Lumpectomy With And Without Radiation For Early
Leonard R. Prosnitz, MDOncology
Breast-conserving therapy with lumpectomy and breast irradiation is an accepted standard treatment for patients with early-stage invasive breast cancer or ductal carcinoma in situ . For both diseases, investigators have tried to identify subgroups of patients who can be “safely” treated with lumpectomy without radiation. Some data suggest that it may be reasonable to omit radiation therapy in patients with small, low-grade invasive or noninvasive tumors and/or in “elderly” patients. Additional studies are needed to better identify criteria to prospectively select appropriate patients for treatment with lumpectomy alone.
Breast-conserving therapy with lumpectomy and breast irradiation is an accepted standard treatment for patients with early-stage invasive breast cancer or ductal carcinoma in situ . For both diseases, investigators have tried to identify subgroups of patients who can be “safely” treated with lumpectomy without radiation. Some data suggest that it may be reasonable to omit radiation therapy in patients with small, low-grade invasive or noninvasive tumors and/or in “elderly” patients. Additional studies are needed to better identify criteria to prospectively select appropriate patients for treatment with lumpectomy alone.
What Is Stage 1 Breast Cancer
Stage 1 breast cancer is the earliest stage of invasive breast cancer. The breast cancer has spread from its original location to the surrounding tissue but it is still contained in a relatively small area.
If you are diagnosed with Stage 1 breast cancer, this means that the tumour is less than 2 centimetres in size. No cancer cells have been found in the lymph nodes or other parts of the body at this stage.
Listen To This Article
Dr. Seema Doshi was shocked and terrified when she found a lump in her breast that was eventually confirmed to be cancerous.
That rocked my world, said Dr. Doshi, a dermatologist in private practice in the Boston suburb of Franklin who was 46 at the time of her diagnosis. I thought, Thats it. I will have to do chemotherapy.
She was wrong.
Dr. Doshi was the beneficiary of a quiet revolution in breast cancer treatment, a slow chipping away at the number of people for whom chemotherapy is recommended. Chemotherapy for decades was considered the rule, the dogma, for treating breast cancer and other cancers, said Dr. Gabriel Hortobagyi, a breast cancer specialist at MD Anderson Cancer Center in Houston. But data from a variety of sources offers some confirmation of what many oncologists say anecdotally the method is on the wane for many cancer patients.
Genetic tests can now reveal whether chemotherapy would be beneficial. For many there are better options with an ever-expanding array of drugs, including estrogen blockers and drugs that destroy cancers by attacking specific proteins on the surface of tumors. And there is a growing willingness among oncologists to scale back unhelpful treatments.
The result spares thousands each year from the dreaded chemotherapy treatment, with its accompanying hair loss, nausea, fatigue, and potential to cause permanent damage to the heart and to nerves in the hands and feet.
Don’t Miss: What Is Hormonal Breast Cancer
Why Receptor Status Matters
Breast cancer is not a single disease, and researchers now have the ability to break down breast cancer into different subtypes based on the receptor status of the tumors. Among the variations between different types of breast cancers are the proteins found on cell surfaces, which are involved tumor growth. These proteins are related to the genetic material of cancer cells.
For example, with estrogen receptor-positive breast cancer, estrogen binds to specific receptors on breast cancer cells, stimulating proliferation. Similarly, HER2 receptors on the surface of breast cancer cells are stimulated by HER2 protein, promoting the growth and spread of breast cancer.
Its important to note, however, that all breast cellsboth cancerous and noncanceroushave HER2 receptors on their surfaces. The difference is that HER2-positive breast cancer cells have 40 to 100 times more receptors than HER2-negative breast cancer cells or normal breast cells. In positive cases, the abundance of receptors fuels the cancer.
Breast Cancer Discussion Guide
Get our printable guide for your next healthcare providers appointment to help you ask the right questions.
Stage 1b Breast Cancer Means One Of The Following Descriptions Applies:
Lymph nodes have cancer evidence with small clusters of cells between the approximate size of a pinprick to the approximate width of a grain of rice .
AND EITHER No actual tumor is found in the breast.
OR The tumor is smaller than the approximate size of a peanut .
Similar to stage 0, breast cancer at this stage is very treatable and survivable. When breast cancer is detected early, and is in the localized stage , the 5-year relative survival rate is 100%.
Don’t Miss: Does Breast Hurt With Cancer
What Is The Survival Outlook For Breast Cancer
According to the National Cancer Institute , the percentage of patients surviving five years after diagnosis is:
- 99 percent for breast cancer that is still local to the breast
- 86 percent for breast cancer that has spread just outside the breast
- 29 percent for breast cancer that has spread to more distant parts of the body
The NCI also lists the five-year survival rate for breast cancer overall as 90.6 percent for women and 83 percent for men.
Stages Of Breast Cancer
Your breast cancer stage indicates the severity of the disease upon diagnosis. Your breast cancer stage indicates the severity of the disease upon diagnosis. Your cancer stage will always stay the same, even if the cancer shrinks or spreads during or after treatment. For instance, if youre diagnosed with stage 1 breast cancer, but the tumor later grows and spreads, its not considered stage 3 or 4 breast cancer. To determine whether the cancer has responded to treatment, a new stage may later be assigned an r in front of it to show that its different from the original stage.
Breast cancer staging is classified by:
- The size and location of the tumor
- Whether the cancer has spread to nearby lymph nodes or other parts of the body
- The grade of the tumoror how likely it is to grow and spread
- Whether certain biomarkershormone receptors or other proteinshave been found
All these attributes help your care team determine how to treat your cancer.
To assess the location, size and spread of cancer, your care team will use the TNM Staging System, developed and updated for breast cancer by the American Joint Committee on Cancer .
- TNM stands for Tumor-Node-Metastasis, which are important factors in determining the severity of your cancer.
- All cancers may be evaluated by TNM markers, but breast cancer staging also uses a few extra criteria for a more detailed description.
- Ultimately, your specific combination of TNM and these other markers will determine your cancers stage.
Also Check: Does Radiation For Breast Cancer Affect Your Teeth
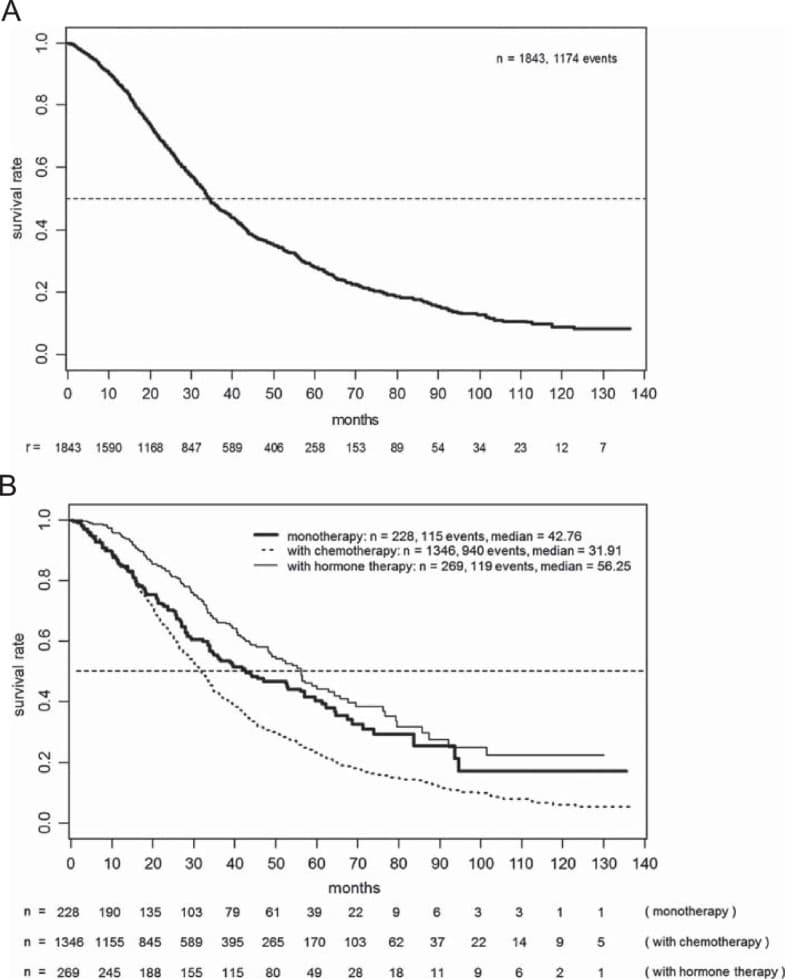
Comparison Of Survival Between Chemotherapy Group And No
The univariate Cox regression analysis for each variable was shown in Table S. Compared to the survival of overall patients in no-chemotherapy group, the result of multivariate analysis shown in Table revealed a better survival in patients received chemotherapy, according to BCSS and OS . We conducted 1:1 PSM analysis between patients in two groups to lower the effects of bias. Finally, we obtained a group with 2,660 patients, and each subgroup included 1,330 patients. As shown in Table , we performed the chi-square test for matched dataset. The P values for each covariables are more than0.05, which indicates the propensity score overlapped well between the two groups of patients.
Table 2 Multivariate Cox proportional hazard model of breast cancer-specific survival and overall survival in all patientsFig. 1
KaplanMeier survival curves of the effect of chemotherapy on BCSS and OS stratified by stage
Fig. 2
KaplanMeier survival curves of the effect of chemotherapy on BCSS and OS stratified by T stage, N stage and tumor grade
Histological grade is one of the fundamental features to describe breast cancer. For patients with grade I and grade II, no statistical survival differences were identified between chemotherapy and no-chemotherapy patients . While for patients with grade III, the chemotherapy patients demonstrated a better prognosis than no-chemotherapy patients in terms of both BCSS and OS .
What Are The Stages Of Breast Cancer
Breast cancer is staged by the size of the tumor and extent of spread. Breast cancers are also graded from one to three, based on how abnormal the cancer cells look and how fast they grow. One is low grade cancer and three is high grade cancer that grows and spreads rapidly.
The four stages of breast cancer are:
- Stage I: The tumor is relatively small and localized to the original site, with possible spread to the sentinel lymph nodes, which are the first lymph nodes the cancer is likely to spread to.
- Stage II: The tumor has grown and spread to a few nearby lymph nodes.
- Stage III: The tumor has grown into many lymph nodes and other tissue in the breast.
- Stage IV: The cancer has spread to distant parts of the body.
Another highly detailed classification system is the TNM classification system based on tumor size, lymph node involvement and metastatic spread.
You May Like: How Long Radiation Treatment For Breast Cancer
Breaking Down The Dogma
The breast cancer treatment guidelines issued by the National Cancer Institute 30 years ago were harsh: chemotherapy for about 95 percent of patients with breast cancer.
The change began 15 years ago, when the first targeted drug for breast cancer, Herceptin, was approved as an initial treatment for about 30 percent of patients who have a particular protein on their tumor surface. It was given with chemotherapy and reduced the chance of a recurrence by half and the risk of dying from breast cancer by a third, almost regardless of how much and what type of chemotherapy was used, Dr. Hortobagyi said.
In a few studies, Herceptin and another targeted drug were even given without chemotherapy, and provided substantial benefit, he added.
That, Dr. Hortobagyi said, started to break the dogma that chemotherapy was essential.
But changing cancer therapies was not easy.
It is very scary, to give fewer drugs, Dr. Hortobagyi said.
It is so much easier to pile on treatment on top of treatment, he continued, with the promise that if we add this it might improve your outcome.
But as years went by, more and more oncologists came around, encouraged by new research and new drugs.
There are now at least 14 new targeted breast cancer drugs on the market three were approved just last year with dozens more in clinical trials and hundreds in initial development.
Now some are in remission 10 or even 15 years after their initial treatment, Dr. Hortobagyi said.
What This Means For You
If youve been diagnosed with early-stage breast cancer, your doctor may recommend treatments after surgery to reduce your risk of recurrence.
If you were diagnosed with hormone receptor-positive, early-stage breast cancer, its likely that your doctor will recommend you take some type of hormonal therapy medicine either tamoxifen or an aromatase inhibitor depending on your menopausal status for five to 10 years after surgery.
Chemotherapy after surgery is usually completed in three to six months. If youre also receiving a targeted therapy, such as Herceptin , with chemotherapy, you may continue to receive the targeted therapy for up to a year after completing chemotherapy.
Radiation therapy after surgery can be completed in one to seven weeks.
So, hormonal therapy after surgery takes the longest to complete. Hormonal therapy medicines also can cause troubling side effects, such as hot flashes, night sweats, and joint pain. Less common but more severe side effects include heart problems and blood clots.
Research has shown that about 25% of women who are prescribed hormonal therapy to reduce the risk of recurrence after surgery either dont start taking the medicine or stop taking it early, in many cases because of side effects.
Learn more about Staying on Track With Treatment. You can read about why its so important to stick to your treatment plan, as well as ways to manage side effects after radiation, chemotherapy, and hormonal therapy.
Don’t Miss: Can Fibrocystic Breast Cause Cancer
Is Her2 Breast Cancer Curable
The chances of successfully treating HER2 breast cancer is high if the cancer is detected in early stages. HER2 cancers, however, are often high grade tumors in stage III at the time of diagnosis. If HER2 cancer has metastasized at the time of diagnosis, it is treatable but not curable in most individuals.
With the development of medications that specifically target HER2 proteins, HER2-positive breast cancers now have a much better outlook than in the past. HER2-positive cancers that have been in remission for five years are less likely to recur.
How Treatment Can Impact Survival Of Early Stage Breast Cancer
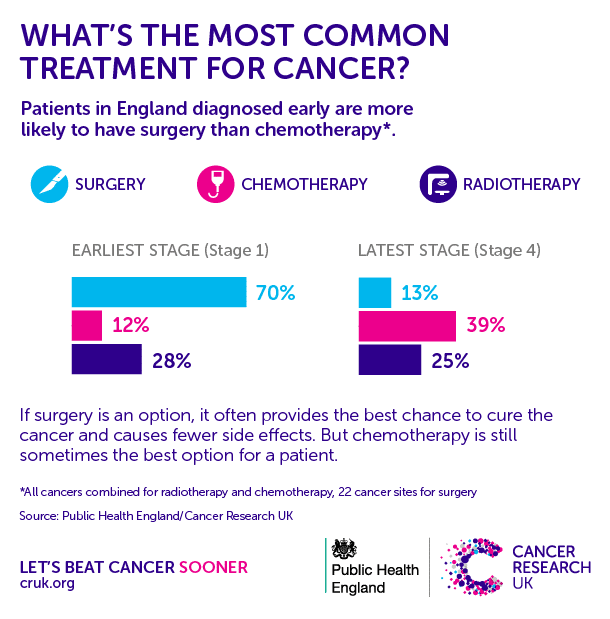
In most cases, the earlier breast cancer is first diagnosed and treated, the better the chance of survival. Cancer cells often become more difficult to treat and may develop drug resistance once they spread. The aim of treatment for Stage 1 and 2 breast cancer is to remove the breast cancer, and any other cancer cells that remain in the breast, armpit or other parts of the body but cannot be detected. Having treatment at this stage can also reduce the risk of the cancer coming back.
Read more:
Don’t Miss: What Cancer Spreads To The Breast
Survival Statistics For Breast Cancer
Survival statistics for breast cancer are very general estimates and must be interpreted very carefully. Because these statistics are based on the experience of groups of people, they cannot be used to predict a particular persons chances of survival.
There are many different ways to measure and report cancer survival statistics. Your doctor can explain the statistics for breast cancer and what they mean to you.
Prognosis And Survival For Breast Cancer
If you have breast cancer, you may have questions about your prognosis. A prognosis is the doctors best estimate of how cancer will affect someone and how it will respond to treatment. Prognosis and survival depend on many factors. Only a doctor familiar with your medical history, the type, stage and characteristics of your cancer, the treatments chosen and the response to treatment can put all of this information together with survival statistics to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person that the doctor will consider when making a prognosis. A predictive factor influences how a cancer will respond to a certain treatment. Prognostic and predictive factors are often discussed together. They both play a part in deciding on a treatment plan and a prognosis.
Doctors use different prognostic and predictive factors for newly diagnosed and recurrent breast cancers.
Read Also: Is Weight Loss A Symptom Of Breast Cancer
Read Also: Can Ovarian Cancer Spread To Breast
Moving Genomic Testing Into Practice
This study is a big deal, said Dr. Timothy Byun, a medical oncologist with The Center for Cancer Prevention and Treatment at St. Joseph Hospital in Southern California, who was not involved in the study.
In an interview with Healthline, Byun said the study may result in fewer breast cancer patients getting chemotherapy, at least in European countries.
In the United States, many of us have already been using the Oncotype DX test to help guide our decisions, said Byun. It uses a 21-gene score. It gives similar information, but we dont know if theres a 100 percent correlation with the MammaPrint test.
Byun referred to the recent TAILORx Trial using the 21-gene test. It found that low-risk patients did well without chemotherapy.
That study showed the test could select a cohort of patients with a 99 percent chance of five-year survival without distant metastasis. For those women, the risks of chemotherapy arent justifiable.
Researchers are still waiting for this data to mature, cautions Byun.
We know that when oncologists see patients after surgery, we look at traditional clinical indicators to guide our decision-making process as to benefits and harms of chemotherapy, he said.
With the information currently available, its likely that some breast cancer patients get unnecessary chemotherapy.
Theres a caveat, according to Byun. Genomic studies, for the most part, have included only estrogen-receptor positive breast cancer patients.
Population And Data Source
Eligible patients included women treated for a primary invasive breast cancer without distant metastasis in the Institut Curie between 1981 and 2008. Patients with a history of previous cancer, with primary chemotherapy, or whose follow-up was less than 3 months were not included.
Data were collected prospectively in this cohort study and were analyzed anonymously. The hospital database was created by knowledgeable workers and validated by a physician. This database was also regularly updated to collect the health status or recent vital status of the patients via phone calls to their doctors and via contacting the governmental records. Data including clinical patient data and tumor characteristics grade, hormone receptor overexpression , human epidermal growth factor receptor-2 status, etc.) were gathered from medical records and pathology reports. The treatment sequence was also recorded: dates of surgery, chemotherapy, radiotherapy, hormone therapy or the administration of targeted therapies such as trastuzumab, as well as adjuvant or neoadjuvant administration. Information regarding the recurrence and vital status of the patients was collected and updated every 12 months.
Recommended Reading: What Are The Physical Symptoms Of Breast Cancer
Examples Of Mortality Rates Versus Number Of Deaths
Say, town A has a population of 100,000 and town B has a population of 1,000. Over a year, say there are 100 breast cancer deaths in town A and 100 breast cancer deaths in town B.
The number of breast cancer deaths in each town is the same. However, many more people live in town A than live in town B. So, the mortality rates are quite different.
In town A, there were 10 breast cancer deaths among 100,000 people. This means the mortality rate was less than 1 percent .
In town B, the mortality rate was 10 percent .
Although the number of deaths was the same in town A and town B, the mortality rate was much higher in town B than in town A .
Lets look at another example. In 2022, its estimated among women there will be :
- 100 breast cancer deaths in Washington, D.C.
- 730 breast cancer deaths in Alabama
- 4,690 breast cancer deaths in California
Of the 3, California has the highest number of breast cancers. However, that doesnt mean it has the highest breast cancer rate. These numbers dont take into account the number of women who live in each place. Fewer women live in Alabama and Washington, D.C. than live in California.
Other factors may vary by place as well, such as the age and race/ethnicity of women. So, to compare breast cancer mortality rates, we need to look at mortality rates.
In 2022, the estimated mortality rates are :
- 25 per 100,000 women in Washington, D.C.
- 21 per 100,000 women in Alabama 22
- 19 per 100,000 women in California 20