Tools Used To Assess Breast Cancer Risk
Several risk assessment tools can help health professionals estimate a womans breast cancer risk. These tools give rough estimates of breast cancer risk, based on different combinations of risk factors and different data sets.
Because each of these tools uses different factors to estimate risk, they might give different risk estimates for the same woman. A women’s risk estimates can also change over time.
Risk assessment tools that include family history in first-degree relatives and second-degree relatives on both sides of the family should be used with the ACS guidelines to decide if a woman should have MRI screening. The use of any of the risk assessment tools and its results should be discussed by a woman with her health care provider.
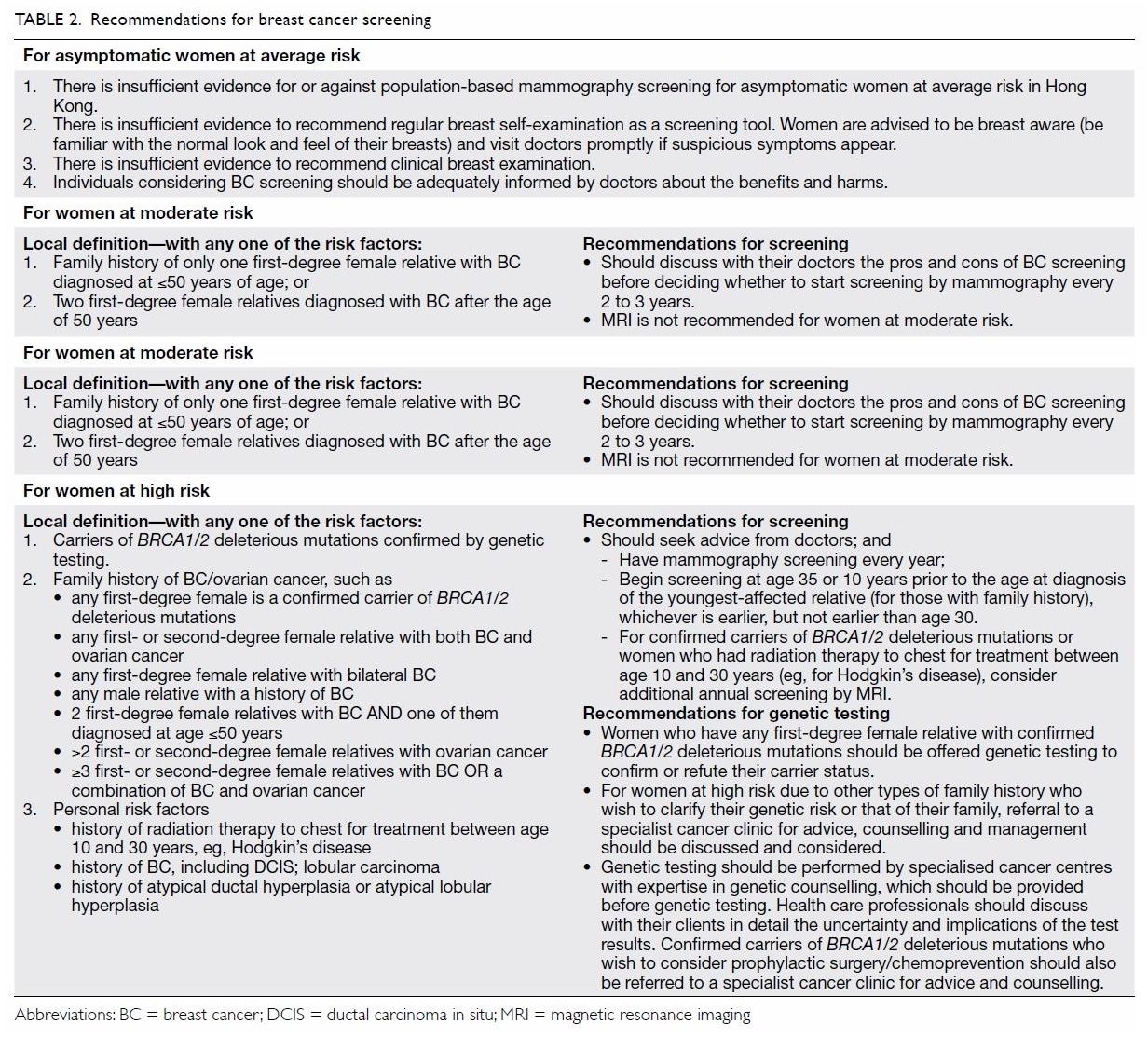
Breast Cancer Screening Guidelines
The decision of when and how often to have breast cancer screening is up to you, based on discussions with your doctor about your personal risks for breast cancer and the benefits of screening.
Breast cancer screening guidelines are generally divided into two groups:
- Guidelines for women at average risk of getting breast cancer
- Guidelines for women at high risk of developing breast cancer
Breast cancer risk is determined based on a combination of your risk factors for breast cancer and other data sets or models, but it is only an estimate. It can vary depending on the assessment tools used.
Breast Cancer Risk Factors
Family history of breast cancer, ovarian cancer, or other hereditary breast and ovarian syndrome- associated cancer
Known deleterious gene mutation
Prior breast biopsy with specific pathology
Atypical hyperplasia
Lobular carcinoma in situ
Prolonged interval between menarche and first pregnancy
Menopausal hormone therapy with estrogen and progestin
Not breastfeeding
Certain ethnicities
Higher body mass index
Prior exposure to high-dose therapeutic chest irradiation in young women
You May Like: What Stage Breast Cancer Do I Have
The Harms Of Mammography Include The Following:
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. A false-positive test result is usually followed by more tests , which also have risks.
When a breast biopsy result is abnormal, getting a second opinion from a different pathologist may confirm a correct breast cancer diagnosis.
Most abnormal test results turn out not to be cancer. False-positive results are more common in the following:
- Younger women .
- Women who have had previous breast biopsies.
- Women with a family history of breast cancer.
- Women who take hormones for menopause.
False-positive results are more likely the first time screening mammography is done than with later screenings. For every ten women who have a single mammogram, one will have a false-positive result. The chance of having a false-positive result goes up the more mammograms a woman has. Comparing a current mammogram with a past mammogram lowers the risk of a false-positive result.
The skill of the radiologist also can affect the chance of a false-positive result.
False-positive results can lead to extra testing and cause anxiety.
If a mammogram is abnormal, more tests may be done to diagnose cancer. Women can become anxious during the diagnostic testing. Even if it is a false-positive test and cancer is not diagnosed, the result can lead to anxiety anywhere from a few days to years later.
False-negative test results can delay diagnosis and treatment.
American Cancer Society Guidelines
The 2015 update of the American Cancer Society guidelines includes the following recommendations :
- Women with an average risk of breast cancer should undergo regular screening mammography starting at age 45 years .
- Women aged 45 to 54 years should be screened annually .
- Women 55 years and older should transition to biennial screening or have the opportunity to continue screening annually .
- Women should have the opportunity to begin annual screening between the ages of 40 and 44 years .
- Women should continue screening mammography as long as their overall health is good and they have a life expectancy of 10 years or longer .
- The ACS does not recommend clinical breast examination for breast cancer screening among average-risk women at any age .
Don’t Miss: What Is The Survival Rate For Lobular Breast Cancer
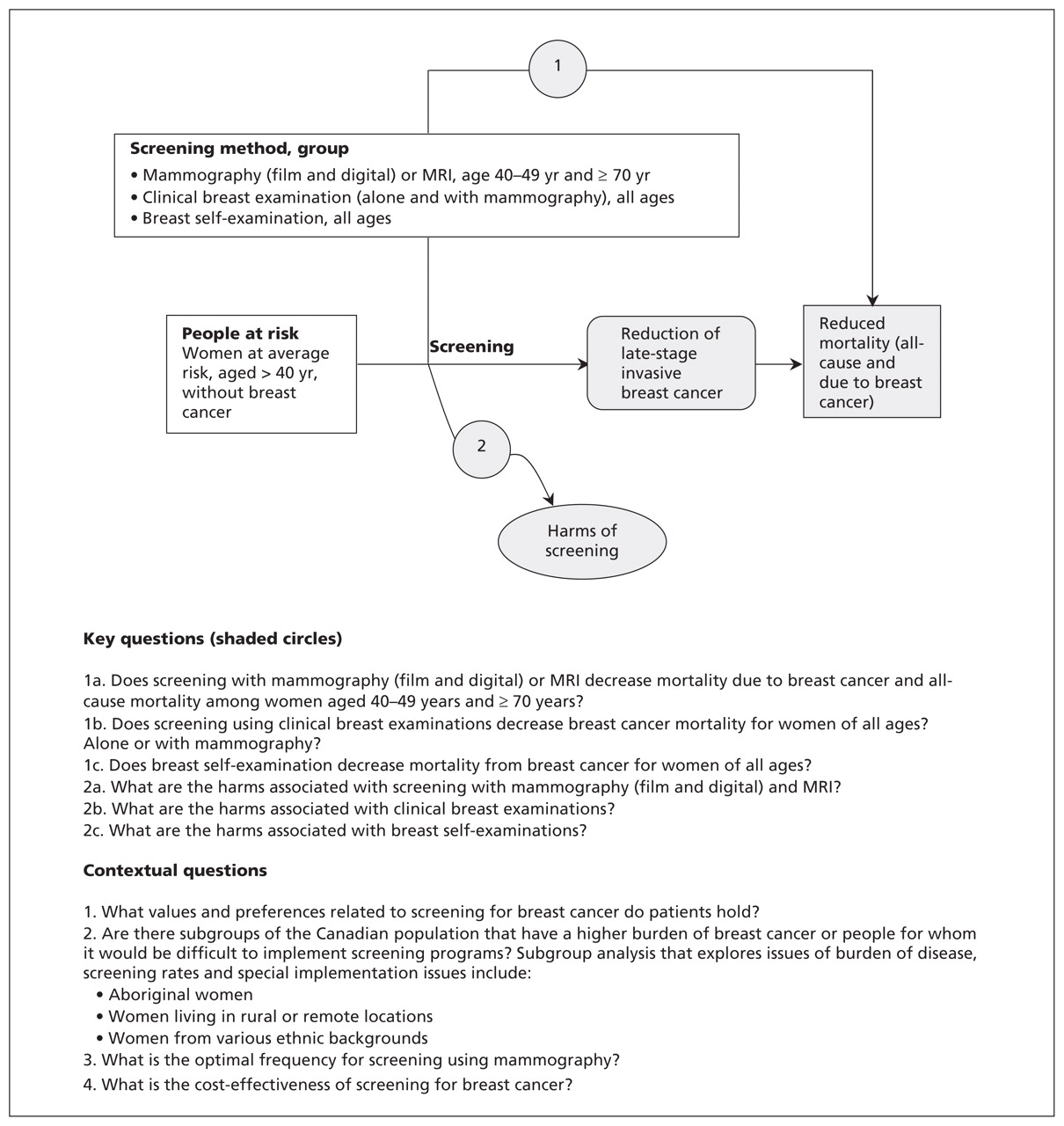
Screening Tests Can Have Harms
Not all breast cancers will cause death or illness in a woman’s lifetime, so they may not need to be found or treated.
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have harms. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the harms of the test and whether it has been proven to reduce the risk of dying fromcancer.
When To Start Screening
Clinical trials, observational studies, and modeling studies all demonstrate that the likelihood of avoiding a breast cancer death with regular screening mammography increases with age, and this increase in benefit likely occurs gradually rather than abruptly at any particular age. In contrast, the harms of screening mammography either remain constant or decrease with age. For example, about the same number of breast biopsies are performed as a result of screening mammography in women aged 40 to 49 years as in those aged 60 to 69 years, but many more of these biopsies will result in a diagnosis of invasive cancer in the older age group. Thus, the balance of benefit and harms improves with age .
It is, however, a false dichotomy to assume that the only options are to begin screening at age 40 or to wait until age 50 years. As women advance through their 40s, the incidence of breast cancer rises. The balance of benefit and harms may also shift accordingly over this decade, such that women in the latter half of the decade likely have a more favorable balance than women in the first half. Indeed, the CISNET models suggest that most of the benefit of screening women aged 40 to 49 years would be realized by starting screening at age 45.7, 8
Don’t Miss: Breast Cancer Walk Philadelphia 2022
Find An Imaging Location
The following are the recommended guidelines for breast cancerscreening by age and risk factor:
Beginning at 16 to 18:
- Breast self-exam
Breast cancer is one of the few cancers that can sometimes be felt. Itis important to become accustomed to how your breasts naturally feel sothat you can recognize any abnormalities. Breast tissue can be lumpy,but if you think you feel something abnormal, you should contact yourdoctor.
20 onward:
This is typically conducted at your yearly gynecological or physicalexam.
40 onward:
- Annual mammogram
There is no recommended age at which you should stop receiving annualmammograms, unless you have less than five years of life expectancy dueto old age or other illness.
40 onward, with high-risk factors
- Annual clinical breast exam
Considerations For Practice Regarding I Statements
Clinical Breast Examination
Potential Preventable Burden. The evidence for CBE, although indirect, suggests that CBE may detect a substantial proportion of cases of cancer if it is the only screening test available. In parts of the world where mammography is infeasible or unavailable , CBE is being investigated in this way.
Potential Harms. The potential harms of CBE are thought to be small but include false-positive test results, which lead to anxiety and breast cancer worry, as well as repeated visits and unwarranted imaging and biopsies.
Costs. The principal cost of CBE is the opportunity cost incurred by clinicians in the patient encounter.
Current Practice. Surveys suggest 1 that the CBE technique used in the United States currently lacks a standard approach and reporting standards. Clinicians who are committed to spending the time on CBE would benefit their patients by considering the evidence in favor of a structured, standardized examination 2.
Digital Mammography
Potential Preventable Burden. Digital mammography detects some cases of cancer not identified by film mammography film mammography detects some cases of cancer not identified by digital mammography. Overall detection is similar for many women. For women who are younger than 50 years or have dense breast tissue, overall detection is somewhat higher with digital mammography. It is not clear whether this additional detection would lead to reduced mortality from breast cancer.
Magnetic Resonance Imaging
You May Like: What Is Level 3 Breast Cancer
Primary And Adjunctive Screening In Women With Dense Breasts
The USPSTF found insufficient evidence to assess the balance of benefits and harms of adjunctive screening for breast cancer using breast ultrasonography, MRI, DBT, or other methods in women identified to have dense breasts on an otherwise negative screening mammogram.
Epidemiology of Dense Breasts
In the United States, the most commonly used classification system for breast density is the American College of Radiologys Breast Imaging Reporting and Data System 4-category scale . Data from the BCSC indicate that about 25 million women aged 40 to 74 years are classified as having heterogeneously or extremely dense breasts. The proportion of women with dense breasts is highest among those aged 40 to 49 years and decreases with age.14
Increased breast density is a risk factor for breast cancer. Data from the BCSC indicate that, compared with women with average breast density, women aged 40 to 49 years with heterogeneously or extremely dense breasts have a relative risk of 1.23 for developing invasive breast cancer. For women aged 50 to 64 years with heterogeneously or extremely dense breasts, the RR is 1.29, and for women aged 65 to 74 years, it is 1.30.7 However, women with dense breasts who develop breast cancer do not have an increased risk for dying from the disease, after adjustment for stage, treatment, method of detection, and other risk factors, according to data from the BCSC.15
Primary Screening Test Performance Characteristics
Primary Screening Frequency
Assessment
Stay Away From Tobacco
There is no safe form of tobacco. If you smoke cigarettes or use other types of tobacco products, it’s best to stop. It’s also important to stay away from tobacco smoke . Both using tobacco products and being exposed to tobacco smoke can cause cancer as well as many other health problems. If you don’t use tobacco products, you can help others by encouraging the people around you to quit. Call us at 1-800-227-2345 for help, or see How to Quit Smoking or Smokeless Tobacco to learn more about quitting.
Don’t Miss: Rare Forms Of Breast Cancer Symptoms
Category A: Eligible For Direct Entry Into The High Risk Breast Screening Program Based On Personal And Family History
Must meet one of the following risk criteria:
- Known carrier of a gene mutation
- First degree relative of a carrier of a gene mutation , has previously had genetic counselling, and has declined genetic testing
- Previously assessed by a genetic clinic as having an equal to or greater than 25% personal lifetime risk of breast cancer based on family history
- Received radiation therapy to the chest before age 30 and at least 8 years ago
Breast Cancer Screening Recommendations
The United States Preventive Services Task Force is an organization made up of doctors and disease experts who look at research on the best way to prevent diseases and make recommendations on how doctors can help patients avoid diseases or find them early.
The USPSTF recommends that women who are 50 to 74 years old and are at average risk for breast cancer get a mammogram every two years. Women who are 40 to 49 years old should talk to their doctor or other health care provider about when to start and how often to get a mammogram. Women should weigh the benefits and risks of screening tests when deciding whether to begin getting mammograms before age 50.
Also Check: Does Your Breast Hurt If You Have Cancer
Cancer Screening Guidelines By Age
The choices you make about diet, exercise, and other habits can affect your overall health as well as your risk for developing cancer and other serious diseases.
Its also important to follow recommendations for cancer screening tests. Screening tests are used to find cancer in people who have no symptoms. Regular screening gives you the best chance of finding cancer early when its small and before it has spread.
Health care facilities are providing cancer screening during the COVID-19 pandemic with many safety precautions in place. Learn how you can talk to your doctor and what steps you can take to plan, schedule, and get your regular cancer screenings in Cancer Screening & COVID-19.
The tabs below provide information on healthy lifestyle choices that can help lower your cancer risk, and cancer screening test recommendations by age.
Other Approaches To Prevention
The USPSTF has made recommendations about the use of medications to reduce women’s risk for breast cancer, as well as risk assessment, genetic counseling, and genetic testing for BRCA1– or BRCA2-related cancer . These recommendations are available on the USPSTF Web site .
This recommendation statement was first published in Ann Intern Med. 2016 164:279â296.
The âOther Considerationsâ and âDiscussionâ sections of this recommendation statement are available at .
The USPSTF recommendations are independent of the U.S. government. They do not represent the views of the Agency for Healthcare Research and Quality, the U.S. Department of Health and Human Services, or the U.S. Public Health Service.
This series is coordinated by Joanna Drowos, DO, contributing editor.
A collection of USPSTF recommendation statements published in AFP is available at .
Don’t Miss: How To Know If Breast Cancer Spread To Lymph Nodes
Other Screening Tests Have Been Or Are Being Studied In Clinical Trials
Studies have been done to find out if the following breast cancer screening tests are useful in finding breast cancer or helping women with breast cancer live longer.
Breast Exam
A clinical breast exam is an exam of the breast by a doctor or other health professional. He or she will carefully feel the breasts and under the arms for lumps or anything else that seems unusual. It is not known if having clinical breast exams decreases the chance of dying from breast cancer.
Breast self-exams may be done by women or men to check their breasts for lumps or other changes. If you feel any lumps or notice any other changes in your breasts, talk to your doctor. Doing regular breast self-exams has not been shown to decrease the chance of dying from breast cancer.
Thermography
Thermography is a procedure in which a special camera that senses heat is used to record the temperature of the skin that covers the breasts. Tumors can cause temperature changes that may show up on the thermogram.
There have been no randomized clinical trials of thermography to find out how well it detects breast cancer or the harms of the procedure.
Tissue sampling
Breast tissue sampling is taking cells from breast tissue to check under a microscope.Breast tissue sampling as a screening test has not been shown to decrease the risk of dying from breast cancer.
Benefits Of Mammographic Screening
The ACS systematic review also examined the effect of screening mammography on life expectancy. Although the review concluded that there was high-quality evidence that mammographic screening increases life expectancy by decreasing breast cancer mortality, the authors were not able to estimate the size of the increase 23.
Also Check: Pattern For Breast Cancer Pillow
Mammograms And More: Breast Cancer Screening Guidelines
Conflicting guidelines on the age to start mammograms might have youscratching your head. Start at 40 years old, or 50? Every year, everyother?
Johns Hopkins Medicine, along with the American College of Radiology and the Society of Breast Imaging maintain theirrecommendation for women at average risk to have routine annualscreening from 40 through 80 years of age. Women with specific riskfactors may start earlier than age 40.
You should discuss your individual screening options with your doctor.
National Comprehensive Cancer Network Guidelines
The NCCN on screening in average-risk women includes the following recommendations :
- Clinical breast examinations every 1-3 years from age 25-39, then annually from age 40 on
- Begin annual screening mammography at age 40 years.
- Consider tomosynthesis
- Promote breast awareness breast self-examination is not recommended
NCCN guidelines provide four separate sets of recommendations for women at increased risk, on the basis of personal or family history, These include earlier initiation of mammography, in some cases, and consideration or recommendation of annual MRI. Additional considerations include the following:
See Mammography in Breast Cancer for more information.
Read Also: Treating Triple Negative Breast Cancer
Basic Facts About Breast Health:
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
American Cancer Society Guidelines For The Early Detection Of Cancer
Screening tests are used to find cancer before a person has any symptoms. Here are the American Cancer Society’s recommendations to help guide you when you talk to your doctor about screening for certain cancers.
Health care facilities are providing cancer screening during the COVID-19 pandemic with many safety precautions in place. The American Cancer Society Get Screened campaign encourages people to start or restart their recommended cancer screenings. Regular screenings can help find and treat pre-cancers and cancers early, before they have a chance to spread. Visit Get Screened to learn about screening tests and what you can do to get on track with a cancer screening schedule thats right for you.
Recommended Reading: What Percent Of Breast Cancer Is Triple Negative
Tests Are Used To Screen For Different Types Of Cancer When A Person Does Not Have Symptoms
Scientists study screening tests to find those with the fewest harms and most benefits. Cancer screening trials also are meant to show whether early detection helps a person live longer or decreases a persons chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.