Breast Cancer Tumor Cells
Under the microscope, breast cancer cells may appear similar to normal breast cells or very little like breast cancer cells , depending on the tumor grade. Cancer cells differ from normal cells in many ways.
The cells may be arranged in clusters, and they may be seen invading blood vessels or lymphatic vessels. The nucleus of cancer cells can be striking, with nuclei that are larger, irregular in shape, and stain darker with special dyes. There are also often extra nuclei, rather than just one.
Possible Side Effects Of Breast
As with all operations, bleeding and infection at the surgery site are possible. Other side effects of breast-conserving surgery can include:
- Pain or tenderness or a “tugging” sensation in the breast
- Temporary swelling of the breast
- Hard scar tissue and/or a dimple that forms at the surgical site
- Swelling of the breast from a collection of fluid that might need to be drained
- Change in the shape of the breast
- Neuropathic pain in the chest wall, armpit, and/or arm that doesnt go away over time. This can also happen in mastectomy patients and is called post-mastectomy pain syndrome or PMPS.
- If axillary lymph nodes are also removed, other side effects such as lymphedema may occur.
Md Anderson Multidisciplinary Practices Facilitating Negative Margins And Local Control Of Disease
In our practice there is extensive interaction between the radiologist, the surgeon, and pathologists preoperatively, intraoperatively, and following surgery to ensure adequate resection of the lesion to minimize the need for repeat surgery and LRR. Decisions regarding adequate extent of margins, use of radiation and/or endocrine therapy are made in a multidisciplinary manner and patient input with respect to perceived benefit and risk is also of prime importance.
You May Like: What Does Stage 1a Breast Cancer Mean
Mastectomy And Tumor Margins
With a mastectomy, the whole breast is removed during surgery. Whether the margins contain cancer cells doesnt usually affect your treatment.
In rare cases after a mastectomy, the deep margin contains cancer cells. In these cases, more surgery and/or radiation therapy may be recommended.
With a nipple-sparing mastectomy, whether or not the nipple margin contains cancer cells can affect treatment. If the nipple margin contains cancer cells, more surgery and/or radiation therapy may be recommended.
Dont Miss: What Is The Fish Test For Breast Cancer
Dcis And Invasive Cancer: Which Guideline To Use

The invasive cancer margin guideline endorses no ink on tumor, while the DCIS guideline states that 2mm is an optimal margin. This raises the question of which guideline to apply in microinvasive carcinoma, or when DCIS occurs in association with invasive carcinoma and the DCIS component is in proximity to the margin. The margins consensus panel opted to draw the line for the DCIS guideline at microinvasive cancer, including this with DCIS because most of the lesion is comprised of DCIS, and because small retrospective studies suggest that the behavior of microinvasive carcinoma is more similar to DCIS than invasive cancer,59 and that the use of systemic therapy is more similar to that seen in DCIS. In contrast, invasive cancer with associated DCIS, whether an EIC or lesser amounts, should be managed according to the invasive guideline. In these cases, the biology of the invasive cancer is the primary determinant of outcome and the majority of patients will receive systemic therapy. Additionally, an EIC excised to clear margins does not increase LR,31, 32 although, as discussed previously, it is a potential marker for a heavier residual disease burden.
You May Like: Can You Get Breast Cancer At 18
Md Anderson Contemporary Outcomes Of Bcs For Dcis And Margin Width
For patients undergoing BCS, a previous analysis of 1,216 patients treated at MD Anderson showed that the presence of close margins less than 2 mm did not increase the patient’s risk for in-breast tumor recurrence in comparison to more widely negative margins, provided the patient also received radiation therapy . Specifically, risk of IBTR at 5-years was 3.7% among women with widely negative margins 2 mm compared to 2.2% among women with close or positive margins. Approximately 80% of patients in this cohort received radiation therapy following breast conserving surgery. In multivariable analysis, age, receipt of radiation therapy, and size of DCIS correlated with IBTR risk, whereas margin status did not.
Randomized Trial Data On Resection Margins And Recurrence In Dcis
TABLE 2
Retrospective Studies of Local Control Following Breast Conservation for Invasive Cancer, Reported Since 2000, With More Than 500 Patients per Study
Wapnir et al have recently reported on pooled data from patients participating in NSABP B-17 and B-24 .Importantly, margin-positive patients were allowed to participate in B-24, and the free margin definition in both studies was “no ink on tumor.” The 15-year outcomes were pooled and published recently, showing that IBTR rates in women treated with excision and radiation have climbed since the original reports they are now 19.8% and 16.6% with radiation therapy alone, and a reduction to 13.2% is seen with the addition of tamoxifen in B-24. The ductal carcinoma in situ trial by the European Organisation for Research and Treatment of Cancer , using a similar margin definition, showed similar results, with a 10-year local recurrence rate of 15% in the radiated group. Thus long-term IBTR rates in prospective studies of DCIS tend to be somewhat higher in DCIS patients than in patients with invasive breast cancer when a similar margin threshold is applied. Table 3 highlights IBTR rates relative to margin width in women treated with radiotherapy for DCIS.
Read Also: Can Breast Cancer Start In The Lymph Nodes
Who Can Have Breast
Breast-conserving surgery is a good option for many women with early-stage cancers. The main advantage is that a woman keeps most of her breast. However, most women will also need radiation therapy, given by a radiation oncologist . Women who have their entire breast removed for early-stage cancers are less likely to need radiation, but they may be referred to a radiation oncologistfor evaluation because each patients cancer is unique.
- Are concerned about losing a breast
- Are willing to have radiation therapy and are able to get to the appointments .
- Have not already had that breast treated with radiation therapy or BCS
- Have only one area of cancer in the breast, or multiple areas in one quadrant that are close enough to be removed together without changing the look of the breast too much
- Have a tumor smaller than 5 cm , that is also small relative to the size of the breast
- Are not pregnant or, if pregnant, will not need radiation therapy immediately
- Do not have a gene mutation such as a BRCA or ATM mutation, which might increase your chance of a second breast cancer
- Do not have certain serious connective tissue diseases such as scleroderma or Sjögren’s syndrome, which may make you very sensitive to the side effects of radiation therapy
- Do not have inflammatory breast cancer
- Do not have positive margins
Papers Of Particular Interest Published Recently Have Been Highlighted As Of Importance
Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002 347:122732.
Virnig BA, Shamliyan T, Tuttle TM, Kane RL, Wilt TJ. Diagnosis and management of ductal carcinoma in situ . Evidence Report Number 185, prepared by the Minnesota Evidence-based Practice Centre for the Agency for Healthcare Quality and Research Publication No. 09-E018. Rockville, MD. AHQR, September 2009.
Newman LA, Kuerer HM. Advances in breast conservation therapy. J Clin Oncol. 2005 23:168597.
Houssami N, Macaskill P, Marinovich ML, Morrow M. The association of surgical margins and local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol. 2014 21:71730. Evidence review and meta-analysis that contributed to the development of SSO-ASTRO guidelines on margins in invasive breast cancer.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. J Clin Oncol. 2014 32:150715. SSOASTRO clinical guidelines with recommendations on margins in invasive breast cancer.
Dixon JM, Houssami N. Bigger margins are not better in breast conserving surgery. BMJ. 2012 345, e5855.
You May Like: Can You See Breast Cancer Lumps
Randomized Trials Resection Margins And Recurrence In Invasive Breast Cancer
The original definition of a negative margin proposed by the NSABP was the absence of tumor cells at the ink, and subsequent NSABP studies follow this simple rule. The landmark NSABP study of breast conservation involved 1851 patients the positive margin rate was 6.8%, and with a 20-year follow-up the in-breast tumor recurrence rate was 14.2%. Importantly, there was no attempt to distinguish new primary tumors from true recurrences, and given the 20-year follow-up interval, there was undoubtedly a substantial proportion of new primaries among the 14.2% of women who experienced ipsilateral breast tumor recurrence . According to recent studies that have tried to distinguish between these events, the new primary cancer rate at 10 years may account for up to half of all observed IBTRs. If one estimates the true recurrence rate in the NSABP B-06 trial based on this estimate, then true local recurrences occurred in about 7% of women. Other randomized trials of breast conservation are summarized in Table 1 all used either “grossly free margins” or “microscopically free margins” with no minimal width required, and none distinguished new primaries from true recurrences except for the Danish trial, which reported an overall IBTR rate of less than 6%. In these large studies with long follow-up periods, IBTR rates range from 6% to 19.7%, but margins were not microscopically defined for most of these trials, so the impact of margin width on IBTR rates is difficult to assess.
Experts Debate How To Achieve Both Clear Margins And The Best Cosmesis
IntroductionAnees B. Chagpar, MD, MSc, MA, MPH, FACS, FRCSBreast CenterSmilow Cancer Hospital at Yale-New Haven and Yale University School of MedicineIn a past column on ASCOconnection.org, I talked about a debate that had occurred in our tumor board in which a patient had a margin < 1 mm from ink. While technically negative, it was a little too close for comfort for me the surgeon whose case it was, however, argued based on evidence from the NSABP B-06 trial that if a tumor did not touch ink, outcomes were equivalent to the alternative of mastectomyat least for survival. It brought up how we interpret dataand the difference between what we know and what we think we know or as the comedian Stephen Colbert would put it, between truth and truthiness. We like to think that what we do is evidence-based, but we can almost always find data to support any position we wish to take.My two good friends, Dr. Mel Silverstein and Dr. Mike Dixon, have duked out the margins debate in many public forums and settle the score here once and for all. Here is what we know for sure: obtaining negative margins reduces local recurrence rates there is no consensus on what constitutes an adequate negative margin radiation therapy continues to play a role in breast-conserving surgery there are ways to take out large segments of breast tissue without compromising cosmesis and finally, for the record, Mel is not a Republican .
References
References
Also Check: How Serious Is Stage 3 Breast Cancer
S For Minimizing Residual Tumor
TABLE 3
DCIS IBTR Rates Relative to Margin Width in Patients Receiving Radiotherapy
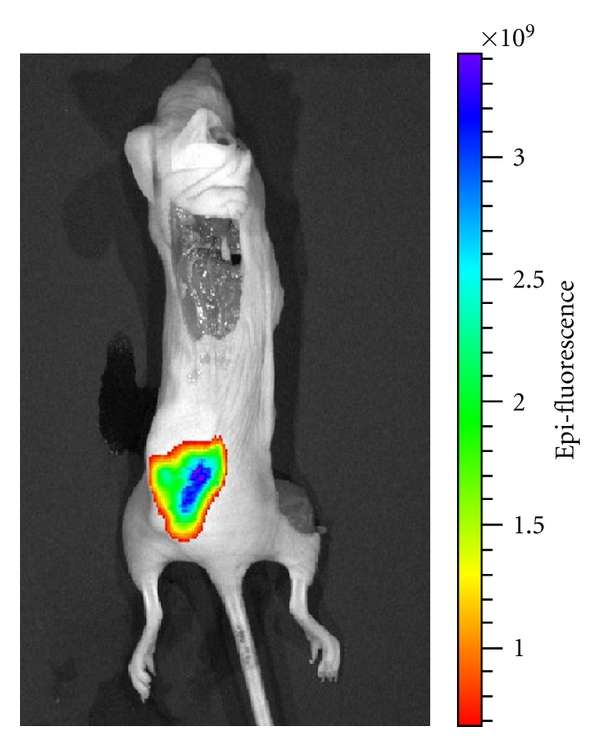
The ability to perform real-time molecular imaging analysis of margins during surgery would clearly be a significant advance several groups have engaged in this effort, with encouraging reports of preliminary data. Further development of such techniques promises to lead to a point at which accurate intraoperative margin evaluation may be possible and may even be combined with therapeutic interventions, using techniques such as photodynamic therapy.
Breast Cancer : Much Progress But Work Remains
Mention that statistic, and many women in the U.S. immediately know it refers to their lifetime risk of getting breast cancer.
Although the statistic may stir up anxiety, those diagnosed with breast cancer today have a more positive prognosis than ever, experts say. Thats due to better understanding of the disease, wider choices of treatments, and more individualized treatment designed to reduce the risk of recurrence and lessen side effects.
While breast cancer incidence has risen by 0.5% per year in recent years, and it remains the second leading cause of cancer death in women, outpaced only by lung cancer, there are now more than 3.8 million breast cancer survivors in the U.S.
If the disease is caught early, women with breast cancer have a survival rate of an astounding 99%, though that may dip to 28% if the cancer has spread.
But despite the progress, much work remains. Read on to see how far weve come in the fight against breast cancer and what experts say needs to happen next.
Breast Cancer: Not a Single Disease
Breast cancer is increasingly viewed as multiple different diseases, says Harold J. Burstein, MD, a breast oncologist at the Dana-Farber Cancer Institute in Boston.
That discovery, in turn, has helped to individualize treatment and predict exactly how much treatment is needed for a specific patient, he and other experts say.
Molecular Diagnostics and ER-Positive Cancers
New Hope for HER2-Positive Cancers
Expanded Genetic Testing
You May Like: Does Breast Cancer Spread To Thyroid
No Association Of Positive Superficial And/or Deep Margins With Local Recurrence In Invasive Breast Cancer Treated With Breast
1Department of Surgery, Hanyang University College of Medicine, Seoul, Korea
2Division of Breast and Endocrine Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
4Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
5Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
* Presented in part at the Global Breast Cancer Conference, Jeju, Korea, April 28-30, 2016.
You May Like: Does Having Breast Cancer Hurt
Radiation Therapy For Dcis
Use of RT is a key consideration when evaluating the adequacy of resection for DCIS. At MD Anderson, we have used a tailored approach when considering the radiation boost dose based on the final surgical margin status. The boost dose is 16 Gy in 8 fractions for patients with positive margins, 14 Gy in 7 fractions for patients with close margins < 2 mm, and 10 Gy in 5 fractions for patients with margins > 2 mm. While there are no high quality prospective data to document appropriate boost dosing and indications in DCIS, the favorable results from the MD Anderson DCIS series cited above support this tailored approach . Further, for patients with DCIS, the extremely favorable results of the Radiation Therapy and Oncology Group 9804 clinical trial, in which 7-year IBTR risk was less than 1% among patients treated with WBRT without a boost, present a strong argument that a tumor bed boost is not needed in the patient population of low-risk DCIS .
Figure 2
| Postmenopausal, hormone-receptor-positive DCIS who underwent lumpectomy with clear margins | 2980 | Anastrozole vs. tamoxifen | Median follow-up of 7.2 years, 67 recurrences for anastrozole vs. 77 for tamoxifen HR: 0.89, 95% CI: 0.64-1.23 no differences in outcomes between treatments |
Abbreviations: NSABP: National Surgical Adjuvant Breast and Bowel Project UK/ANZ: United Kingdom, Australia and New Zealand IBIS: International Breast Cancer Intervention Study HR: Hazard ratio CI: confidence interval
You May Like: Is There Immunotherapy For Breast Cancer
Dcis Margins And Breast Conservation: Md Anderson Cancer Center Multidisciplinary Practice Guidelines And Outcomes
Henry M. Kuerer1 , Benjamin D. Smith2, Mariana Chavez-MacGregor3, 4, Constance Albarracin5, Carlos H. Barcenas3, Lumarie Santiago6, Mary E. Edgerton5, Gaiane M. Rauch6, Sharon H. Giordano3, 4, Aysegul Sahin5, Savitri Krishnamurthy3, Wendy Woodward2, Debasish Tripathy3, Wei T. Yang6, Kelly K. Hunt1
1. Department of Breast Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX 2. Department of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX 3. Department of Breast Medical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX 4. Department of Health Services Research, The University of Texas MD Anderson Cancer Center, Houston, TX 5. Department of Pathology, The University of Texas MD Anderson Cancer Center, Houston, TX 6. Department of Diagnostic Radiology, The University of Texas MD Anderson Cancer Center, Houston, TX.
Corresponding authors: Henry M. Kuerer, MD, PhD, FACS, Kelly K. Hunt, MD, FACS, Department of Breast Surgical Oncology, The University of Texas MD Anderson Cancer Center, 1400 Pressler St, Unit 1434, Houston, TX 77030 E-mail: hkuererorg khuntorg Telephone: 713-745-5043 Fax: 713-794-5026More
Citation:J Cancer
Invasive Breast Cancer Margins: How Much Is Enough
As mentioned, the no ink on tumor guideline has led to a significant reduction in the use of additional surgery after an initial lumpectomy. At MSK, re-excision rates among women with invasive breast cancer declined significantly, from 21.4 percent before to 15.1 percent after early adoption of the guideline in January 2014. The use of BCT rose 13 percent over the same period.
In another study at MSK, we investigated the effect of margin width on LR in patients with triple-negative breast cancer who received BCT and analyzed the results for 535 cancers treated. Seventy-one cancers had margins less than or equal to 2 mm, and 464 had margins greater than 2 mm. Notably, there was no difference in the five-year LR rates between the smaller margin group and the larger margin group .
Read Also: What Is Treatment For Stage 2 Breast Cancer
Read Also: What Deodorant Can I Use After Breast Cancer
International Guidelines For Dcis Margins For Bcs
The new SSO, ASTRO, and ASCO guidelines are also consistent with the European Society for Medical Oncology , the National Institute for Health and Clinical Excellence , and the New Zealand Guidelines Group which all define an appropriate margin width in DCIS to be 2 mm . The National Comprehensive Cancer Network guidelines now also state that margins of at least 2 mm are associated with a reduced risk of ipsilateral breast tumor recurrence relative to narrower negative margin widths in patients receiving WBRT . The American Society of Breast Surgeons defines a negative margin in patients with DCIS as no ink on tumor . Therefore, our group was particularly interested in defining the absolute risk of local recurrence in contemporary patients with less than 2 mm margins treated for DCIS with BCS with and without radiotherapy at MD Anderson.