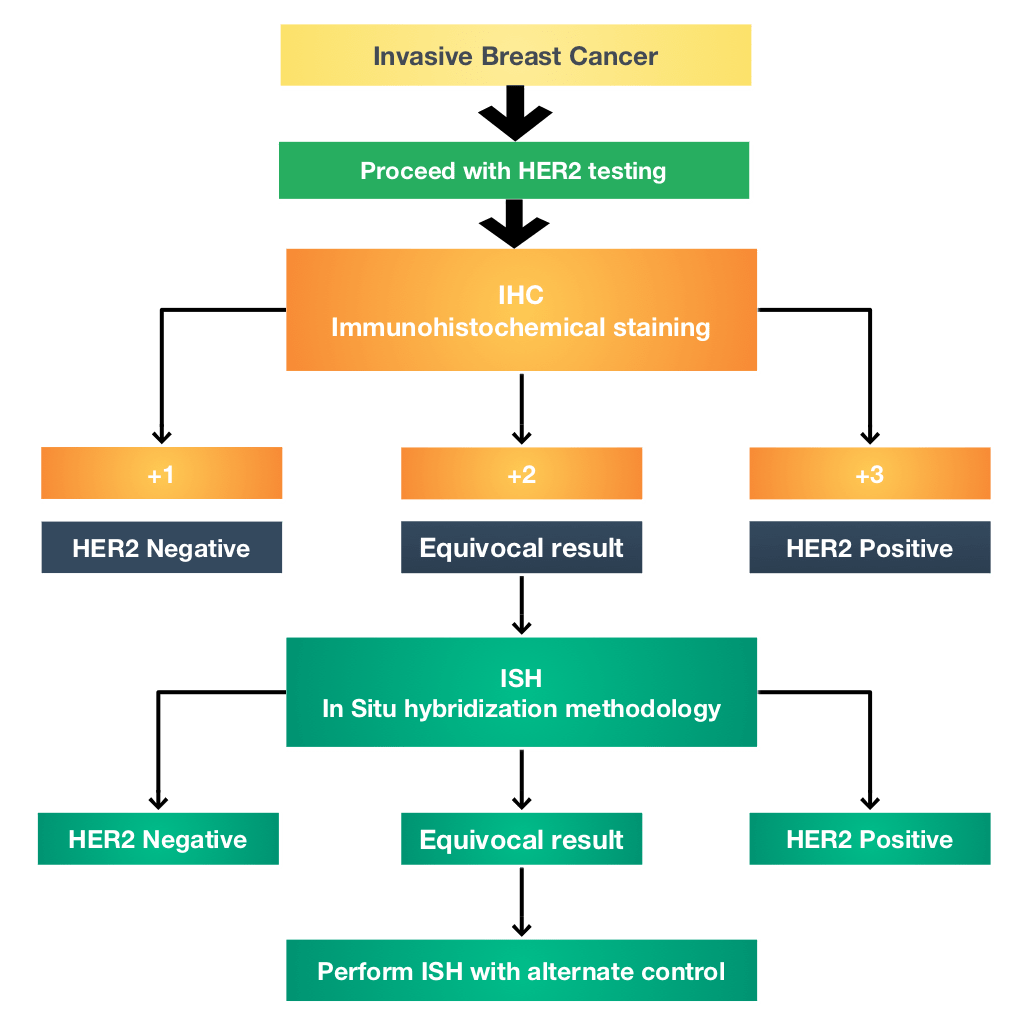
A breast biopsy is used to determine HER2 status. The biopsy can be sent for laboratory testing with an immunohistochemistry test. The fluorescence in situ hybridization test looks for the HER2 gene in breast cancer cells.
The results of an immunohistochemistry test show different levels of HER2 positivity. For example, a tumor may be reported as 0, 1+, 2+, or 3+. Tumors with a higher number may be referred to as having an overexpression of HER2.
According to the American Cancer Society, immunohistochemistry test results should be considered as follows:
| Designation | |
|---|---|
| Equivocal | |
| 3+ | HER2-positive |
The impact of being HER2-positive on breast cancer survival is, of course, a top concern. Unfortunately, statistics can be misleading without considering other aspects of your diagnosis, including cancer stage at diagnosis and whether the tumor is also estrogen and/or progesterone receptor-positive.
With this in mind, you may also be tested for progesterone and estrogen receptors. Triple-negative breast cancers are negative for HER2, estrogen, and progesterone, while triple-positive breast cancers are positive for all three.
Treatments And The Treatment Dilemma
If you have triple negative or HER2-negative breast cancer, many commonly used therapies may not help your disease. If your cancer is HER2-negative but not triple negative, you are still a candidate for endocrine therapy typically used to treat breast cancer. If your tumor is HER2-negative and triple negative, there are still treatments available to help your particular type of breast cancer.
Women with triple negative cancer are usually candidates for chemotherapy, surgery, and radiation. In fact, this type of breast cancer may respond better than other types to chemo if its treated early on.
Newer therapies, such as PARP inhibitors, VEGF inhibitors, and EGFR-targeted treatments, are also showing promise in helping women with metastatic triple negative breast cancer in clinical trials.
Surgery, chemo, hormone therapies, and some targeted treatments may be options for those with HER2-negative breast cancer.
Talk to your doctor about what treatments are most effective for your type of cancer.
Also Check: What Percentage Of Breast Cancer Is Triple Negative
Should I Enroll In A Clinical Trial
Clinical trials are definitely worth considering, according to the Susan G. Komen organization. They offer the chance to try and possibly benefit from new treatments. The best time to join a trial is before starting treatment or, if your provider is considering changing treatments, before you switch to a new treatment. Ask your doctor if there are any trials that would suit your circumstances. You can also search the clinical trial database at ClinicalTrials.gov or use the Susan G. Komen Metastatic Trial Search, a personalized tool to match you with clinical trials.
Does The Her2 Alteration Affect Sensitivity To Anthracyclines
When evidence emerged indicating that HER2 amplification is a poor prognostic indicator in breast cancer,,,,, investigators began to query whether this outcome may be linked to altered sensitivity to various standard chemotherapies. To this end, archived tumor samples from a number of adjuvant trials conducted in the pre-trastuzumab era were analyzed. Initially, several studies evaluating non-anthracycline-based chemotherapy indicated that HER2 overexpression was associated with resistance to chemotherapy and thus may, at least in part, explain the poor outcome associated with this genetic alteration,,.
Table 1 Summary of studies anthracycline vs non-anthracycline chemo: outcome based on HER2.
Several additional studies,,,,, also showed a trend toward a positive relationship between the HER2 alteration and benefit from dose intense anthracyclines. Dhesy-Thind performed a meta-analysis,,, using FISH data from the Belgian study and data from the high dose and medium dose anthracycline arms from the CALGB 8541 analysis. This showed that those with HER2+ breast cancer derive a significant DFS benefit from dose intense chemotherapy whereas those with HER2 disease do not . While two studies, failed to show an association with HER2 status and benefit from an additional cycle of anthracycline, these trials were confounded by the addition of either taxane or high dose chemotherapy followed by stem cell rescue in the arm with less anthracycline.
You May Like: How Effective Is Chemotherapy For Breast Cancer
The Exploration Of Other Genomic Alterations
As referenced above, Desmedt and colleagues analyzed tumor tissue from a neoadjuvant clinical trial of anthracycline-based therapy and showed that pCR was associated with TOP2A amplification. As part of this study, they also developed an A-score comprised of a TOP2A gene signature and two signatures related to tumor invasion and immune response. They validated the A-score in two cohorts of patients treated with neoadjuvant anthracycline-based regimens. This signature was shown to be associated with a high negative predictive value for pCR in both HER+ and negative disease. It does not appear, however, to have been evaluated in a study with anthracycline- vs non-anthracycline-based therapy.
Investigators have also investigated duplication of chromosome 17 centromere as a marker of sensitivity to anthracyclines. It should be noted that it is not rare to see increased numbers of CEP17 in breast cancer and, in particular, HER2+ breast cancer . It is not clear that these increased CEP17 numbers actually represent duplication. It is difficult to envision why increased copies of CEP17 would lead to anthracycline sensitivity. However, a number of groups analyzed breast tumor samples for CEP17 dup with varying definitions with inconsistent results,,.
How Can I Tell If My Treatment Is Working
One way youll know is if your pain starts going away, Brufsky says. Your doctor will also monitor your progress every few months with a variety of assessments, which may include a physical exam, blood tests to check for tumor markers, and imaging tests: X-ray, CT scan, PET scan, or bone scan. The results of these tests, combined with the symptoms you report, will help your cancer team understand whether your treatment is helping to control tumor growth, according to Breastcancer.org.
Treatment is typically continued if its working and your side effects are manageable, but if the treatment is no longer working or the side effects are problematic, your doctor may switch you to a different drug. We expect that just about every treatment we choose will work for a period of time and then likely stop working as the cancer develops resistance, Brufsky says. Fortunately, we have many treatments that are effective with HR-positive/HER-2-negative metastatic breast cancer.
Recommended Reading: Where Can Breast Cancer Lumps Be
Is Her2 Breast Cancer Curable
The chances of successfully treating HER2 breast cancer is high if the cancer is detected in early stages. HER2 cancers, however, are often high grade tumors in stage III at the time of diagnosis. If HER2 cancer has metastasized at the time of diagnosis, it is treatable but not curable in most individuals.
With the development of medications that specifically target HER2 proteins, HER2-positive breast cancers now have a much better outlook than in the past. HER2-positive cancers that have been in remission for five years are less likely to recur.
What Foods Are Good For Her2 Positive Cancer
A research study found two specific flavonoids in citrus fruits: naringenin and hesperetin. In a lab setting, the flavonoids helped stop HER2-positive cancer cells from growing. Citrus fruits may also help make cancer cells more sensitive to medications that stop them from spreading to other parts of the body.
Don’t Miss: How Often Chemo For Breast Cancer
There Is No Role Of Anthracyclines In Her2+ Disease Regardless Of Top2a Amplification
Though HER2 amplified tumors displayed varying sensitivity to anthracycline-based regimens described above, the introduction of trastuzumab revolutionized systemic therapy in this patient population. After improved TTP and OS was shown with the addition of trastuzumab to chemotherapy in metastatic HER2 amplified breast cancer, further studies in early-stage HER2 amplified breast cancer,, demonstrated significant DFS and OS benefit with the addition of trastuzumab to standard chemotherapy. However, as all three large studies used a combination of trastuzumab and an anthracycline, there was also a four to fivefold increase in the rate of CHF.
A fourth study assigned patients with early-stage HER2 amplified breast cancer to receive either AC-T, AC-T+trastuzumab, or a new anthracycline-sparing, platinum-containing regimen: TCH . This regimen was based on preclinical studies showing synergy with platinum salts and trastuzumab, which was not evident with anthracyclines or taxanes,,. As expected, each trastuzumab-containing group had improved DFS and OS compared to the AC-T arm. Though the statistical plan was to compare each trastuzumab arm head-to-head with the control arm, a post hoc statistical comparison between the two trastuzumab arms was performed, revealing no difference in efficacy with respect to DFS or OS.
Summary Of Treatment Options For Metastatic Breast Cancer
Hormone receptor-positive, HER2-negative breast cancer
Hormonal therapy is considered the standard initial treatment for HER2-negative metastatic breast cancer that is also hormone receptor-positive, and is often given in combination with targeted therapy. However, chemotherapy may also be given. A clinical trial may also be an option for treatment at any stage.
Hormone receptor-negative, HER2-negative breast cancer
In general, chemotherapy or targeted therapy is given for treatment of triple-negative breast cancer. A clinical trial may also be an option for treatment at any stage.
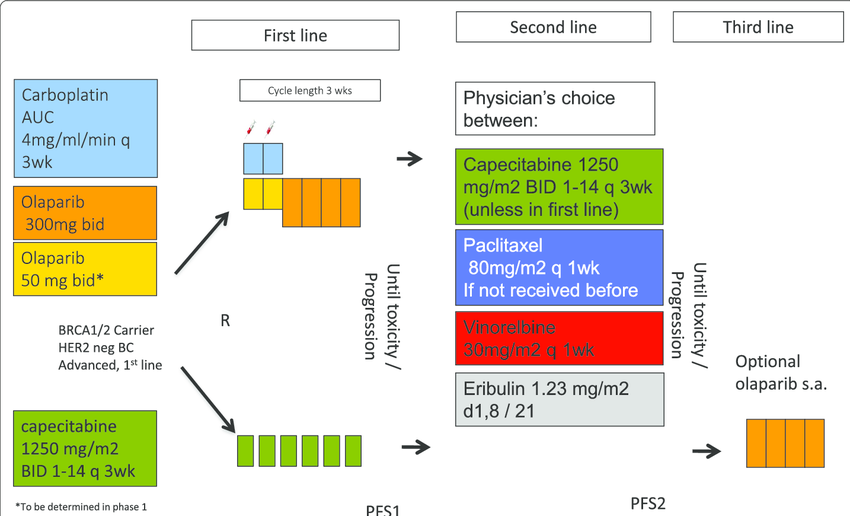
HER2-positive breast cancer that has spread to parts of the body other than the brain
In general, HER2-targeted therapy is regularly added to treatment for HER2-positive breast cancer that has spread. The drugs used depend on the treatments already given and whether the cancer is hormone receptor-positive. The treatment recommendations for first-line, second-line, and third-line or higher treatment are listed below. A clinical trial may also be an option for treatment at any stage.
First-line treatment
Second-line treatment
-
Second-line treatment is used for people with early-stage breast cancer who had the cancer either spread during initial treatment with trastuzumab or return within 12 months after stopping treatment with trastuzumab. It is also used for people whose cancer worsens while receiving first-line treatment.
-
The preferred second-line treatment is the drug T-DM1.
Don’t Miss: How Dangerous Is Stage 3 Breast Cancer
Top2a Amplification And Response To Anthracyclines
Numerous retrospective analyses have been conducted to evaluate whether TOP2A amplification is associated with response to anthracyclines. While the majority have indicated either a significant association or a trend between TOP2A amplification and benefit from anthracycline, a handful have not. As a whole, the results are difficult to interpret due to their retrospective nature, generally small sample sizes as well as their non-standardized testing techniques and varying definitions of alterations.
Table 5 Studies evaluating the relationship between topoisomerase IIa and response to anthracycline .
Press and colleagues analyzed TOP2A status on 279 HER2 amplified tumors from the H0648 trial in which patients were randomized to receive chemotherapy alone or with trastuzumab. They demonstrated a significant association between
TOP2A co-amplification and improved survival in patients treated with an anthracycline. No difference in survival was noted in patients with TOP2A amplified or non-amplified tumors who were treated with paclitaxel.
A larger analysis was performed on samples from the DBCG 89D trial in which patients were treated with adjuvant CMF or CEF,. While there was no differential benefit from anthracycline-based therapy in patients with HER2+ vs HER2 breast cancer in this study, those with tumor TOP2A-amplification had a significantly improved RFS and OS with CEF. Those with TOP2A-normal tumors derived no differential benefit with anthracycline-based therapy.
Life Expectancy And Outlook
In the United States, its estimated that more than 42,000 women will die from breast cancer in 2020.
However, its important to know that aspects like life expectancy and your outlook can vary greatly based off many individual factors.
In the past, a diagnosis with HER2-positive breast cancer was associated with a poor outlook. Advances in drug therapies in recent years have improved the treatment options for HER2-positive breast cancer as well as the outlook for people with the disease.
According to the American Cancer Society, HER2-positive breast cancers are much more likely to respond to drugs that target the HER2 protein, despite the fact that they can grow and spread quickly.
This type of treatment is called targeted therapy. Well discuss it in more detail in a bit.
When considering your outlook, your doctor must analyze many other factors as well. Among them are:
Hormone treatments may be an option for cancer thats also HR positive.
Also Check: Is Breast Cancer Curable In The 3 Stage
How Are Breast Tumors Tested For Her2
Women newly diagnosed with invasive breast cancers should be tested for HER2.
A biopsy or surgery sample of the cancer is usually tested with either immunohistochemical stains or Fluorescent in situ hybridization .
See Testing Biopsy and Cytology Specimens for Cancer and Understanding Your Pathology Report: Breast Cancerto get more details about these tests.
Hormone Receptor Status And Hormone Therapy
Hormone receptor-positive breast cancers can be treated with hormone therapy drugs. These include tamoxifen and the aromatase inhibitors, anastrozole , letrozole and exemestane . Ovarian suppression, with surgery or drug therapies, is also a hormone therapy.
Hormone receptor-negative breast cancers are not treated with hormone therapies because they dont have hormone receptors.
Learn about hormone therapy for the treatment of metastatic breast cancers.
Also Check: How Long Does Someone Live With Stage 4 Breast Cancer
What Is Her2 Cep17 Ratio
CEP17 stands for chromosome enumeration probe 17, which means that the cancer cells have more than one chromosome 17. Cancers that have more than one chromosome 17 are more likely to have more copies of the HER2 gene. The HER2-to-CEP17 ratio is sometimes considered a better indicator of whether a cancer is HER2-positive.
What Is The Grade Of My Tumor
Grading is not the same as staging. Both are indicators of a cancers severity and prognosis, but they use different criteria. Staging deals with the tumor size, location and the distribution of cancer cells in your body. But grading is based on how the cancer cells appear under a microscope.
The more abnormal-looking the cells are, the more likely they are to quickly grow and spread. Grades usually run from I to III. A higher grade is a more aggressive cancer. Its possible to have a Stage I tumor thats also a Grade III cancer.
Read Also: Does Breast Cancer Show In Blood Work
Outcomes According To Hr Status
When HR was positive, the HER2 group and HER2+ + T group had significantly lower LRR , DM and higher DFS at 5 years than that in the HER2+ T group. There were no significant differences in LRR , DM or DFS at 5 years between the HER2 group and HER2+ + T group.
Figure 3 KaplanMeier plots of locoregional recurrence , distant metastasis , disease-free survival , and overall survival of HR-positive patients and HR-negative patients grouped according to HER2 status and trastuzumab treatment. HR, hormonal receptor-negative HR+, hormonal receptor-positive HER2, HER2-negative HER2+ + T, HER2-positive with trastuzumab HER2+ T, HER2-positive without trastuzumab.
When HR was negative, there were no significant differences in LRR, DM, DFS or OS among HER, HER2+ + T, or HER2+ T groups .
What Do The Test Results Mean
The results of HER2 testing will guide you and your cancer care team in making the best treatment decisions.
It is not clear if one test is more accurate than the other, but FISH is more expensive and takes longer to get the results. Often the IHC test is done first.
- If the IHC result is 0 or 1+, the cancer is considered HER2-negative. These cancers do not respond to treatment with drugs that target HER2.
- If the IHC result is 3+, the cancer is HER2-positive. These cancers are usually treated with drugs that target HER2.
- If the IHC result is 2+, the HER2 status of the tumor is not clear and is called “equivocal.” This means that the HER2 status needs to be tested with FISH to clarify the result.
Triple-negative breast tumors dont have too much HER2 and also dont have estrogen or progesterone receptors. They are HER2-, ER-, and PR-negative. Hormone therapy and drugs that target HER2 are not helpful in treating these cancers. See Triple-negative Breast Cancer to learn more.
Triple-positive breast tumorsare HER2-, ER-, and PR-positive. These cancers are treated with hormone drugs as well as drugs that target HER2.
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.
Last Revised: September 20, 2019
Recommended Reading: Does Breast Cancer Cause High Blood Pressure
How Is Tnbc Diagnosed
Imaging tests are usually the first tests done:
- Mammography, the most common screening tool for breast cancer, uses X-rays to take images of the breast and can uncover tumors that may be too small to feel.
- MRI uses a magnet, radio waves and a computer to make detailed images of the breast with a much greater resolution than a mammogram offers.
The next step is a biopsy to remove a sample of suspicious cells from the breast to analyze them. Techniques include:
The appropriate type of biopsy for you depends on factors such as the size and location of the tumor. You may also have a biopsy of your underarm lymph nodes at the same time to see if any cancer is there.