Proteins For Targeted Cancer Drugs
Testing cancer cells for particular proteins can help to show whether targeted drug treatments might work for your breast cancer.
Targeted cancer drugs are treatments that change the way cells work and help the body to control the growth of cancer.
Some breast cancers have large amounts of a protein called HER2 receptor . They are called HER2 positive breast cancers. About 15 out of every 100 women with early breast cancer have HER2 positive cancer.
Targeted cancer drugs such as trastuzumab can work well for this type of breast cancer. These drugs attach to the HER2 protein and stop the cells growing and dividing.
Determining Your Her2 Status
A breast biopsy is used to determine HER2 status. The biopsy can be sent for laboratory testing with an immunohistochemistry test. The fluorescence in situ hybridization test looks for the HER2 gene in breast cancer cells.
The results of an immunohistochemistry test show different levels of HER2 positivity. For example, a tumor may be reported as 0, 1+, 2+, or 3+. Tumors with a higher number may be referred to as having an overexpression of HER2.
According to the American Cancer Society, immunohistochemistry test results should be considered as follows:
| Designation | |
|---|---|
| Equivocal | |
| 3+ | HER2-positive |
The impact of being HER2-positive on breast cancer survival is, of course, a top concern. Unfortunately, statistics can be misleading without considering other aspects of your diagnosis, including cancer stage at diagnosis and whether the tumor is also estrogen and/or progesterone receptor-positive.
With this in mind, you may also be tested for progesterone and estrogen receptors. Triple-negative breast cancers are negative for HER2, estrogen, and progesterone, while triple-positive breast cancers are positive for all three.
How Does Her2 Positive Breast Cancer Develop
While we are still learning about the causes of HER2 positive breast cancer, researchers have identified how HER2 positive breast cancer develops. In about 25 percent of breast cancers, the cancer cells have an excess of the HER2 protein. This is caused by a mutation in the HER2 gene. When the HER2 gene mutates, it causes cells in the breast to grow and divide at an uncontrolled rate, leading to tumor growth.
You May Like: Side Effects Of Hormone Blockers For Breast Cancer
Will I Ever Be Cured
Oncologists dont talk about curing stage 4 breast cancer as much as managing it as you would other chronic diseases, according to Brufsky. Were not likely going to get rid of every single bit of cancer, but were learning that people can live with this disease and be asymptomatic for years and years, he explains. While the mean survival of patients with HR-positive/HER-2-negative metastatic breast cancer is now over five years, its hard to say what the future holds for a woman diagnosed with the disease today. The field is changing so quickly and dramatically that in two or three years, this will be a different conversation.
Immunohistochemistry: Er Pr And Her2
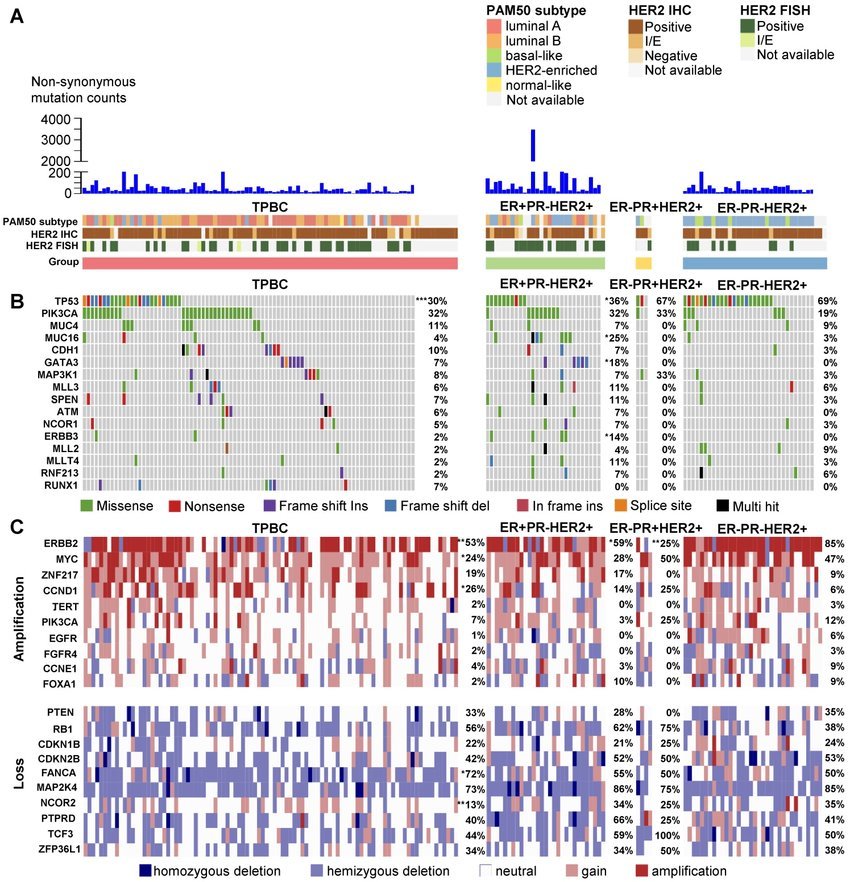
Via the characterization of ER, PR, and HER2 status, we can divide BC in three phenotypes or entities. Hormone receptor-positive breast cancers are defined as positive by expression of ER and/or PR receptor equal to 1% or higher of invasive cancer cells . ER and PR receptors are expressed around 80 and 65% of breast cancers, respectively . Although estrogen receptor-positive tumors co-express PR in the majority of breast cancers, some cases are ER+/PR and less frequently, ER/PR+. The response to hormonal therapy seems to be major in breast tumors with positivity for ER and PR, with lower rates in ER+/PR and ER/PR+ tumors .
Even so, this current and basic classification of human breast tumors presents a number of important limitations. The main one is the variability in therapeutic response and clinical outcomes, even for tumors with similar clinical and pathological features. Secondly, this classification provides limited knowledge into the biology and the molecular pathways that divide the BC in distinct subtypes and stages, stepping away from the personalized treatment paradigm.
Recommended Reading: Can Nipple Piercings Cause Breast Lumps
How Are Breast Tumors Tested For Her2
Either a test called an immunohistochemistry test or fluorescence in situ hybridization test is used to find out if cancer cells have a high level of the HER2 protein.
See Testing Biopsy and Cytology Specimens for Cancer and Understanding Your Pathology Report: Breast Cancerto get more details about these tests.
When Herceptin Is Used
Herceptin can be used to treat:
- early-stage HER2 positive breast cancer, following surgery and/or radiotherapy and chemotherapy, to reduce the risk of the cancer coming back
- advanced HER2 positive breast cancer that has spread from the breast , to slow the growth of the cancer and increase survival time
- advanced HER2 positive stomach cancer that has spread out of the stomach
- advanced HER2 positive gastro-oesophageal cancer, which affects where the food pipe meets the stomach
If you have breast, oesophageal or stomach cancer, you will have tests to check if the cancer is HER2 positive before herceptin is offered.
Read Also: What Is Stage 3 Cancer Mean
Portrait Of A Scientist
Portrait of a Scientist
For over 30 years, Genentech has been working on the science of the HER2 gene. Senior Scientist Gail Lewis Phillips has had a unique vantage point, having begun her career at Genentech in 1985. We asked Illustrator Wendy MacNaughton to visit Gail at Genentech and explore the story behind the science.
Starting With Neoadjuvant Therapy
Most often, these cancers are treated with neoadjuvant chemotherapy. For HER2-positive tumors, the targeted drug trastuzumab is given as well, often along with pertuzumab . This may shrink the tumor enough for a woman to have breast-conserving surgery . If the tumor doesnt shrink enough, a mastectomy is done. Nearby lymph nodes will also need to be checked. A sentinel lymph node biopsy is often not an option for stage III cancers, so an axillary lymph node dissection is usually done.
Often, radiation therapy is needed after surgery. If breast reconstruction is planned, it is usually delayed until after radiation therapy is done. For some, additional chemo is given after surgery as well.
After surgery, some women with HER2-positive cancers will be treated with trastuzumab for up to a year. Many women with HER2-positive cancers will be treated first with trastuzumab followed by surgery and then more trastuzumab for up to a year. If after neoadjuvant therapy, any residual cancer is found at the time of surgery, ado-trastuzumab emtansine may be used instead of trastuzumab. It is given every 3 weeks for 14 doses. For women with hormone receptor-positive cancer that is in the lymph nodes, who have completed a year of trastuzumab, the doctor might also recommend additional treatment with an oral targeted drug called neratinib for a year.
Don’t Miss: Stage Iiii Cancer
What Is The Grade Of My Tumor
Grading is not the same as staging. Both are indicators of a cancers severity and prognosis, but they use different criteria. Staging deals with the tumor size, location and the distribution of cancer cells in your body. But grading is based on how the cancer cells appear under a microscope.
The more abnormal-looking the cells are, the more likely they are to quickly grow and spread. Grades usually run from I to III. A higher grade is a more aggressive cancer. Its possible to have a Stage I tumor thats also a Grade III cancer.
Understanding Her2 Status In Breast Cancer
Sharing is caring!
HER2 is a protein receptor. Normally, this protein helps breast cells to grow, divide, and repair themselves. But sometimes, some changes occur in the genes that controls the HER2 protein and make the cells grow in a cancerous manner.
If your healthcare provider suspects cancer presence in your mammogram, biopsy or breast MRI, they will first try to identify the type of breast cancer. This information will be the key to understand cancer behaviour and in determining treatment plans.
Read Also: Estrogen Receptor Negative Breast Cancer Prognosis
Recommended Reading: Stage 3 Ductal Carcinoma Prognosis
Who May Not Be Able To Have Herceptin
Herceptin should not be used to treat people with breast, oesophageal or stomach cancer that is not HER2 positive.
It may also not be suitable if:
- you have a pre-existing heart condition, such as heart failure, severe angina or a problem with your heart valves
- you have poorly controlled high blood pressure
- you’re pregnant
- you’re breastfeeding
Avoid becoming pregnant while taking herceptin and for at least 7 months after treatment stops, as it could harm your developing baby.
Also avoid breastfeeding until at least 7 months after treatment stops, as the medicine can enter breast milk and may be harmful for babies.
The Overall Hormone Receptor Status Of A Breast Tumor Helps Predict Behaviour And Responsiveness To Treatment
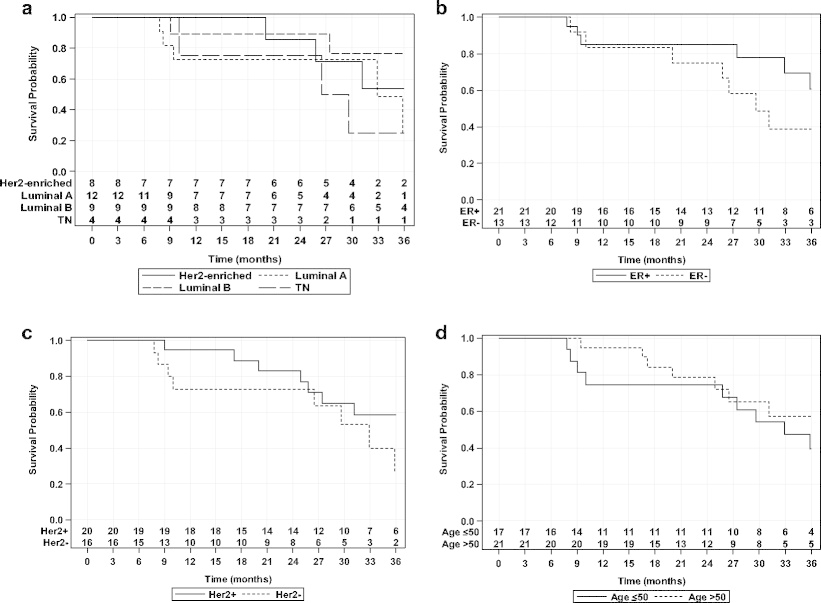
Indeed, specialists consider the hormone-receptor status of a tumor to be more of a predictive factor rather than a prognostic factor. It helps determine what you are up against, and how best to treat it.
However, research shows that the outlook for a particular breast cancer is more likely to be influenced by the histological type and grade of the breast cancer tumor at the time of discovery.
Also, whether or not there is lymphatic involvement is another important factor, and not the hormone receptor status.
It is true, however, that breast cancer tumors with a positive hormone receptor status have a more indolent course than do hormone receptor-negative tumors.
Indolent is kind of a strange term to use, but it means that a tumor is less responsive or lazy in response to treatment than hormone negative receptor status tumors. Some kind of extra intervention or boost is often necessary to really get a positive healing response from cancer.
However, the good news is that certain kinds of hormone-receptor-positive tumors are actually more responsive to endocrine therapy. So, there is a positive aspect to this as well.
In fact, there is often a kind of inverse relationship between the HER-2 hormone receptor status, and the ER and PR status of a tumor.
You May Like: Chemotherapy For Breast Cancer Stage 3
High Tumor Responses With Trastuzumab Deruxtecan
The DESTINY-Breast01 trial was not a randomized study, so all patients in the trial received trastuzumab deruxtecan.
Nearly all of the more than 180 women in the trial had at least some reduction in the size of their tumors, with 61% experiencing substantial reductions, Dr. Krop reported. Several patients had no evidence of cancer following treatment, known as a complete response. The median progression-free survival was more than 16 months.
Dr. Krop called the results compelling, noting that the tumor response rate is roughly double or triple what we typically see in other studies of this third- or later-line population.
Most of the treatment-related side effects seen in the trial were mild, Dr. Krop said. Even so, 15% of the participants stopped taking the drug because of side effects. Nearly all of these women were those who experienced ILD. Four of the women who developed ILD died as a result.
Why we have this particular risk is unclear, he said. And clearly we need to do more research to identify those patients who are at risk of getting the most severe cases of ILD and how to mitigate the risk.
For future studies of the drug, Dr. Krop said, clinicians will be advised to carefully monitor patients for any evidence or symptoms of ILD and, if they suspect it has developed, to immediately stop the drug and treat the patient with steroids.
We definitely have to be cautious, he continued. But I dont think is a major barrier to moving this drug forward.
How Kadcyla Is Thought To Work
Kadcyla is an antibody-drug conjugate, made up of Herceptin and a chemotherapy medicine attached by a stable linker.
In addition to helping block HER2 signaling and recruiting immune cells, once Kadcyla is internalized by the cell, the chemotherapy is released, helping to destroy the cell.
Because HER2 is present in all cells, Kadcyla may also affect healthy cells.
Following that discovery, in collaboration with Massachusetts-based ImmunoGen, the medicine that would become Kadcyla was born. Results of the Phase III EMILIA trial that led to its FDA approval in 2013 showed that it helped give certain people with HER2-positive metastatic breast cancer more time before their cancer got worse and extended their lives by almost six months compared to a standard treatment, at the time of the trial.42-44
People receiving Kadcyla in the trial still experienced severe side effects, including nerve problems, low levels of red blood cells, tiredness, liver problems, pain, bleeding and constipation. Kadcyla also has boxed warnings for potential heart and liver damage, can also harm an unborn baby and must not be substituted for Herceptin.
Don’t Miss: Is Breast Cancer Curable
Triple Negative Breast Cancer
Triple negative breast cancers don’t have oestrogen receptors, progesterone receptors or HER2 receptors. Around 15 out of 100 women have this type . It is more common in younger women.
Hormone therapies and targeted cancer drugs do not work well for this type of breast cancer. So you are more likely to have chemotherapy.
Histopathological Subtypes: Morphologic Heterogeneity
The histopathological classification of BC is set by the 2012 World Health Organization . Most of the breast cancers are adenocarcinomas, with around 7080% defined as invasive ductal carcinomas not otherwise specified . The rest, around 2530%, are characterized by histological special types such as papilar, metaplastic, cribiform, apocrine, or mucinous carcinomas, among others . The majority of special types is rare and differ strongly about prognosis and response to the treatments . The tumor grade is the other important intrinsic characteristic of tumoral heterogeneity .
Read Also: Breast Cancer Recurrence Symptoms Pain
There Are Several Targeted Therapy Options Available
Doru Paul, MD, is triple board-certified in medical oncology, hematology, and internal medicine. He is an associate professor of clinical medicine at Weill Cornell Medical College and attending physician in the Department of Hematology and Oncology at the New York Presbyterian Weill Cornell Medical Center.
If you have HER2-positive breast cancer, your options for treatment will depend on several factors, such as the stage of cancer and the hormone receptor status of the tumor.
HER2-positive tumors can also be estrogen-receptor-positive . However, a tumor’s receptor status can change . Therefore, the treatment plan your oncologist recommends might change as well.
Breast Cancer Doctor Discussion Guide
Get our printable guide for your next doctor’s appointment to help you ask the right questions.
It’s believed that around 20-25% of newly diagnosed cases of breast cancers are positive for a genetic mutation that causes HER2 gene amplification. The mutation causes the gene to produce too many HER2/neu proteins .
In normal amounts, these proteins act as receptors that tell the breast cells how much to grow . When the mutation is present, the overproduction of HER2 proteins drives the growth of breast cancer cells.
Therapies that specifically target HER2 include Herceptin , Perjeta , and T-DM1 which is sold under the brand nameKadcycla.
Verywell / Ellen Lindner
What Does Testing Involve
If a doctor confirms an unusual growth, they will take a biopsy. To collect a sample, they may perform one of the following procedures:
- Use a fine needle to remove a sample of breast cells or a liquid in fine-needle aspiration.
- Use a larger needle in a core needle biopsy.
- Carry out minor surgery as an outpatient procedure.
According to the American Cancer Society , a core needle biopsy is often the preferred option.
The doctor will send the tissue samples to a laboratory to test whether or not breast cancer is present. If it is, the pathologist will test to see if the cancer is HER2-positive.
The two main tests for determining whether or not HER2-positive cancer is present are the fluorescent in situ hybridization test and the immunohistochemistry test.
The FISH test looks for additional copies of the HER2 gene in breast cancer cells. It uses special labels that attach to the HER2 proteins that glow in the dark.
The IHC test uses a chemical dye to stain HER2 proteins and can determine how much HER2 protein is present in breast cancer cells.
Often, the pathologist will carry out the IHC test and then the FISH test. IHC testing is faster and less costly than FISH testing. However, if the results of the IHC test are unclear, a person will need a FISH test to determine whether or not a tumor is HER2-positive.
Also Check: Hormone Therapy Metastatic Breast Cancer
Current Classification Of Breast Cancer
Intertumoral heterogeneity of BC is initially illustrated with a clinical staging of the disease. The TNM staging system by the American Joint Committee on Cancer and Union for International Cancer Control adds information about tumor features such as size, regional lymph-node involvement or the presence of distant metastases . After the clinical diagnosis, the first step is the assessment of histological criteria on the primary tumor obtained by surgery and/or a core biopsy, encompassing morphology-base and immunohistochemical analyses for testing the biomarker profile. This is a classical and non-molecular classification of BC, and sets the standard in the usual clinical practice. Classic pathological criteria, such as histological type, tumor size, grade and axillary lymph node status, are relevant for the initial prognostic evaluation . The expression of hormone receptors by IHC and the overexpression and/or amplification of HER2 by IHC and/or ISH gives additional predictive value, being elementary for guiding algorithms of treatment , as will be discussed in the following two sections.
Iv Optimal Combinations Of Her
Because HER-2 inhibitors are indispensible for breast cancer treatment, the interaction between HER-2 inhibitors and anti-cancer agents needs to be considered for treating HER-2 subtypes of breast cancer. Preclinical data available on these combinations can be used to determine rational combinations of trastuzumab with other chemotherapeutic drugs. The interaction between trastuzumab and anti-cancer drugs in HER-2-overexpressing breast cancer cell lines was examined in one study, which showed that the anthracyclines, doxorubicin and epirubicin acted additively with trastuzumab . A randomized clinical trial demonstrated that doxorubicin-based chemotherapy combined with trastuzumab showed better results than chemotherapy alone. However, cardiotoxicity was observed clinically, which was not predicted in preclinical studies. Thus, the concurrent use of anthracyclines and trastuzumab is not practical.
Mean combination index values for anticancer drugtrastuzumab combinations
Don’t Miss: Stage 3 Ductal Carcinoma