How Is Breast Cancer Treated
If the tests find cancer, you and your doctor will develop a treatment plan to eradicate the breast cancer, to reduce the chance of cancer returning in the breast, as well as to reduce the chance of the cancer traveling to a location outside of the breast. Treatment generally follows within a few weeks after the diagnosis.
The type of treatment recommended will depend on the size and location of the tumor in the breast, the results of lab tests done on the cancer cells, and the stage, or extent, of the disease. Your doctor will usually consider your age and general health as well as your feelings about the treatment options.
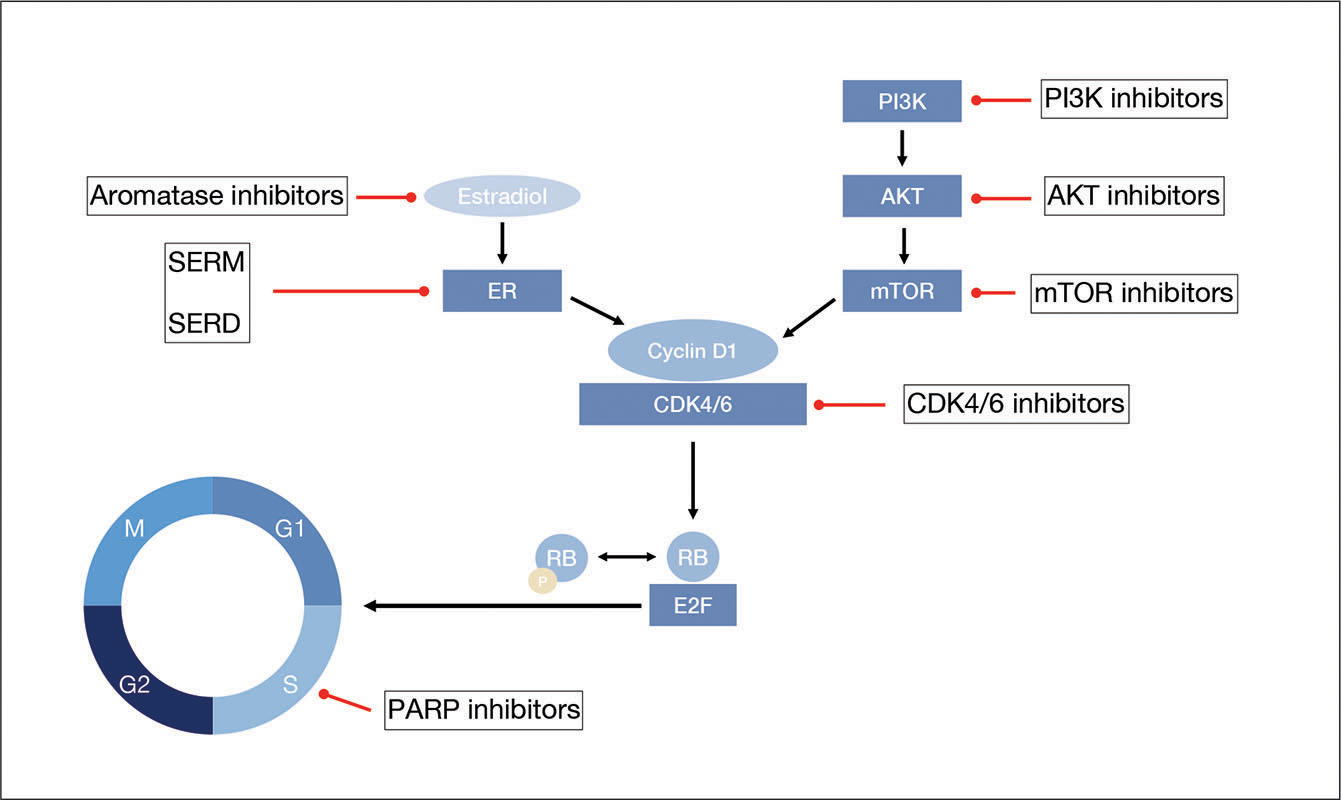
Breast cancer treatments are local or systemic. Local treatments are used to remove, destroy, or control the cancer cells in a specific area, such as the breast. Surgery and radiation treatment are local treatments. Systemic treatments are used to destroy or control cancer cells all over the body. Chemotherapy and hormone therapy are systemic treatments. A patient may have just one form of treatment or a combination, depending on her individual diagnosis.
Recommended Reading: What Is The Survival Rate Of Breast Cancer Stage 4
Other Hormones And Breast Cancer Risk
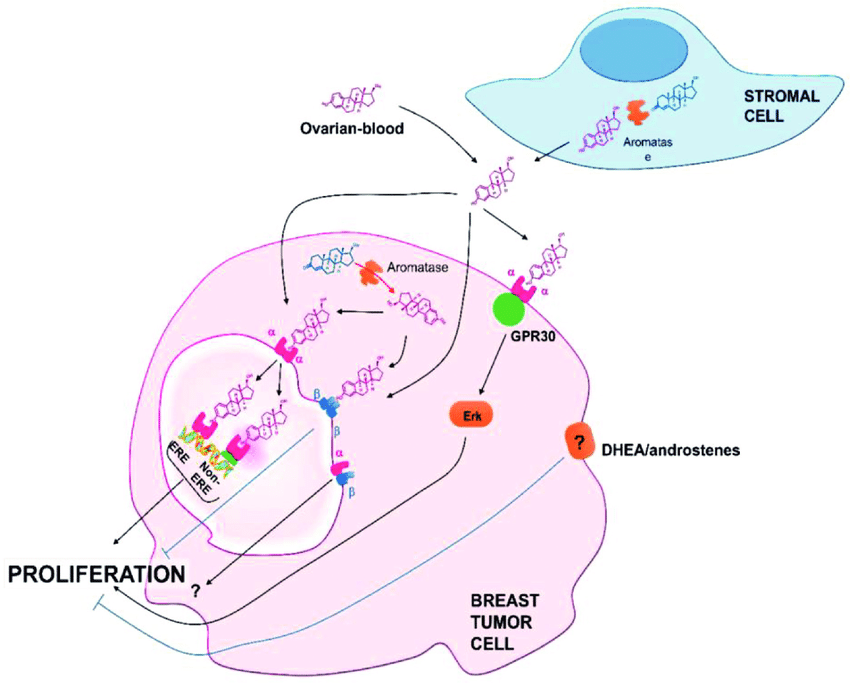
Whereas early hypotheses focused on oestrogens as important hormonal determinants of breast cancer risk , current epidemiological and experimental data indicate that other hormones, such as progesterone , prolactin and testosterone , are also important in the aetiology of breast cancer.
It has been proposed that progesterone augments the effects of oestrogens on breast cancer development , and this hypothesis has gained support from several lines of evidence. Breast cell proliferation has been found to be greatest during the luteal phase of the menstrual cycle , when levels of progesterone are at their highest, and a cross-sectional study of women undergoing breast biopsies found that the mitotic activity in the terminal ductal lobular unit of the breast was greater in women taking combined hormone preparations than in women using oestrogen alone . Furthermore, recent data indicate that hormone replacement therapies containing both oestrogens and progestogens have a greater detrimental effect on risk for breast cancer than preparations containing oestrogens alone . Progestins, like oestrogens, are thought to exert their effects mainly through binding to nuclear receptor proteins.
Signs Of Estrogen Dominance
Estrogen can be metabolized in your body in different ways. Some pathways lead to estrogen metabolites that can compromise your health. This can be a particular problem if your liver is not functioning well. Then your liver doesnt process estrogen metabolites and help remove them from your body, and you end up with more estrogen circulating, causing havoc and estrogen excess.
ED can mean one of two things: you either have too much estradiol in relation to progesterone, or an imbalance in your estrogen metabolites .
This can lead to the following symptoms:
- Worsening PMS
- Lumpy, painful or swollen breasts
- Weight gain, particularly around the hips
Read Also: Will I Survive Breast Cancer
Variant Of Uncertain Significance
A VUS test result is not conclusive. However, most of the time, minor changes in a gene turn out to be normal variants. Most VUS results do not impact the genes ability to work, meaning they dont increase the risk of breast cancer. VUS results are usually treated similar to negative results.
VUS results are much more common with expanded panel testing than with BRCA1/2 genetic testing. Panel testing looks at many genes . With more genes in the test, its more likely youll get a VUS.
Over time, the lab may clarify the meaning of the VUS and send an updated test report to the health care provider who ordered the test. You should be notified if the VUS gets updated.
You can also check with the health care provider who ordered the test every 1-2 years to see if there is any new information about the VUS. While this may seem like a long time to wait, the information isnt likely to change very often.
A VUS test result can be confusing. If you have any questions about a VUS result, meet with a genetic counselor to go over the results.
Emotional Risks For Family Members
Genetic testing may also have an emotional impact on family members.
Your genetic counselor may suggest you talk to your family about BRCA1/2 or expanded panel testing before you get tested or before you learn your results. That way you can find out if they want to know about your results.
For people with a BRCA1/2 or other high-risk inherited gene mutation, figuring out how to tell relatives can be hard.
Some family members may value the option of BRCA1/2 or panel testing. Others may be upset, anxious or angry about hearing the news.
If you have concerns about the best way to share the news with your family members, talk with a genetic counselor. You may prefer to write a letter to your relatives , especially if you have a big family. Your genetic counselor may be able to help you write this letter.
Recommended Reading: Stage 2 Triple Positive Breast Cancer
You May Like: Chances Of Breast Cancer Survival
Taking Charge: Who Gets Breast Cancer
There are no rules about who gets this disease. The two most significant risk factors are being a woman, and increasing age. However, there are other factors that may increase your risk, and some that may lower it.
The development of breast cancer may be influenced by factors that affect the levels of female hormones that circulate in your body throughout life. These factors include the age when you began your menstrual period, the number of times you have been pregnant, your age at first pregnancy, whether you have breastfed your children, and your level of physical activity.
What To Do If A Person Is Concerned About Their Risk
If a person is concerned that they may have inherited a breast cancer gene, they should speak with a doctor. A doctor may suggest for a person to undergo genetic counseling.
Genetic counseling involves a person speaking with a genetic counselor about their chances of developing breast cancer. Genetic counselors can also provide a person with resources and support.
This type of counseling can also help a person decide if they would like to take part in genetic testing or not. Genetic testing involves checking a persons genetic profile for breast cancer-causing genes.
Genetic testing for cancer usually involves a person submitting a blood sample. However, other forms of genetic testing can use cell samples from a persons:
- hair
- anastrozole
Recommended Reading: Grade 2 Breast Cancer Treatment
If You Have Breast Cancer
If you have a breast cancer gene abnormality and you develop breast cancer, your doctor will work with you to determine how your BRCA status might affect your treatment decisions. For example, if you have a BRCA1 mutation, the breast cancer is less likely to be estrogen-receptor-positive, which means that you may not be a candidate for treatment with hormonal therapy. If you have a BRCA2 mutation, however, you are more likely to be a candidate for hormonal therapy. Because research on the PALB2 gene is ongoing, its not clear yet if cancers caused by a PALB2 mutation are likely to have specific characteristics.
Youll also want to talk with your doctor about reducing the risk of a new, second breast cancer or ovarian cancer. Women with breast cancer and a BRCA1 or BRCA2 abnormality have a significantly greater risk of developing a new, second breast cancer, as well as ovarian cancer.
How Much Does Hrt Increase Risk
The risk of developing breast cancer between the ages of 50 and 69 is around:
- 63 in every 1,000 women who have never used HRT
- 83 in every 1,000 women who use combined HRT for five years from the age of 50
- 68 in every 1,000 women who use oestrogen-only HRT for five years from the age of 50
Oestrogen-only HRT increases the risk of womb cancer, so is generally only offered to women who have had their womb removed .
Tibolone is another type of HRT that contains a steroid that acts like oestrogen and progesterone. Tibolone users also have an increased risk of breast cancer, but probably less so than combined HRT users.
Also Check: What Is Estrogen Positive Breast Cancer
Recommended Reading: Malignant Neoplasm Of Breast Treatment
Stopping The Ovaries Working
In premenopausal women, doctors might use a type of hormone treatment to stop the ovaries from producing oestrogen. This type of drug is called a luteinising hormone releasing hormone . For example, goserelin and leuprorelin . You might have this on its own or with other hormone therapy drugs.
LHRH drugs work by blocking a hormone made in the pituitary gland that stimulates your ovaries to make and release oestrogen. This stops your ovaries from working. So you wont have periods or release eggs while you are having the injections.
When you stop taking the drug, your ovaries should start working again. But, if youre close to the age at which your menopause would naturally start, your periods might not start again.
Recommended Reading: Symptoms Of Recurring Breast Cancer
Age At Menarche Is More Influential Than Age At Menopause On Breast Cancer Risk
The observation that lengthening the reproductive life of a woman, either by an earlier menarche or later menopause, increases the risk of breast cancer would suggest that the overall duration of the exposure to estrogen is underlying the risk. However, a recent meta-analysis of reproductive events and breast cancer risk has found that age at menarche may be more of a deciding factor on the risk than age at menopause .
These findings contradict earlier theories that the influence of age at menarche and menopause on breast cancer risk was simply due to the duration of exposure to cycling ovarian hormones. Instead, it seems that the timing of the first exposure of the mammary gland to cyclic hormones sets up a developmental program that has consequences for breast cancer risk later in life.
Don’t Miss: What Does Her2 Negative Mean In Breast Cancer
Will I Be Covered If I Have To Leave Work Because Of Ovarian Cancer
If you are currently covered by insurance through your employer, the Family and Medical Leave Act provides up to 12 weeks of job-protected, unpaid leave during any 12-month period to eligible, covered employees to either care for their own serious health conditions or care for an immediate family member with a serious health condition. FMLA also requires that employees group health benefits be maintained during the leave.
Also Check: Breast Cancer Symptom Checker
Your Race And Ethnicity
White and Black women have the highest risk of developing breast cancer in their lifetime. Asian/Pacific Islander and Hispanic/Latina womens breast cancer rates fall in between two major groupings while American Indian and Alaska Native women are on the lowest end of risk.
While white women are more likely to develop breast cancer than Black women overall, they tend to be diagnosed at an older age . Black women have the highest breast cancer rates among women under age 40. Black women make up a higher percentage of triple-negative breast cancer cases.
What to do: If your race or ethnicity places you at higher risk, make sure you follow all screening recommendations to improve your chances of catching cancer early.
Don’t Miss: Breast Cancer Type 3
Breast Cancer And Hormone Replacement Therapy
Menopause can trigger unpleasant side effects such as hot flushes and vaginal dryness. Hormone replacement therapy eases the symptoms by boosting sex hormone levels. It also reduces the risk of osteoporosis and heart disease.
Since some breast cancers depend on oestrogen, women taking HRT for a long time have a 0.3-fold increased risk. Women who undergo HRT for shorter periods have the same risk of breast cancer as women who have not used HRT. The health benefits of HRT in women in early post-menopause may outweigh the risks in many cases.
Not All Estrogens Are Bad
Let me not vilify all estrogens, as they are not the same. There are 16 forms of estrogens but todays science has only gone deeper into understanding three estrogens: estrone , estradiol and estriol . Out of these three, estradiol tends to be the most aggressive estrogen that has been linked to breast cancer multiplication. In fact, estriol is a protective estrogen that is often prescribed for women with estrogen dominance.
Another thing I need you to know is that it is also certain metabolites that are broken down in the liver that can be antagonistic. In fact, one of the breast cancer risk tests used is a blood test called 2:16 hydroxy-estrone which measures the relationship between estrones metabolites to determine the risk factor. In my practice, I like to look at three markers to identify the risk factor of a women :
The first test can be ordered by your physician, while you can order the saliva test online from Canary Club. The urine tests need to be ordered by an integrative physician, one of whom you can find near you from the listing here .
Recommended Reading: Stage 3 B Breast Cancer
Inheriting Certain Gene Changes
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene changes passed on from a parent.
BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of these genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has up to a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer.
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts.
- Women with one of these gene changes also have a higher risk of developing ovarian cancer and some other cancers.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi origin than in other racial and ethnic groups, but anyone can have them.
Other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
Inherited mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Discovery Of Common Low
The approaches to studying common genetic susceptibility factors have evolved very quickly over the last several years, owing to the completion of the sequencing of the human genome and the mapping of haplotypes of a large subset of the most common genetic variation, namely, the single nucleotide polymorphism ,. Rapid advances in annotating genomes in populations coupled with efficient developments in genotyping technologies together and substantial reductions in genotyping costs now enable determination of hundreds of thousands of SNPs simultaneously. Genetic variants are determined for each individual from a source of genomic DNA using different genotyping technologies such as TaqMan assays for single SNPs or multiplexed genotyping platforms to determine several SNPs simultaneously. The technical advances have enabled investigators to move beyond evaluating a few candidate variants in key genes, to conduct more comprehensive as well as exploratory evaluation of common genetic variation in candidate pathways to cancer, and perform GWAS.
Don’t Miss: Stage 3 Grade 3 Breast Cancer
If Your Risk Is Assessed As Moderate Or High
Consider changing other risk factors for breast cancer as outlined above for women with normal or near-normal risk.
You will be offered a referral to see a doctor who is a specialist. He or she will make a detailed assessment of your risk on the basis of family history.
You may be offered genetic testing and counselling. This is usually done in a specialist genetics clinic. This may involve tests to see if you carry one or more of the faulty genes mentioned above. A blood test may also be taken from your family member who has breast cancer.
Depending on the outcome of the tests and assessment of the risk, some women are offered regular tests such as mammography or MRI scans for screening from an early age. The timing and frequency of any screening tests will depend on your own individual risk.
For a small number of women, whose risk is very high, surgery to remove the breasts and/or ovaries before cancer develops may be an option. This is not an option which is taken lightly and is only done after full risk assessment and counselling.
There are medicines which have also been shown to reduce the risk of breast cancer in women who are at increased risk of the disease.
Risk Factors You Cant Change
Being a woman. Men can get breast cancer too, but itâs 100 times more likely to affect women.
History of breast cancer. A woman who has had cancer in one breast, such as ductal carcinoma in situ or invasive breast cancer, is three to four times likelier to develop a new breast cancer, unrelated to the first one, in either the other breast or in another part of the same breast. This is different than a recurrence of the previous breast cancer.
Age. Your risk goes up as you age. About 77% of women diagnosed with breast cancer each year are over 50, and more than 40% are 65 and older.
In women ages 40 to 50, there is a 1 in 68 chance of developing breast cancer. From 50 to 60, that goes up to 1 in 42. From 60 to 70, its one in 28. And in women 70 and older, its 1 in 26.
Direct family history. Having a mother, sister, or daughter with breast cancer puts a woman at higher risk. Its even greater if this relative developed breast cancer before 50 and had cancer in both breasts.
Having one first-degree relative with breast cancer roughly doubles your risk, and having two first-degree relatives triples your risk. Having a male blood relative with breast cancer will also increase the risk.
Dense breasts. Your breasts are a mix of fatty, fibrous, and glandular tissue. Dense breasts have more glandular and fibrous tissue and less fat. A woman with dense breasts is 1.5 to 2 times more likely to get breast cancer.
Also Check: T3 Breast Cancer