Which Women Might Consider Having Surgery To Reduce Their Risk Of Breast Cancer
Women who inherit a deleterious mutation in the BRCA1 gene or the BRCA2 gene or mutations in certain other genes that greatly increase the risk of developing breast cancer may consider having bilateral prophylactic mastectomy and/or bilateral prophylactic salpingo-oophorectomy to reduce this risk.
In two studies, the estimated risks of developing breast cancer by age 70 years were 55 to 65 percent for women who carry a deleterious mutation in the BRCA1 gene and 45 to 47 percent for women who carry a deleterious mutation in the BRCA2 gene . Estimates of the lifetime risk of breast cancer for women with Cowden syndrome, which is caused by certain mutations in the PTEN gene, range from 25 to 50 percent or higher , and for women with Li-Fraumeni syndrome, which is caused by certain mutations in the TP53 gene, from 49 to 60 percent .
Other women who are at very high risk of breast cancer may also consider bilateral prophylactic mastectomy, including:
- those with a strong family history of breast cancer
- those with lobular carcinoma in situ plus a family history of breast cancer
- those who have had radiation therapy to the chest before the age of 30 yearsâfor example, if they were treated with radiation therapy for Hodgkin lymphoma
What About Other Cancers
The gene faults that increase the risk of breast cancer and cancer of the ovaries and fallopian tubes in women may also increase the risk of other cancers.
- Faults in BRCA1 may be associated with a slightly increased risk of prostate cancer in men.
- Faults in BRCA2 are associated with a slightly increased risk of male breast cancer, prostate cancer and sometimes cancer of the pancreas or melanoma.
- Li-Fraumeni syndrome is not usually associated with cancer of the ovaries and fallopian tubes, but is associated with bone, soft tissue, brain, lung or adrenal gland cancers, or leukaemia.
- Hereditary non-polyposis colorectal cancer is due to faults in mismatch repair genes. It is not associated with breast cancer but is associated with bowel and other gastrointestinal, uterine and ovarian cancers.
- The doctors at your family cancer clinic will be able to discuss these issues with you in more detail.
Coping With The Effects Of Ovarian Suppression
For some women coping with the effects of ovarian suppression and possibly an early menopause brought on by treatment can be difficult.Your treatment team will discuss with you the possible benefits and risks of ovarian suppression.
If you have ongoing side effects, tell your treatment team so they can suggest how best to manage them.
Research has shown that younger women are more likely to stop taking hormone therapy early if they dont get help with possible side effects so its important to get support if you need it. Not having hormone therapy for the recommended time may increase the risk of breast cancer coming back.
Going through the menopause prematurely can create feelings of loss, and make you feel isolated from women your own age.
You dont have to cope on your own. Some women find it helpful to discuss their feelings and concerns with their breast care nurse or GP. If you feel youd like to talk things through in more depth, a counsellor or psychologist may be more appropriate.
You can also call our free Helpline on 0808 800 6000 and talk with our nurses or use our Ask Our Nurses email service.
Sharing your feelings with someone who has had a similar experience can be helpful. Breast Cancer Now runs services especially for younger women with primary breast cancer:
Find out more about our information and support for younger women with breast cancer.
Also Check: Is Breast Cancer Slow Growing In The Elderly
Data Collection And Statistical Analysis
Vital status and cancer occurrence information were obtained by use of the ongoing follow-uprecords for each study subject from existing clinical research programs and from follow-uptelephone interviews and/or self-administered questionnaires. For women who were deceasedbased on records maintained for each family, we reviewed medical records and family historyreports to establish date of death and whether any malignancy had been diagnosed in that subject.Living women were interviewed by telephone to assess current vital status and occurrences ofcancer. We obtained a self-reported reproductive history and history of hormone replacementtherapy use by interview. Occurrences of postsurgery cancer were verified by review ofmedical records, operative notes, and/or pathology reports.
Screening For Cancer Of The Ovaries And Fallopian Tubes
Women at high risk of ovarian and fallopian tube cancer are advised to consider surgery to reduce their risk . Screening for ovarian cancer is difficult. Unlike breast cancer, which can be detected early with mammograms, there are no screening tests that reliably pick up ovarian cancer at an early stage. Screening with transvaginal ultrasound of the ovaries and measuring CA125 levels in the blood is not recommended. Evidence from large research trials shows that these tests do not effectively pick up ovarian cancer early.
Also Check: Can You Feel Breast Cancer
After Prophylactic Ovary Removal
If you had laparoscopic surgery, you will go home from the hospital the same day or the very next day. Abdominal surgery requires you to spend 1-2 nights in the hospital.
After surgery, your doctor will monitor you for any signs of infection, such as a fever or unusual redness and drainage from your incision. You may be given pain reliever in a pump that you control, giving yourself doses through an intravenous line as needed. As you recover, you also will take some pain medications by mouth, immediately and for a few weeks after your surgery.
The same day or the very next day, your doctor or nurse will have you get up and walk around. Although walking may be painful at first, it can help prevent the formation of blood clots in the legs, strengthen the abdominal muscles, and get your digestive system working again.
Both the surgery itself and the pain medications can slow down your intestines, which play a key role in digesting your food and removing waste from the body. At first, you may not be allowed to take any food or drink by mouth, instead taking your nutrients through an intravenous line. After that, youll probably be restricted to a diet of fluids or soft foods until your doctor is sure that your intestines are working normally again.
How Long Do I Need Ovarian Suppression For
If you are having ovarian suppression to try to preserve fertility during chemotherapy, an injection is usually given at least two weeks before chemotherapy starts, then every four weeks during chemotherapy.
Ovarian suppression as a treatment for primary breast cancer is usually given for between two and five years.
If you are having ovarian suppression for secondary breast cancer, you will usually continue for as long as the treatment is effective.
Also Check: Does Obesity Cause Breast Cancer
How Effective Are Risk
Bilateral prophylactic mastectomy has been shown to reduce the risk of breast cancer by at least 95 percent in women who have a deleterious mutation in the BRCA1 gene or the BRCA2 gene and by up to 90 percent in women who have a strong family history of breast cancer .
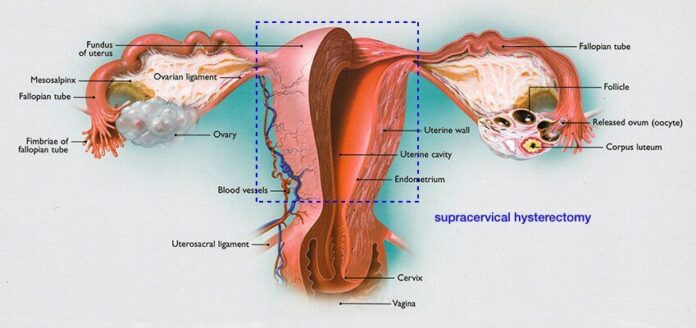
Bilateral prophylactic salpingo-oophorectomy has been shown to reduce the risk of ovarian cancer by approximately 90 percent and the risk of breast cancer by approximately 50 percent in women at very high risk of developing these diseases .
Ovary Removal May Improve Breast Cancer Survival With Gene Mutation
By Andrew M. Seaman, Reuters Health
5 Min Read
– Women with a gene mutation that puts them at a high risk of breast and ovarian cancers have better survival odds if their ovaries and fallopian tubes are removed soon after a breast cancer diagnosis, suggests a new study from Canada.
Women with the BRCA1 gene mutation who were diagnosed with early-stage breast cancer and had salpingo-oophorectomy were 62% less likely to die from the cancer over more than a decade, compared to women who didnt have the procedure.
This is really providing evidence that its going to be effective and have influence on survival, said Kelly Metcalfe, the studys lead author from the Womens College Research Institute in Toronto.
Women with the BRCA1 and BRCA2 gene mutations have up to a 70% risk of developing breast cancer during their lifetimes, the researchers point out online April 23 in JAMA Oncology. Theyre also at an increased risk of ovarian cancer.
Past studies have found that removing the ovaries and tubes after a breast cancer diagnosis reduced the risk of death for women with the gene mutations, but those studies were small or didnt look at the specifics of the cancers, the authors note.
For the new study, they compared data on 676 women with BRCA1 or BRCA2 mutations, who were age 65 or younger and diagnosed with breast cancer between 1977 and 2009. The average age at diagnosis was 42.
The researchers compared 345 women who had their ovaries removed to 331 who did not.
You May Like: How Can Guys Get Breast Cancer
Angelina Jolie Pitt Reveals She Had Ovaries Removed
After actress and filmmaker Angelina Jolie Pitt went public two years ago with her choice to have a preventive double mastectomy to combat the risk of breast cancer, she hinted that another surgery awaited her.
Jolie, who lost her mother, grandmother and aunt to cancer, has the BRCA1 genetic mutation, which puts her at high risk for breast and ovarian cancer.
Now, in an opinion piece published in The New York Times, she has announced that last week she also had surgery to remove her ovaries and fallopian tubes.
âSurgery to remove my tubes and ovaries was the best option because on top of the BRCA gene, three women in my family have died from cancer,â she wrote. âMy doctors indicated I should have preventive surgery about a decade before the earliest onset of cancer in my female relatives. My motherâs ovarian cancer was diagnosed when she was 49. Iâm 39. Last week, I had the procedure: a laparoscopic bilateral salpingo-oophorectomy.â
Dr. Elizabeth Swisher, medical director of the Breast and Ovarian Cancer Prevention Program at Fred Hutchinson Cancer Research Centerâs treatment arm, Seattle Cancer Care Alliance, said Jolie made a lifesaving decision.
Swisher said studies have shown that prophylactic measures, such as the removal of ovaries and fallopian tubes, are effective in avoiding both breast and ovarian cancer.
Prophylactic Ovary Removal To Reduce Risk Of Breast Cancer
Many studies show that prophylactic ovary removal reduces the risk of breast cancer among high-risk women. According to the National Cancer Institute, prophylactic ovary removal would reduce the number of new breast cancer cases among high-risk women by 50%. This benefit occurs only if the ovary removal is performed before menopause. Removing the ovaries before menopause significantly reduces the level of estrogen in a womans body. Because some breast cancers require estrogen to grow, removing the ovaries may slow or even stop the growth of breast cancer cells.
A 2008 study showed that the reduction in breast cancer risk after ovary removal is greater in women with the BRCA2 mutation.
Don’t Miss: What Is The Most Common Treatment For Breast Cancer
What Are The Cancer Risk Reduction Options For Women Who Are At Increased Risk Of Breast Cancer But Not At The Highest Risk
Risk-reducing surgery is not considered an appropriate cancer prevention option for women who are not at the highest risk of breast cancer . However, some women who are not at very high risk of breast cancer but are, nonetheless, considered as being at increased risk of the disease may choose to use drugs to reduce their risk.
Health care providers use several types of tools, called risk assessment models, to estimate the risk of breast cancer for women who do not have a deleterious mutation in BRCA1, BRCA2, or another gene associated with breast cancer risk. One widely used tool is the Breast Cancer Risk Assessment Tool , a computer model that takes a number of factors into account in estimating the risks of breast cancer over the next 5 years and up to age 90 years . Women who have an estimated 5-year risk of 1.67 percent or higher are classified as “high-risk,” which means that they have a higher than average risk of developing breast cancer. This high-risk cutoff is widely used in research studies and in clinical counseling.
Having A Double Mastectomy And Her Ovaries Removed Helped Tess Feel That She Was Doing Something
The two operations, both the mastectomy and then the oophorectomy, the taking the ovaries out, they felt very different because they felt prophylactic. You know I suppose I felt a little bit more in control, like I was doing something, I wasnt just getting rid of disease, I was doing something kind of to help myself in the future. And so I felt, you know, I think that sort of feeling in control made me feel quite, it wasnt so scary. And I guess inevitably its not so scary because you just feel like youre just, youre sort of dealing with possibility rather than actual certainty, having to have it done. So I think it, and again I felt for both those operations.
Surgery to remove the ovaries is known as an oophorectomy. The operation is usually done using laparoscopic or keyhole techniques. This involves using a laparoscope a thin, flexible tube with a light and magnifying lens at the tip. It enables the surgeon to look into the abdomen . The surgery usually involves a general anaesthetic. Two or three small cuts are made into the skin and muscle of the abdomen to allow the laparoscope and other instruments to be inserted. Most women will be in hospital one or two days.
You May Like: How To Reduce Breast Cancer Risk
Breast Reconstruction Using Your Natural Body Tissue
Breast reconstruction can also be done using tissue from another part of the body to create a breast. This is usually done with tissue from:
- the lower tummy , called a transverse rectus abdominis myocutaneous flap, or deep inferior epigastric artery perforator flap or
- the back and shoulder blade area, called a latissimus dorsi flap, with or without an implant.
Breast reconstruction using natural body tissue is a much bigger operation than breast reconstruction using an implant. It takes many hours to perform. The recovery time is longer because there are other wounds that need to heal .
There are lots of things that may influence your choice of breast reconstruction.
Your body shape, your level of physical activity, your general fitness and personal preference are all things to be considered. The costs of all types of breast reconstruction may be covered by Medicare and also by private health funds.
If you are thinking about breast reconstruction, your doctor can refer you to a plastic surgeon experienced in breast reconstruction to discuss your options in detail.
Genetic Testing And Research Focus On How Best To Reduce Cancer Risk
In Canada, public policy mandates that women who undergo hysterectomies have their fallopian tubes taken out, even if no cancer is present. But the impact on ovarian cancer incidence in the country is expected to take years to determine and these opportunistic surgeries, as they are known, affect average-risk women, not those at high-risk for the disease.
Also Check: Where Does Breast Cancer Typically Metastasize To
Environmental And Lifestyle Factors
Most cancer-causing gene changes are not inherited. Instead, they happen throughout a personâs life. They may develop in one or more cells from exposure to substances that damage DNA like ultraviolet light or radiation. They may also develop randomly as a cell grows and divides. Some environmental and lifestyle factors can increase the chances that genes mutate and change. These factors make people more likely to be diagnosed with multiple types of cancer.
Factors that raise the risk of ovarian cancer or breast cancer include:
- Being older
- Being obese
- Never having had children
- Having oneâs first child at a later age
- Using hormone replacement therapy during or after menopause
If you have any of these shared risk factors, you are slightly more likely to develop ovarian cancer and breast cancer.
What This Means For You
If you know you have a BRCA mutation, you may be considering taking steps to keep your risks of breast and ovarian cancer as low as they can be. There are many lifestyle choices you can make, including:
-
never smoking
You also may be considering risk-reducing surgery to remove your ovaries and fallopian tubes. As this study shows, the amount of risk reduction you get depends on the type of BRCA mutation you have. If you have a BRCA1 mutation, your age at the time of the surgery will likely also affect how much your risk of breast cancer is lowered.
Prophylactic surgery decisions require a great deal of thought, patience, and discussion with your doctors, genetic counselor, and family over time along with a tremendous amount of courage. Take the time you need to consider these options, and make decisions that feel comfortable to you and are best for your unique situation.For more information, visit the Breastcancer.org Prophylactic Ovary Removal page.
Read Also: How Is Chemotherapy Administered For Breast Cancer
What Happens When Breast Cancer Develops In A Woman Who Carries A Gene Fault
If breast cancer develops in a woman who carries a gene fault the treatment choices are the same as they are for any woman. Treatment may include mastectomy or breast conservation surgery. Radiotherapy, chemotherapy and/or hormone therapy may also be recommended. Your treatment team may be more likely to recommend a mastectomy or may even recommend removing both breasts if you carry a gene fault. This is because your risk of developing a breast cancer in the other breast in the future is higher than it is for other women.
The treatment for breast cancer depends on lots of factors and these will be discussed in detail with you if this situation develop