Distinctive Predictors Of Self
The ultimate mannequin defined 36% of the variance in self-reported adherence . Facet impact severity defined probably the most distinctive variance , adopted by self-efficacy , and medicine/healthcare system-related limitations . No different components accounted for added distinctive variance.
|
Desk 3 Stepwise Regression Mannequin Inspecting Which Doubtlessly Modifiable Components Uniquely Predict Self-Report Adherence at Baseline |
I Havent Lost My Hair Yet And My Counts Havent Dropped Does This Mean That The Chemotherapy Isnt Working
Not having side effects such as hair loss, lowered blood counts, or nausea doesnt mean that the chemotherapy isnt working. Different therapies cause different side effects. Different people also have different reactions to the same treatment. Your doctor and nurse will monitor your progress and response to treatment.
Targeted Chemotherapy In Early
Research has been performed on targeted chemotherapy agents, including the following:
-
Cyclin-dependent kinase inhibitors
-
Small-molecule epidermal growth factor receptor tyrosine kinase inhibitors
-
Blockade by antiangiogenic agents
-
PI3K/Akt/mammalian target of rapamycin inhibitors
-
Poly polymerase inhibitors]
Recommended Reading: How Does Metastatic Breast Cancer Start
Neoadjuvant Chemotherapy For Invasive Breast Cancer
|
This summary table contains detailed information about research studies. Summary tables are a useful way to look at the science behind many breast cancer guidelines and recommendations. However, to get the most out of the tables, its important to understand some key concepts. Learn how to read a research table. |
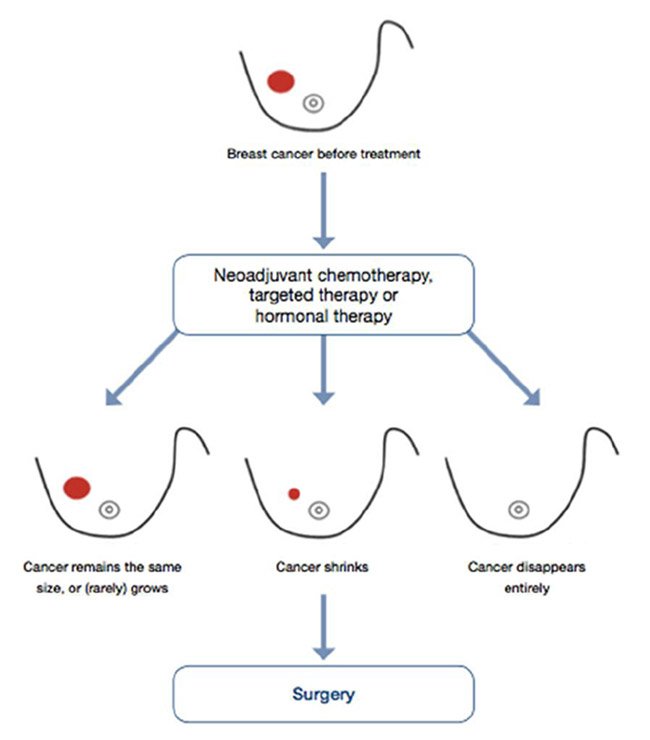
Introduction: Some women with invasive breast cancer may get chemotherapy before breast surgery. This is called neoadjuvant chemotherapy.;
Neoadjuvant chemotherapy may shrink tumors enough so a;lumpectomy becomes an option to a;mastectomy.
Learn about the strengths and weaknesses of different types of studies.
Study selection criteria: Randomized controlled trials with at least 100 participants and meta-analyses.
Table note: These studies looked at different chemotherapy drug regimens, so results cant be compared directly to one another. However, for each study, the neoadjuvant and adjuvant chemotherapy drug regimens are the same.
Can Hormone Therapy Be Used To Prevent Breast Cancer
Yes. Most breast cancers are ER positive, and clinical trials have tested whether hormone therapy can be used to prevent breast cancer in women who are at increased risk of developing the disease.
A large NCI-sponsored randomized clinical trial called the Breast Cancer Prevention Trial found that tamoxifen, taken for 5 years, reduces the risk of developing invasive breast cancer by about 50% in postmenopausal women who were at increased risk . Long-term follow-up of another randomized trial, the International Breast Cancer Intervention Study I, found that 5 years of tamoxifen treatment reduces the incidence of breast cancer for at least 20 years . A subsequent large randomized trial, the Study of Tamoxifen and Raloxifene, which was also sponsored by NCI, found that 5 years of raloxifene; reduces breast cancer risk in such women by about 38% .
As a result of these trials, both tamoxifen and raloxifene have been approved by the FDA to reduce the risk of developing breast cancer in women at high risk of the disease. Tamoxifen is approved for this use regardless of menopausal status. Raloxifene is approved for use only in postmenopausal women.
Also Check: What Is Stage 3a Breast Cancer
Breast Cancer Immunotherapy Supplements The Bodys Defense Systems
Breast cancer immunotherapy is a relatively new approach in breast cancer treatment. Our own bodies have a powerful immune system in place to fight off infection and disease.; So,;;breast cancer immunotherapy is a means of amplifying the effectiveness of the bodys own defense systems.
Its much like receiving a vaccination for the flu or measles, but on a larger scale. By placing antibodies or immune cells from someone else into a breast cancer patients system, the bodys own defenses receive a huge boost.
Breast cancer immunotherapy is still an experimental breast cancer treatment, largely informed by advances fighting immune system diseases such as AIDS.
Physicians will tend to be cautious before utilizing this modality to fight breast cancer.; But when the cancer is not responding to the usual treatments, it is a reasonable approach. There can be rather serious side effects to breast cancer immunotherapy.; So patients and the breast cancer treatment team must take the decision to proceed very carefully.
Who Shouldnt Do Adjuvant Chemotherapy
Adjuvant therapies are not recommended for every cancer patient. Some types of cancer do not have good evidence supporting the use of neoadjuvant, adjuvant, or maintenance chemotherapies. Your cancer stage and the likelihood of remission are also important. If youre not at high risk for cancer to come back, you may not be a good candidate for adjuvant therapies.
You May Like: Can Estrogen Cause Breast Cancer
Sensation Changes In Your Hands Or Feet
Some types of chemotherapy can affect the nerves in your hands and feet. You may develop some numbness or tingling in your fingers, toes, or both. This is known as neuropathy. This may not last or might be permanent depending on how long youre taking the chemotherapy. Your doctor may be able to help your neuropathy by using medications or changing the dose of your chemotherapy. For more information on neuropathy, read Neuropathic Pain.
What you can do:
- Talk with your doctor about putting ice on your hands and feet during your treatment, which may help prevent neuropathy. For more information, read Nail Cooling During Treatment with Taxane-based Chemotherapy.
- Be extra careful to avoid burning yourself when using the stove, oven, or iron. You may not be able to feel heat as much as you used to.
What to avoid:
- Using heating pads or hot packs because you could burn yourself.
Contact your doctor or nurse if you have:
- Problems holding a pencil or pen or closing buttons.
- Pain, burning, or tingling in your fingers or toes.
- Trouble walking or feeling the ground when you walk.
- Trouble balancing resulting in falls.
Rationale For Neoadjuvant Therapy: The Nsabp B
The NSABP B-18 trial was designed to determine whether preoperative treatment with four cycles of doxorubicin/cyclophosphamide would improve overall survival and DFS when compared with the same treatment given postoperatively. At 9 years of follow-up, there was no difference in survival or DFS between the two groups,. A critical observation during this follow-up was that pCR correlated with OS, and this finding became stronger with longer follow up. Primary tumor response graded as pCR, pINV , clinical partial response , or clinical non-responder and was associated with outcome measures of OS , DFS , and RFS . The B-18 trial established that chemotherapy can be given before surgery with no loss of efficacy, opening the way to measuring chemotherapy effect and the testing of novel agents, as in the B-27 trial.
Read Also: Is Stage 2 Breast Cancer Bad
Endocrine Therapy And Chemotherapy
General principles
TNBC and HER2+ breast cancers are each seen in about 15% of older patients. For TNBC, chemotherapy is the only systemic therapy of benefit and should be considered for most patients. HER2+ cancers that are HR are the worst breast phenotype when untreated, and consideration of chemotherapy and trastuzumab is appropriate for most of these patients. Those with small HR+, HER2+ tumors have a better short-term prognosis, and the decision regarding chemotherapy/trastuzumab is more complex; those with larger tumors with this phenotype should be considered for chemotherapy and trastuzumab.
Selection and pitfalls of endocrine therapy
The other major toxicity associated with AI use is accelerated bone loss and an increased risk of fracture. Many older patients already have osteopenia or osteoporosis when breast cancer is diagnosed. Older patients on AIs should be encouraged to exercise and use recommended doses of vitamin D and calcium. For those with severe osteopenia or osteoporosis, either bisphosphonates or other bone-protecting agents such as denosumab should be considered. These agents, although generally safe, can add to the costs of treatment. The World Health Organization fracture risk assessment tool, FRAX, can be used to estimate fracture risk from clinical and bone densitometry data .
Selecting chemotherapy
FIGURE 3
FIGURE 4
Are Neoadjuvant And Adjuvant Therapies Used Together
Because they are administered at different phases of the treatment process, your doctor may suggest you get both neoadjuvant therapies and adjuvant therapies. Neoadjuvant therapies happen before the primary treatment, while adjuvant or maintenance therapies are used after addressing the original tumor with surgery or radiation.
Recommended Reading: What Happens When Breast Cancer Metastasis
Hormone Therapy For Breast Cancer
Hormone therapy is sometimes used to treat breast cancer. It is a treatment that adds, blocks or removes hormones. Hormones are substances that control some body functions, including how cells act and grow. Changing the levels of hormones or blocking certain hormones can slow the growth and spread of breast cancer cells. Drugs, surgery or radiation therapy can be used to change hormone levels or block their effects.
Hormone therapy is only used for breast cancer that is hormone receptor positive. This means that the cancer cells have receptors for estrogen , progesterone or both. When cancer cells have these receptors, the hormones can attach to them and help them grow. Research has shown that giving hormone therapy after surgery and radiation therapy lowers the risk that the breast cancer will come back, and improves survival.
Breast cancer tissue is always tested to find out if it has hormone receptors or does not have hormone receptors . Find out more about .
You may be offered hormone therapy to:
- lower the risk that non-invasive breast cancer, or may lead to an invasive breast cancer
- lower the risk that invasive breast cancer can come back by destroying cancer cells left behind after surgery and radiation therapy
- shrink a large tumour before surgery
- treat locally advanced or recurrent breast cancer
- relieve pain or control the symptoms of advanced breast cancer
Primary Breast Cancer Therapies
The primary treatments for breast cancer are radiation therapy and breast cancer surgery.; In addition, adjuvant therapy is used to limit the chances of the breast cancer returning.
Breast cancer surgery can usually remove all of the malignant cancer cells.;;So adjuvant therapy is a way to kill off cancer cells which may have been left behind or migrated undetected to other areas of the body.
There are many benefits to adjuvant therapies, but they are not without side effects.; Thus,; the patient and the breast cancer team must weigh the decision carefully.
Also Check: Does Red Wine Cause Breast Cancer
Feeling Unwell Or Tired
Many women do not feel as healthy after chemo as they did before. There is often a residual feeling of body pain or achiness and a mild loss of physical functioning. These changes may be very subtle and happen slowly over time.
Fatigue is another common problem for women who have received chemo. This may last a few months up to several years. It can often be helped, so its important to let your doctor or nurse know about it. Exercise, naps, and conserving energy may be recommended. If you have sleep problems, they can be treated. Sometimes fatigue can be a sign;of depression, which may be helped by counseling and/or medicines.
What Are The Most Common Side Effects
The most common side effects of PERJETA when given with Herceptin and chemotherapy as part of an early breast cancer regimen before surgery are:
- Constipation
- Damage to the nerves ;
- Diarrhea
- Low levels of red blood cells;
- Low levels of white blood cells with or without fever;
- Low platelet count;
- Weakness;
Side effects may vary based on chemotherapy regimen.
The most common side effects of PERJETA when given with Herceptin and chemotherapy as part of an early breast cancer regimen after surgery are:
- Diarrhea;
- Damage to the nerves
- Vomiting
The most common side effects of PERJETA when given with Herceptin and docetaxel for treatment of breast cancer that has spread to other parts of the body are:
- Diarrhea
- Low levels of white blood cells with or without fever
- Nausea
You May Like: Where To Buy Breast Cancer Merchandise
Estrogen Receptor Blockers Estrogen Receptor Blocker Drugs Attach Directly To And Block The Estrogen Receptors On Cancer Cells So That The Cancer Cells Cant Use Estrogen They Do Not Affect The Level Of Estrogen In The Body Estrogen Receptor Blockers Are Also Called Selective Estrogen Receptor Modulators
Tamoxifen
Tamoxifen is the most commonly used anti-estrogen drug. It is used in post-menopausal and premenopausal women. Tamoxifen is given by mouth as a pill.
Tamoxifen is the hormonal therapy drug used most often to lower the risk that DCIS or LCIS will lead to an invasive breast cancer.
Tamoxifen very slightly increases the risk for uterine cancer, deep vein thrombosis and stroke. Doctors will carefully weigh these risks against the benefits of giving this drug before they offer it to women who have a personal or a strong family history of these conditions. Usually the benefits of taking tamoxifen outweigh these risks.
Fulvestrant
Fulvestrant is an anti-estrogen drug that reduces the number of estrogen receptors on breast cancer cells. It is given as an injection into the muscles of the buttocks.
Fulvestrant is used in post-menopausal women if the breast cancer has grown after they were treated with tamoxifen. It is also used in postmenopausal women with locally advanced or metastatic breast cancer that have never been treated with hormonal therapy.
Third Generation Chemotherapy Regimens
Docetaxel, doxorubicin, and cyclophosphamide
Unlike paclitaxel, docetaxel does not have a major pharmacokinetic interaction with doxorubicin, and does not increase doxorubicin-related cardiotoxicity when given concurrently . Two studies compared a combination of docetaxel, doxorubicin, and cyclophosphamide with FAC . The Breast Cancer International Research Group 0001 trial compared six cycles DAC with FAC every 3;weeks as adjuvant treatment for 1,491 women with operable node-positive breast cancer . After a median follow-up of 124;months, there were improvements in DFS and OS . The benefit in DFS was irrespective of nodal, hormone receptor, and HER2 status. The GEICAM 9805 trial compared six cycles of DAC with FAC in 1,060 patients with node-negative breast cancer . After a median follow-up of 77;months, there was a significant improvement in DFS and a trend toward improved OS favoring DAC. In both trials, DAC was associated with considerably more toxicity, including febrile neutropenia.
Sequential FEC-taxane therapy
Dose dense sequential doxorubicin/cyclophosphamide-paclitaxel
Sequential AC-weekly paclitaxel or every 3;week docetaxel
Sequential versus concurrent taxane administration
Predicting benefit from chemotherapy
Don’t Miss: What Are Signs Of Breast Cancer In Males
Side Effects Experienced By Women
Menstrual cycle changes
Some treatments may cause your periods to change , become irregular, or stop. Your treatment plan may also include medication or surgery that will stop your periods.
- If you still have ovaries and a uterus, you can still be ovulating and can get pregnant, even if your periods stop. If you have ovaries and a uterus, you must use a non-hormonal form of birth control such as a condom, diaphragm, or non-hormonal IUD during your treatment.
- Read the resource Sex and Your Cancer Treatment for more information.
Vaginal dryness
Many women have vaginal dryness after menopause or from hormonal treatments. This can make penetrative sex painful or difficult. It can also make it easier to get urinary tract infections .
What you can do to help with vaginal dryness:
- Use vaginal moisturizers regularly, such as Replens®, K-Y®, Silk-E®, or Vitamin E gel caps.
- Use lubricants during sexual activity to reduce discomfort.
- Use water-based lubricants, such as Astroglide®, K-Y® Jelly, or Liquid Silk.
Addition Of Cyclin Dependent Kinase Inhibitors To Adjuvant Endocrine Therapy
Recently, the phase 3 Palbociclib Collaborative Adjuvant Study and monarchE adjuvant trials testing different CDKis in endocrine receptorpositive/HER2-negative breast cancer have reported results. The PALLAS trial investigated a primary endpoint of invasive DFS for patients who received standard endocrine therapy alone or in combination with the CDK4/6 inhibitor palbociclib for 2 years. PALLAS was a multicenter open-label randomized trial that studied patients with stage II or III breast cancer. A preplanned analysis was performed, and the PALLAS trial was stopped because of futility . The monarchE trial also measured a primary endpoint of IDFS for patients who received standard endocrine therapy alone or in combination with the CDK4/6 inhibitor abemaciclib for 2 years. monarchE is a multicenter open-label randomized trial that studies a population of patients at high risk for recurrence with four or more pathologically positive lymph nodes or one to three lymph nodes and high-risk features such as primary tumor of at least 5 cm, grade 3 tumor, or Ki67 of at least 20%. monarchE showed a significant improvement in IDFS with abemaciclib and endocrine therapy versus endocrine therapy alone with respective IDFS rates of 92.2% versus 88.7% at 2 years. The monarchE paper and the PALLAS trial press release indicate a difference between CDKi types in the adjuvant setting. Whether there are differences between CDKis in the neoadjuvant setting remains to be seen.
Recommended Reading: Is Breast Cancer Curable In The 3 Stage
Adjuvant Breast Cancer Treatments
Radiotherapy , antihormonal treatment , and chemotherapy were the most common modalities of adjuvant anticancer therapy. There were some inconsistencies in the reports on antihormonal therapies: 16% of the patients reported an antihormonal therapy despite having stated an absence of hormone receptor positivity; 6% received an antihormonal drug despite having reported no antihormonal treatment. Therefore, a total of 78% probably had a hormone receptor-positive breast cancer.
Taxanes , anthracyclines , and cyclophosphamide were the most commonly used chemotherapeutics.
A total of 18% of all patients reported to have received HER2-directed therapies; this includes 80% of the patients with HER2 3+ positive status and 24% of those with HER2 0-2+ status.
In the subgroup of patients treated with antihormonal drugs, tamoxifen and aromatase inhibitors were the most commonly used substances .
Table;2
Drugs used for anticancer treatment