Treatment Options For Her2 Positive Breast Cancer Tumors
Treating doctors will usually offer women with HER-2 positive breast treatment with Trastuzumab .
Indeed, this is the only therapy that the US Food and Drug Administration approvesfor women with breast cancer tumors over-expressing HER-2 proteins.
It is often the case that women with HER2 breast cancer tumors do not respond to Tamoxifen therapy.
But, the use of trastuzumab in combination with chemotherapy has led to longer survival rates for women with metastatic HER-2 positive breast carcinomas.
The addition of Herceptin when HER-2 is positive gives an amazing boost to the response and cure rates.
How Does Her2 Status Affect Breast Cancer Treatment
HER2-positive result could mean your healthcare provider will treat it with different means than other breast cancer types. The treatment plans are also influenced by the stage of the cancer . Generally, a HER2-positive cancer is metastatic , where it spreads to other parts from its origin. However, early detection can make treatments effective and improve the outlook for cancer and increase survival rates.
Following are some of the treatment options:
HER2-positive result could mean your healthcare provider will treat it with different means than other breast cancer types. The treatment plans are also influenced by the stage of the cancer . Generally, a HER2-positive cancer is metastatic , where it spreads to other parts from its origin. However, early detection can make treatments effective and improve the outlook for cancer and increase survival rates.
Following are some of the treatment options:
Survival Analysis Of Single Hormone Receptor
Approximately 97% of patients with ER + PR- tumors and 88% of patients with ER-PR+ tumors received endocrine therapy. More patients with ER + PR- and ER-PR+ tumors received chemotherapy than the group with ER + PR+ tumors , but less than the group with ER-PR- tumors . Approximately 72% of patients with ER + PR- tumors received both endocrine therapy and chemotherapy, and 24.9% of patients received only endocrine therapy. In ER-PR+ tumors, 80% of patients received both chemotherapy and endocrine therapy, 8.2% of patients received only endocrine therapy and 9.4% of patients received only chemotherapy.
With univariate analysis by Kaplan-Meier method, the survival graph of ER + PR- tumors was located between that of ER + PR+ tumors and ER-PR- tumors. The 5-year and 10-year DFS of ER + PR- tumors was 91.4% and 79.6%, respectively, and the 5-year and 10-year OS was 95.9% and 93.9%, respectively. Patients with ER-PR+ tumors had worse DFS and OS than those with ER + PR-.
Figure 1
Among 1,376 patients with HER2 overexpression, there was no significant difference in DFS between four subgroups , and patients with ER-PR-HER+ tumors had the worst OS . However, the 790 patients who received trastuzumab therapy had similar OS , as did the 586 patients who did not receive trastuzumab therapy .
Figure 2Figure 3Table 2 Multivariate analysis of disease-free survival and overall survival in 1.376 women with HER2-positive breast cancer
Read Also: How Long Can U Live With Stage 4 Cancer
Should I Have Breast Reconstruction And When
This is another question that has a multi-layered answer. It involves both medical and personal considerations. Some women opt not to have reconstruction. Others believe it benefits their appearance and psychological recovery.
This is another question that has a multi-layered answer. It involves both medical and personal considerations. Some women opt not to have reconstruction. Others believe it benefits their appearance and psychological recovery.
If youre having one or both breasts removed and are considering reconstruction, the stage of your cancer may dictate the timing of the reconstructive surgery. For patients with early-stage breast cancer, Dr. Abraham says immediate reconstruction is reasonable. With a Stage III cancer, you should discuss with your oncologist and surgeon whether immediate reconstruction is advisable.
Understanding Her2 Status In Breast Cancer
Sharing is caring!
HER2 is a protein receptor. Normally, this protein helps breast cells to grow, divide, and repair themselves. But sometimes, some changes occur in the genes that controls the HER2 protein and make the cells grow in a cancerous manner.
If your healthcare provider suspects cancer presence in your mammogram, biopsy or breast MRI, they will first try to identify the type of breast cancer. This information will be the key to understand cancer behaviour and in determining treatment plans.
Read Also: Estrogen Receptor Negative Breast Cancer Prognosis
What Is My Estrogen Receptor And Progesterone Receptor Status
Your bodys hormones such as estrogen and progesterone may play a role in how your breast cancer progresses.
Normal cells are equipped with receptors that allow them to receive information from circulating hormones, similar to the way your phone picks up satellite signals. Cancer cells may also have hormone receptors, letting them tap into your bodys normal cell growth-regulating system.
Your ER/PR status is determined by testing a sample of breast cancer cells removed during a biopsy. If your breast cancer cells have estrogen and progesterone receptors if theyre ER/PR-positive then theyre capable of detecting estrogens signal and using it to fuel growth. If the cancer cells lack these receptors meaning theyre ER-/PR-negative they cant hear the growth-signaling message.
About 70% of breast cancer patients have positive ER/PR hormone status.
While being ER/PR-positive sounds bad, theres actually a benefit. Doctors can take advantage of the receptors presence. They can use an anti-estrogen drug that blocks the receptors and blocks estrogens growth signal. Or they can use other drugs like aromatase inhibitors that lower your bodys estrogen levels to deprive the cancer cells of fuel.
What Is My Her2 Status
HER2 is another type of growth signal receptor which may be present on your breast cancer cells. About 25% of breast cancers are HER2-positive. HER2-positive cancers are a mix of good and bad news.
The bad news is the tumors tend to grow more aggressively than those without the HER2 receptor. The good news is that like ER/PR-positive cancers, medicines can switch the HER2 growth receptor off.
New drugs such as trastuzumab, pertuzumab, T-DM1 and lapatinib are extremely effective at this and have dramatically improved the prognosis for HER2-positive patients, Dr. Abraham says. Treatment outcomes are now as good as those with HER2-negative tumors.
But HER2-positive tumors bigger than half a centimeter or that have spread into the lymph nodes may require treatment with chemotherapy and one of the medicines specifically targeting the HER2 receptor, such as trastuzumab.
Recommended Reading: Breast Cancer Medications After Surgery
If I Have Chemotherapy Will I Need To Take Other Medications Like Trastuzumab
If your breast cancer is HER2-positive, its recommended that you take trastuzumab for one year, Dr. Abraham says. This ensures that the HER2 growth receptor on any remaining cancer cells stays shut off. Trastuzumab is not chemotherapy. The hair you lost during chemotherapy will regrow and your energy level will improve while youre taking trastuzumab.
Why Receptor Status Matters
Breast cancer is not a single disease, and researchers now have the ability to break down breast cancer into different subtypes based on the receptor status of the tumors. Among the variations between different types of breast cancers are the proteins found on cell surfaces, which are involved tumor growth. These proteins are related to the genetic material of cancer cells.
For example, with estrogen receptor-positive breast cancer, estrogen binds to specific receptors on breast cancer cells, stimulating proliferation. Similarly, HER2 receptors on the surface of breast cancer cells are stimulated by HER2 protein, promoting the growth and spread of breast cancer.
It’s important to note, however, that all breast cellsboth cancerous and noncanceroushave HER2 receptors on their surfaces. The difference is that HER2-positive breast cancer cells have 40 to 100 times more receptors than HER2-negative breast cancer cells or normal breast cells. In positive cases, the abundance of receptors fuels the cancer.
Breast Cancer Discussion Guide
Get our printable guide for your next healthcare provider’s appointment to help you ask the right questions.
Also Check: Can You Get Breast Cancer From Nipple Piercing
Will I Ever Be Cured
Oncologists dont talk about curing stage 4 breast cancer as much as managing it as you would other chronic diseases, according to Brufsky. Were not likely going to get rid of every single bit of cancer, but were learning that people can live with this disease and be asymptomatic for years and years, he explains. While the mean survival of patients with HR-positive/HER-2-negative metastatic breast cancer is now over five years, its hard to say what the future holds for a woman diagnosed with the disease today. The field is changing so quickly and dramatically that in two or three years, this will be a different conversation.
Hormone Receptor Status And Early Breast Cancer Prognosis
Hormone receptor status is related to the risk of breast cancer recurrence.
Hormone receptor-positive tumors have a slightly lower risk of breast cancer recurrence than hormone receptor-negative tumors in the first 5 years after diagnosis .
After about 5 years, this difference begins to decrease and over time, goes away .
|
For a summary of research studies on hormone receptor status and survival, visit the Breast Cancer Research Studies section. |
Don’t Miss: Stage Iii A Cancer
Stage The Stage Is The Main Prognostic Factor For Breast Cancer There Is Less Risk That Early Stage Breast Cancer Will Come Back So It Has A More Favourable Prognosis Breast Cancer Diagnosed At A Later Stage Has A Greater Risk Of Recurrence So It Has A Less Favourable Prognosis Doctors Will Consider If Cancer Has Spread To Lymph Nodes And The Size Of The Tumour When They Predict A Prognosis
If cancer has spread to lymph nodes
Whether or not cancer has spread to lymph nodes is the most important prognostic factor for breast cancer. Breast cancer that has spread to lymph nodes has a higher risk of coming back and a less favourable prognosis than breast cancer that has not spread to the lymph nodes.
The number of lymph nodes that contain cancer is also important. The more positive lymph nodes there are, the higher the risk that breast cancer will come back. Breast cancer that has spread to 4 or more lymph nodes has the highest risk for recurrence.
The size of the tumour
The size of the tumour is the 2nd most important prognostic factor for breast cancer. The tumour size will affect prognosis no matter how many lymph nodes have cancer in them.
Breast tumours that are 5 cm or larger are more likely to come back after treatment than smaller tumours. Breast tumours that are smaller than 1 cm and have not spread to the lymph nodes have a very favourable prognosis.
The Overall Hormone Receptor Status Of A Breast Tumor Helps Predict Behaviour And Responsiveness To Treatment

Indeed, specialists consider the hormone-receptor status of a tumor to be more of a predictive factor rather than a prognostic factor. It helps determine what you are up against, and how best to treat it.
However, research shows that the outlook for a particular breast cancer is more likely to be influenced by the histological type and grade of the breast cancer tumor at the time of discovery.
Also, whether or not there is lymphatic involvement is another important factor, and not the hormone receptor status.
It is true, however, that breast cancer tumors with a positive hormone receptor status have a more indolent course than do hormone receptor-negative tumors.
Indolent is kind of a strange term to use, but it means that a tumor is less responsive or lazy in response to treatment than hormone negative receptor status tumors. Some kind of extra intervention or boost is often necessary to really get a positive healing response from cancer.
However, the good news is that certain kinds of hormone-receptor-positive tumors are actually more responsive to endocrine therapy. So, there is a positive aspect to this as well.
In fact, there is often a kind of inverse relationship between the HER-2 hormone receptor status, and the ER and PR status of a tumor.
Read Also: Left Breast Cancer Symptoms
How Is This Cancer Treated
Your treatment plan will depend on where the cancer has spread, the extent of the disease, other medical conditions you have, and your age and menopause status. Common therapies include:
- Ovarian suppression For premenopausal women with metastatic breast cancer of this type, hormone therapy almost always begins with ovarian suppression by means of surgery to remove the ovaries or drugs, such as goserelin or leuprolide, that stop the ovaries from producing hormones, says Brufsky. Ovarian suppression lowers hormone levels in the body so the tumor cant get the estrogen it needs to grow.
- Aromatase inhibitors Postmenopausal women and premenopausal women who have undergone removal or suppression of their ovaries are often treated with AIs, such as anastrozole, exemestane, and letrozole. These drugs block the activity of the enzyme aromatase, which the body uses to make estrogen in the adrenal glands and fat tissue. This means less estrogen is available to stimulate the growth of HR-positive breast cancer cells, according to the National Cancer Institute.
- CDK4/6 inhibitors These drugs, which include palbociclib, ribociclib, and abemaciclib, block proteins in the cell known as cyclin-dependent kinases . CDKs regulate cell proliferation and growth and are often elevated in breast cancer, fueling uncontrolled growth of cancer cells. They are typically used in combination with AIs as a first-line treatment for HR-positive/HER-2-negative metastatic breast cancer, Brufsky says.
Addition Of Cyclin Dependent Kinase Inhibitors To Adjuvant Endocrine Therapy
Recently, the phase 3 Palbociclib Collaborative Adjuvant Study and monarchE adjuvant trials testing different CDKis in endocrine receptorpositive/HER2-negative breast cancer have reported results. The PALLAS trial investigated a primary endpoint of invasive DFS for patients who received standard endocrine therapy alone or in combination with the CDK4/6 inhibitor palbociclib for 2 years. PALLAS was a multicenter open-label randomized trial that studied patients with stage II or III breast cancer. A preplanned analysis was performed, and the PALLAS trial was stopped because of futility . The monarchE trial also measured a primary endpoint of IDFS for patients who received standard endocrine therapy alone or in combination with the CDK4/6 inhibitor abemaciclib for 2 years. monarchE is a multicenter open-label randomized trial that studies a population of patients at high risk for recurrence with four or more pathologically positive lymph nodes or one to three lymph nodes and high-risk features such as primary tumor of at least 5 cm, grade 3 tumor, or Ki67 of at least 20%. monarchE showed a significant improvement in IDFS with abemaciclib and endocrine therapy versus endocrine therapy alone with respective IDFS rates of 92.2% versus 88.7% at 2 years. The monarchE paper and the PALLAS trial press release indicate a difference between CDKi types in the adjuvant setting. Whether there are differences between CDKis in the neoadjuvant setting remains to be seen.
You May Like: 3 Stage Of Cancer
Cumulative Incidences And Hazard Ratios Of Death From Any Cause And Metachronous Breast Cancer
Supplementary Table 12 shows cumulative incidences and hazard ratios for death from any cause. During follow-up, 5416 women died of any cause. In the full regression models, old age at diagnosis , being postmenopausal vs premenopausal at diagnosis , and higher tumor grade were associated with a higher risk of death from any cause . The pattern of better shorter-term but similar longer-term prognosis for ER-positive vs ER-negative tumors was evident also when death from any cause was the outcome . None of the patient or tumor characteristics were associated with risk of metachronous breast cancer .
Options For Luminal Breast Cancer
with luminal or other types of HR-positive breast cancer receive hormone therapy. Some people call this endocrine therapy.
Triple-negative breast cancer does not respond to hormone therapy because it is HR-negative.
Anti-estrogen therapy
Anti-estrogen therapy works by preventing estrogen from attaching to the estrogen receptors of breast cancer cells.
The four different types of anti-estrogen therapy are:
- selective estrogen-receptor response modulators, such as tamoxifen
- aromatase inhibitors
- estrogen-receptor downregulators, such as fulvestrant
- luteinizing hormone releasing agents, including goserelin and leuprolide , prevent the ovaries from producing estrogen
The type of anti-estrogen therapy a person receives depends on various factors, including:
- the stage of the breast cancer
- whether the person has any other medical conditions
- whether the person has been through menopause
A person usually continues hormone therapy for at least .
Other hormone therapies
In some cases, HR-positive breast cancer may not respond to the above treatments. Consequently, a doctor may recommend one of the following hormone therapies for more advanced cancer:
- progestin medications, such as megestrol
- an anabolic steroid, such as fluoxymesterone
Targeted therapies
Targeted therapies focus on specific genetic mutations that play a role in a cancers growth and spread. These drugs are usually combined with hormone therapy.
Examples of CDK4/6 inhibitors include:
- abemaciclib
- palbociclib
- ribociclib
Don’t Miss: Chemotherapy For Invasive Ductal Carcinoma
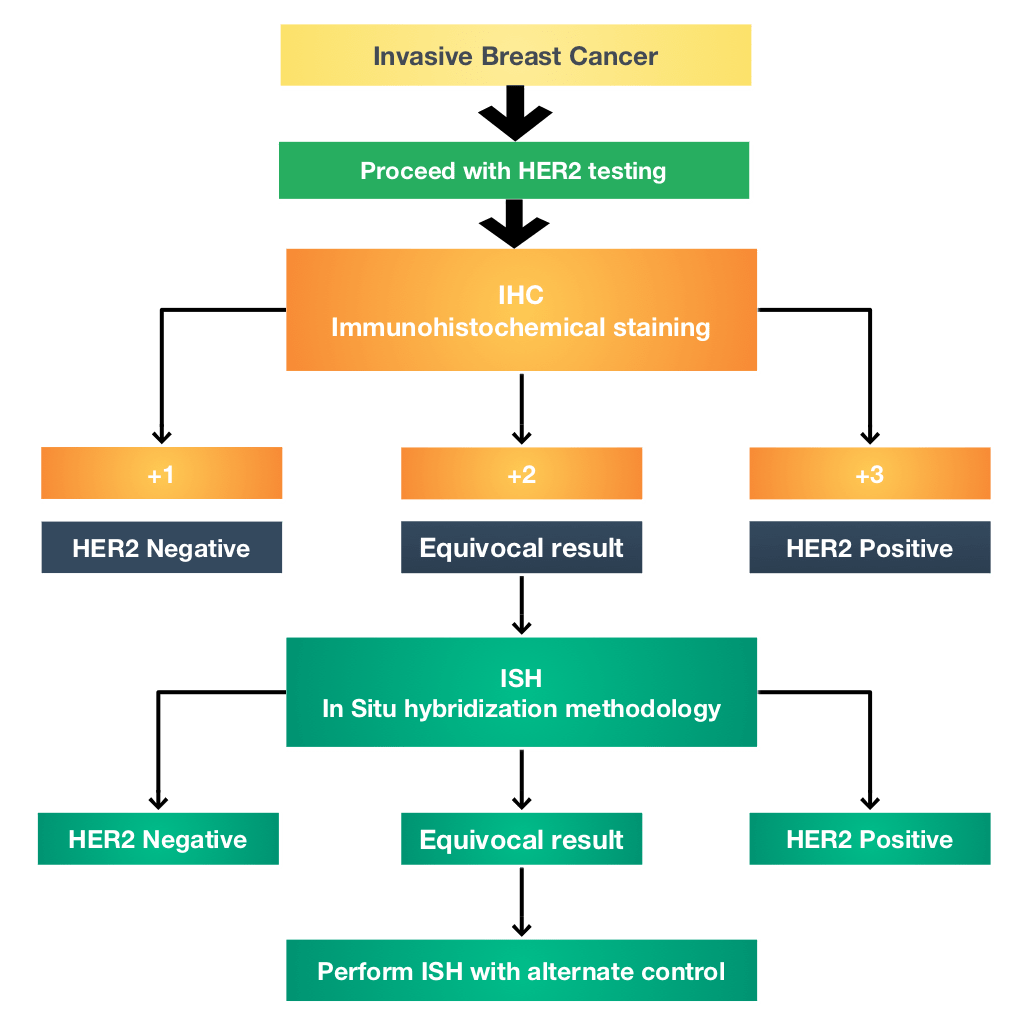
There Are Two Ways To Measure The Her
The most common way to measure the HER-2 status of a potential breast cancer tumor is through an immunohistochemistry test. This will likely be part of an overall histological/pathological evaluation of the tumor.
Various tumor markers, including the HER-2 status indicators, give the pathologist a characterization of the tumor. This helps to predict the future behavior and probable responses, of the tumor to different types of treatments.
The immunohistochemistry test of the HER-2 status measures the over-expression of a particular protein and is typically given a score of 0 to +3.
The pathologist actually counts the number of receptors on the surface of the cancer cells. Indeed, the pathologist can see the cells microscopically because they are receptive to certain protein-based dyes and change color.
Scores of 0 and +1 are indicative of a negative status , whilst +2 and +3 are HER-2 positive . There is no in-between state.