Genetic Determinants Of Endogenous Hormones In Relation To Breast Cancer Risk
The genetic control of oestrogen levels has recently received much attention and with it the notion that susceptibility to breast cancer might in part be determined through germline polymorphisms in metabolic genes, specifically those encoding enzymes involved in the biosynthesis and metabolism of oestrogens . Further, it has been suggested that small effects of individual polymorphisms in genes involved in steroid biosynthesis and catabolism might be cumulative . Such polymorphisms might be particularly important among postmenopausal women, in whom oestrogen production is not homeostatically controlled by pituitary gonadotrophins. Several recent epidemiological studies have observed an association between risk for breast cancer and polymorphisms in genes involved in oestrogen synthesis, such as CYP17 and CYP19, and in HSD17B1, which codes for an enzyme that converts oestrone to oestradiol . However, other studies have not found an association between such polymorphisms and breast cancer, and a biological relationship of these polymorphisms with circulating oestrogens and oestrogen metabolites has yet to be established .
Breast Cancer In Postmenopausal Women
Breast cancer is most common in postmenopausal women, and most breast cancers in postmenopausal women are hormone receptor positive. As women age, the fat cells in their breasts tend to produce greater and greater amounts of an enzyme called aromatase. Aromatase promotes the production of oestrogen. Consequently, with age, the levels of oestrogen present in women’s breasts increases. This locally produced oestrogen plays a role in both the development and growth of breast cancer in postmenopausal women. Once established, the tumour acts to increase oestrogen levels to help it grow, with immune cells appearing to boost oestrogen production. Recent studies have also identified a link between obesity and oestrogen production. Data demonstrating that obesity carries a two-fold increased risk of developing breast cancer in older women supports these findings. This makes sense considering that obese women have more of the fat cells responsible for producing oestrogens.
Most Breast Cancers Are Not Genetic
Only five percent of breast cancers are related to genetics and even then, that doesnt mean that all women with the BRAC genes that make them more vulnerable, will go on to develop breast cancer.
Though you cant alter risk factors like your age or parents, simple lifestyle changes can do a great deal to protect you from developing breast cancer.
One of the least discussed but most important steps is to reduce risks caused by too much estrogen.
In my experience working with women, estrogen dominance is very common, but often women dont know the signs or even realize that ED is a concern or that it kick starts substantial health risks.
You can learn how to rebalance your hormones with food in my book, Cooking for Hormone Balance.
Recommended Reading: What Causes Her2 Negative Breast Cancer
Vitamin D And Breast Cancer Prevention
Vitamin D is in fact, not a vitamin at all but a hormone that is synthesized through the action of sunlight upon precursors within the skin. Undiagnosed vitamin D deficiency is now considered to be epidemic among the elderly who stay indoors much of the time, and those living in northern climates where there is less sunshine per day and people tend to wear more clothing. Studies indicate that widespread vitamin D deficiencies are increasing risk for cancers of the colon, pancreas, prostate, ovaries and breast, and that people living at higher latitudes are more likely to die from these cancers, as compared with people living at lower latitudes. . People of darker skin, the obese, and younger children also tend towards a deficiency of vitamin D. Scientists say that vitamin Ds anti-cancer actions lie in its ability to stop the uncontrolled growth of cells and encourage their natural differentiation and death , before they can mutate and become cancerous. The action of vitamin D is also breast protective because it can inhibit the blood supply that feeds tumors in malignant breast tissue.
Can Eating Soy Cause Breast Cancer
There is no shortage of claims on the internet that certain foods can cause cancer. For example, you may have read or heard the myth that eating soy can increase your risk for breast cancer. But is it actually true? Here, we discuss where this idea comes from, what the science says about soy and cancer risk, and what to know about incorporating soy into your diet.
Don’t Miss: Suspicious Malignancy Breast
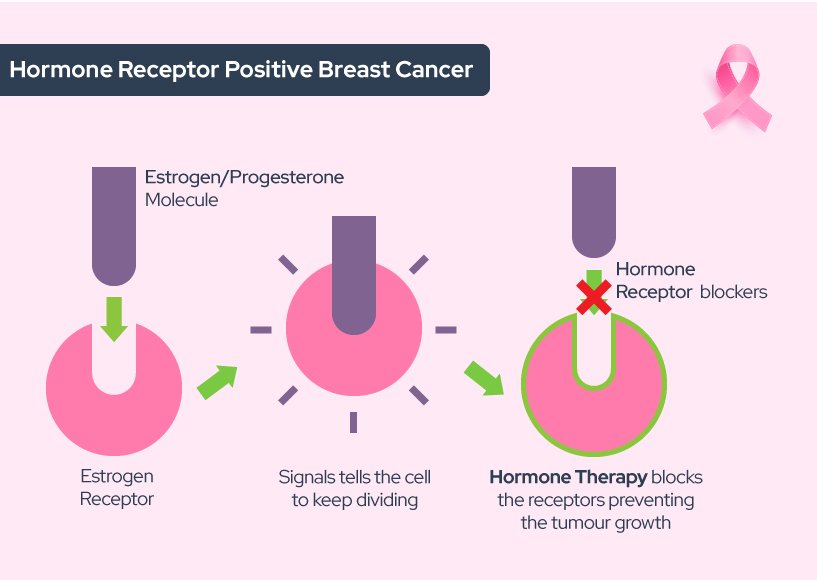
How Does Hormone Therapy Work
About 2 out of 3 breast cancers are hormone receptor-positive. Their cells have receptors for the hormones estrogen and/or progesterone which help the cancer cells grow and spread.
There are several types of hormone therapy for breast cancer. Most types of hormone therapy either lower estrogen levels or stop estrogen from acting on breast cancer cells.
How Much Does Hrt Increase Risk
The risk of developing breast cancer between the ages of 50 and 69 is around:
- 63 in every 1,000 women who have never used HRT
- 83 in every 1,000 women who use combined HRT for five years from the age of 50
- 68 in every 1,000 women who use oestrogen-only HRT for five years from the age of 50
Oestrogen-only HRT increases the risk of womb cancer, so is generally only offered to women who have had their womb removed .
Tibolone is another type of HRT that contains a steroid that acts like oestrogen and progesterone. Tibolone users also have an increased risk of breast cancer, but probably less so than combined HRT users.
Also Check: What Is Estrogen Positive Breast Cancer
Not All Estrogens Are Bad
Let me not vilify all estrogens, as they are not the same. There are 16 forms of estrogens but todays science has only gone deeper into understanding three estrogens: estrone , estradiol and estriol . Out of these three, estradiol tends to be the most aggressive estrogen that has been linked to breast cancer multiplication. In fact, estriol is a protective estrogen that is often prescribed for women with estrogen dominance.
Another thing I need you to know is that it is also certain metabolites that are broken down in the liver that can be antagonistic. In fact, one of the breast cancer risk tests used is a blood test called 2:16 hydroxy-estrone which measures the relationship between estrones metabolites to determine the risk factor. In my practice, I like to look at three markers to identify the risk factor of a women :
The first test can be ordered by your physician, while you can order the saliva test online from Canary Club. The urine tests need to be ordered by an integrative physician, one of whom you can find near you from the listing here .
Risk Factors You Can Change
Weight. Being overweight after menopause increases your odds.
Drinking alcohol.Alcohol is linked to breast cancer. Compared with nondrinkers, women who drink one alcoholic drink a day have a very small increase in risk, and those who are moderate drinkers have about a 20% higher risk.
Hormone replacement therapy . Long-term use of estrogen and progesterone increases the risk of breast cancer. This risk seems to go away if you’ve stopped using them for 5 years or longer.
Being inactive. Your odds go up if you donât exercise.
Reproductive history. Having your first child after age 30 or never having a full-term pregnancy puts you at higher risk. So does not breastfeeding.
Read Also: Stage Iv Breast Cancer Symptoms
The Role Of Estriol In Breast Cancer Prevention
Estriol, the weakest of the three estrogens is thought to protect against breast cancer by softening the effects of its more potent sisters. A revisiting of the literature finds that estriol is vitally important, precisely because it is a weak estrogen. And a number of studies, published over four decades, have demonstrated that estriols unique and perhaps most important role, may be to oppose the growth of cancers, including breast cancer. When lower-strength estriol is used topically, it does not raise the risk of breast cancer as stronger and/or synthetic estrogens do.
Estriols protective action is linked to its ability to bind loosely to hormone receptors on the cell walls of breast tissue, thus blocking more potent estrogens from occupying the sites and stimulating breast cells to grow. Unlike these more excitatory estrogens, estriol does not stimulate growth nearly as much. Some of the best research on the inherent strengths of this weakest of estrogens has been done in Europe where estriol has been more readily available and studied for years:
Women in Balance suggests talking to your physician about bioidentical hormone treatments containing estriol.
How Is Breast Cancer Treated
If the tests find cancer, you and your doctor will develop a treatment plan to eradicate the breast cancer, to reduce the chance of cancer returning in the breast, as well as to reduce the chance of the cancer traveling to a location outside of the breast. Treatment generally follows within a few weeks after the diagnosis.
The type of treatment recommended will depend on the size and location of the tumor in the breast, the results of lab tests done on the cancer cells, and the stage, or extent, of the disease. Your doctor will usually consider your age and general health as well as your feelings about the treatment options.
Breast cancer treatments are local or systemic. Local treatments are used to remove, destroy, or control the cancer cells in a specific area, such as the breast. Surgery and radiation treatment are local treatments. Systemic treatments are used to destroy or control cancer cells all over the body. Chemotherapy and hormone therapy are systemic treatments. A patient may have just one form of treatment or a combination, depending on her individual diagnosis.
Recommended Reading: What Is The Survival Rate Of Breast Cancer Stage 4
What Happens After The Local Breast Cancer Treatment
Following local breast cancer treatment, the treatment team will determine the likelihood that the cancer will recur outside the breast. This team usually includes a medical oncologist, a specialist trained in using medicines to treat breast cancer. The medical oncologist, who works with the surgeon, may advise the use of the drugs like tamoxifen or anastrozole or possibly chemotherapy. These treatments are used in addition to, but not in place of, local breast cancer treatment with surgery and/or radiation therapy.
After treatment for breast cancer, it is especially important for a woman to continue to do a monthly breast examination. Regular examinations will help you detect local recurrences. Early signs of recurrence can be noted in the incision area itself, the opposite breast, the axilla , or supraclavicular region .
Maintaining your follow-up schedule with your physician is also necessary so problems can be detected when treatment can be most effective. Your health care provider will also be able to answer any questions you may have about breast self-examination after the following procedures.
What Is Unique About The Young Mammary Gland That Makes It So Susceptible To Cancer Induction And Protection
The fact that two crucial reproductive events, menarche and young age at parity, have the greatest effect on lifetime breast cancer risk suggests that the young mammary gland represents a crucial window in tumorigenic susceptibility. Why this is the case is less clear. Based on the epidemiological evidence for this, a few hypotheses have been generated, but again few have been tested experimentally, and this work is largely restricted to rodent models.
Recommended Reading: Metastatic Breast Adenocarcinoma
Age At Menarche Is More Influential Than Age At Menopause On Breast Cancer Risk
The observation that lengthening the reproductive life of a woman, either by an earlier menarche or later menopause, increases the risk of breast cancer would suggest that the overall duration of the exposure to estrogen is underlying the risk. However, a recent meta-analysis of reproductive events and breast cancer risk has found that age at menarche may be more of a deciding factor on the risk than age at menopause .
These findings contradict earlier theories that the influence of age at menarche and menopause on breast cancer risk was simply due to the duration of exposure to cycling ovarian hormones. Instead, it seems that the timing of the first exposure of the mammary gland to cyclic hormones sets up a developmental program that has consequences for breast cancer risk later in life.
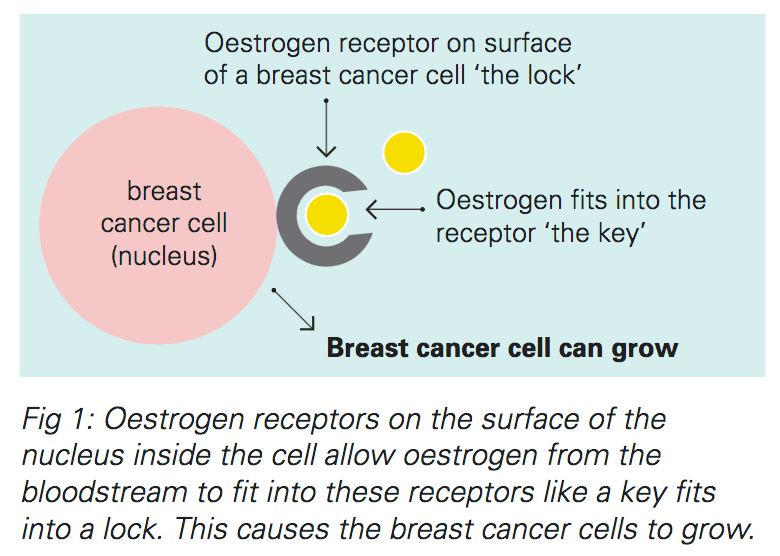
How Estrogen Feeds Cancer
A high proportion of breast cancers are Estrogen Receptor Positive. This means they have a large number of estrogen receptors, indicating that estrogen is helping to feed their growth.
The American Cancer Society explains Estrogen Receptor Positive cancer like this:
Breast cancer that involves estrogen and progesterone receptors is likely to respond to treatments known as endocrine therapies. In medicine, drugs such as Tamoxifen are used to block the estrogen receptors and help prevent the cancer from recurring. In post-menopausal women, drugs called aromatase inhibitors may be more beneficial to help stop production of estrogen.
But what women with breast cancer are rarely told? That as well as taking medication , they can adopt diet and lifestyle strategies which can effectively reduce high levels of the antagonistic estrogen, estradiol.
And addressing estrogen dominance through lifestyle is equally important if you dont have cancer. By reducing your estradiol levels you stabilize your progesterone levels too which in the long-term, could reduce your risk of breasts cancers that are ER Positive and PR Positive.
Reducing Estrogen Dominance is also important to reduce the risk of other ER Positive cancers of the:
- Ovaries
- Prostate, in men
Don’t Miss: How Breast Cancer Affects The Body
Reproductive Risk Factors Oestrogen And Breast Cancer
Oestrogens have an essential role, together with other hormones, in the development of the female sex organs and secondary sex characteristics, the regulation of the menstrual cycle and reproduction. Thus, it has been proposed that the effects of many established reproductive risk factors for breast cancer are mediated by hormonal mechanisms, for the most part involving oestrogens .
Although risk for breast cancer increases with age, there is a marked decline in the rate of increase in risk with age following the loss of ovarian function, either as a result of a bilateral oophorectomy or due to the menopause , showing that hormone production by the ovaries is a crucial risk factor for breast cancer in humans. The duration of exposure to ovarian hormones seems to be closely related to breast cancer risk: a 1-year delay in the onset of menarche is associated with a 5% reduction in risk for developing breast cancer in later life , and each 1-year delay in the onset of menopause is associated with a 3% increase in risk .
Breast feeding is associated with a modest decrease in risk for breast cancer, above and beyond that associated with multiple pregnancies . This effect might be due to the suppression of ovulation, reducing exposure to ovarian hormones.
What Causes Breast Cancer
Many different things can affect your chances of getting breast cancer.
Theres no single cause. It results from a combination of the way we live our lives, our genes and our environment.
We cant predict who will get breast cancer. And we cant confidently say what might have caused someones breast cancer.
There are, however, some things you can do to lower your chances of getting it.
You May Like: What Is The Prognosis For Stage 4 Breast Cancer
Risk Factors You Cant Change
Being a woman. Men can get breast cancer too, but itâs 100 times more likely to affect women.
History of breast cancer. A woman who has had cancer in one breast, such as ductal carcinoma in situ or invasive breast cancer, is three to four times likelier to develop a new breast cancer, unrelated to the first one, in either the other breast or in another part of the same breast. This is different than a recurrence of the previous breast cancer.
Age. Your risk goes up as you age. About 77% of women diagnosed with breast cancer each year are over 50, and more than 40% are 65 and older.
In women ages 40 to 50, there is a 1 in 68 chance of developing breast cancer. From 50 to 60, that goes up to 1 in 42. From 60 to 70, it’s one in 28. And in women 70 and older, it’s 1 in 26.
Direct family history. Having a mother, sister, or daughter with breast cancer puts a woman at higher risk. It’s even greater if this relative developed breast cancer before 50 and had cancer in both breasts.
Having one first-degree relative with breast cancer roughly doubles your risk, and having two first-degree relatives triples your risk. Having a male blood relative with breast cancer will also increase the risk.
Dense breasts. Your breasts are a mix of fatty, fibrous, and glandular tissue. Dense breasts have more glandular and fibrous tissue and less fat. A woman with dense breasts is 1.5 to 2 times more likely to get breast cancer.
Stopping The Ovaries Working
In premenopausal women, doctors might use a type of hormone treatment to stop the ovaries from producing oestrogen. This type of drug is called a luteinising hormone releasing hormone . For example, goserelin and leuprorelin . You might have this on its own or with other hormone therapy drugs.
LHRH drugs work by blocking a hormone made in the pituitary gland that stimulates your ovaries to make and release oestrogen. This stops your ovaries from working. So you won’t have periods or release eggs while you are having the injections.
When you stop taking the drug, your ovaries should start working again. But, if you’re close to the age at which your menopause would naturally start, your periods might not start again.
Recommended Reading: Symptoms Of Recurring Breast Cancer
Other Hormones And Breast Cancer Risk
Whereas early hypotheses focused on oestrogens as important hormonal determinants of breast cancer risk , current epidemiological and experimental data indicate that other hormones, such as progesterone , prolactin and testosterone , are also important in the aetiology of breast cancer.
It has been proposed that progesterone augments the effects of oestrogens on breast cancer development , and this hypothesis has gained support from several lines of evidence. Breast cell proliferation has been found to be greatest during the luteal phase of the menstrual cycle , when levels of progesterone are at their highest, and a cross-sectional study of women undergoing breast biopsies found that the mitotic activity in the terminal ductal lobular unit of the breast was greater in women taking combined hormone preparations than in women using oestrogen alone . Furthermore, recent data indicate that hormone replacement therapies containing both oestrogens and progestogens have a greater detrimental effect on risk for breast cancer than preparations containing oestrogens alone . Progestins, like oestrogens, are thought to exert their effects mainly through binding to nuclear receptor proteins.