Lymph Node Metastasis May Be Slightly More Likely When Infiltration Is In Clusters
In the unlikely event of lymph node metastasis following the presentation of microinvasive ductal carcinoma, the prognosis for the patient tends to be mostly influenced by the number of metastatic nodes, irrespective of the absolute quantity of invasive carcinoma in the breast area. Some studies also suggest that lymph node metastasis, which is highly unlikely, is slightly more probable for microinvasive tumors in which the infiltration of the periductal stroma occurs by clusters of cells, rather than by single cells. But even with these clustered microinvasive formations, the risk of metastasis is at most about 10%.
Reproductive Factors And Steroid Hormones
Late age at first pregnancy, nulliparity, early onset of menses, and late age of menopause have all been consistently associated with an increased risk of breast cancer. Prolonged exposure to elevated levels of sex hormones has long been postulated as a risk factor for developing breast cancer, explaining the association between breast cancer and reproductive behaviors.
Clinical trials of secondary prevention in women with breast cancer have demonstrated the protective effect of selective estrogen receptor modulators and aromatase inhibitors on recurrence and the development of contralateral breast cancers. Use of SERMs in women at increased risk for breast cancer has prevented invasive ER-positive cancers. These data support estradiol and its receptor as a primary target for risk reduction but do not establish that circulating hormone levels predict increase risk.
A number of epidemiologic and pooled studies support an elevated risk of breast cancer among women with high estradiol levels. The Endogenous Hormones and Breast Cancer Collaborative Group reported a relative risk of 2.58 among women in the top quintile of estradiol levels.
A meta-analysis by the Collaborative Group on Hormonal Factors in Breast Cancer of 58 international studies that included 143,887 postmenopausal women with invasive breast cancer and 424,972 without breast cancer concluded the following about menopausal HRT and breast cancer :
Causes Of Invasive Ductal Carcinoma
The causes of invasive ductal carcinoma have not been conclusively established. Researchers have determined that cancer can form when the cells in a milk-producing duct undergo changes that cause them to grow uncontrollably, divide very rapidly or remain viable longer than they should. The result is an accumulation of excess cells that can form a mass or tumor and potentially spread to nearby lymph nodes and distant areas of the body. The underlying reason for those cellular changes, however, remains unclear.
Recommended Reading: Stage Iiia Cancer
What Breast Changes Happen At Puberty
As a girl approaches her teen years, the first visible signs of breast development begin. When the ovaries start to produce and release estrogen, fat in the connective tissue starts to collect. This causes the breasts to enlarge. The duct system also starts to grow. Often these breast changes happen at the same that pubic hair and armpit hair appear.
Once ovulation and menstruation begin, the maturing of the breasts begins with the formation of secretory glands at the end of the milk ducts. The breasts and duct system continue to grow and mature, with the development of many glands and lobules. The rate at which breasts grow is different for each young woman.
| Female breast developmental stages |
|---|
| Mature adult breast. The breast becomes rounded and only the nipple is raised. |
Local Recurrence May Happen But Does Not Affect The Overall Outcome

Local recurrence is rare with microinvasive ductal carcinoma and factors associated with recurrence tend to be close surgical margins, breast conservation versus mastectomy, and a younger age. Local recurrence tends not to be a serious issue with microinvasive breast carcinoma, and tends to be treated and cured locally.
You May Like: Breast Duct Cancer Symptoms
Microvinvasive Breast Carcinoma Cells Are Often Comedotype
Microinvasive ductal carcinoma are frequently associated with a higher nuclear grade comedo type ductal carcinoma in situ. Other histologic subtypes of DCIS such as cribriform, papillary and solid, are thought to invade less frequently than comedo DCIS. If the microinvasive DCIS element comprises cells of either the solid, papillary, or cribriform pattern, the changes of lymph node metastasis are reduced even further.
What You Need To Know
- The risk of getting invasive ductal breast cancer increases with age: According to the American Cancer Society, about two-thirds of women diagnosed with IDC are age 55 or older.
- IDC can affect men.
- Without prompt treatment, invasive ductal carcinoma can spread to lymph nodes or blood vessels and metastasize throughout the body.
- Identifying characteristics of the tumor, such as whether or not the cells are sensitive to certain hormones, can help your doctor choose the best treatment.
Also Check: Mbc Metastatic Breast Cancer
Histological Analysis Of Suspected Microinvasive Dcis Tumors Can Help Clarify The Diagnosis
Since treatment for pure DCIS differs or may differ from DCIS with microinvasive status, identifying the smallest focus or foci of any invasive carcinoma is of some significance.
One of the histological hallmarks of microinvasive breast carcinoma is the presence of a dense lymphocytic infiltrate. Evidence of an inflammatory reaction is often part of the overall diagnosis of an aggressive, invasive situation, but the pathologist must be careful not to dismiss the finding as simply an inflammatory reaction possibly due to infection or other illness.
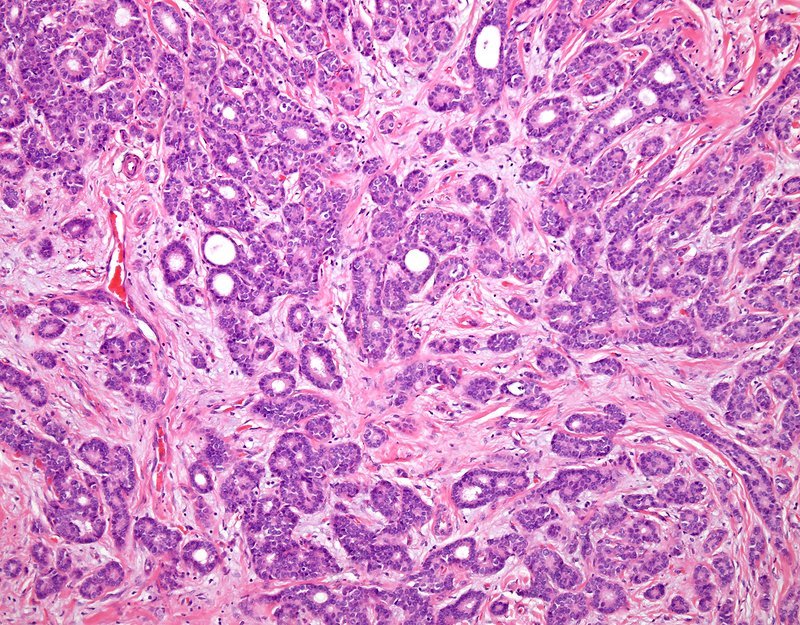
The microinvasive carcinoma element which has caused the inflammatory response might be very small, almost undetectable. However, invasive tumor cells are readily distinguished from inflammatory cells by cytokeratin AE1/3 immunostaining. In the microscopic image of microinvasive ductal carcinoma below, inflammatory cells mask the focus of invasive ductal carcinoma. Recent studies which highlight myoepithelial cells using antibodies to cytoskeletal proteins, or to the nuclear protein p63, , has also proven to be a useful histological tool in distinguishing invasive carcinoma from similar-appearing, benign breast diseases. False-positive diagnosis of microinvasive breast carcinomas often turn out later to be radial sclerosing lesions or sclerosing adenosis.
Grading Breast Cancer Cells
Three cancer cell features are studied and each is assigned a score. The scores are then added to get a number between 3 and 9 that is used to get a grade of 1, 2, or 3, which is noted on your pathology report. Sometimes the terms well differentiated, moderately differentiated, and poorly differentiated are used to describe the grade instead of numbers:
- Grade 1or well differentiated . The cells are slower-growing, and look more like normal breast tissue.
- Grade 2 or moderately differentiated . The cells are growing at a speed of and look like cells somewhere between grades 1 and 3.
- Grade 3or poorly differentiated . The cancer cells look very different from normal cells and will probably grow and spread faster.
Our information about pathology reports can help you understand details about your breast cancer.
Also Check: What Is The Latest Treatment For Melanoma
You May Like: Chemotherapy Cycles For Breast Cancer
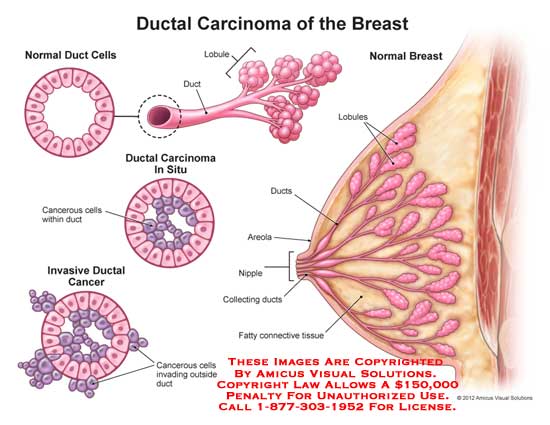
What Is Ductal Carcinoma In Situ
Ductal Carcinoma in Situ , also known as intraductal carcinoma, accounts for one of every five new breast cancer diagnoses. It’s an uncontrolled growth of cells within the breast ducts. Itâs noninvasive, meaning it hasnât grown into the breast tissue outside of the ducts. The phrase “in situ” means “in its original place.”
DCIS is the earliest stage at which breast cancer can be diagnosed. It’s known as stage 0 breast cancer. The vast majority of women diagnosed with it can be cured.
Even though itâs noninvasive, it can lead to invasive cancer. It’s important that women with the disease get treatment. Research shows that the risk of getting invasive cancer is low if youâve been treated for DCIS. If it isnât treated, 30% to 50% of women with DCIS will get invasive cancer. The invasive cancer usually develops in the same breast and in the same area as where the DCIS happened.
Risk Of Lymph Node Metastasis Is Extremely Low In Micro
So, there is agreement that the risk of lymph node metastasis is very low, but the debate then turns to analyzing the various presenting factors in the microinvasive breast cancer tumor which might positively or negatively influence the incidence rate. Some studies have considered the difference in frequency of axillary node metastasis between tumors with measurable invasion, versus those of microfocal invasion. The rate of axillary lymph node metastasis for microinvasive tumors is estimated at around 4%, and about 8%-9% for measurable tumors. Whether or not the statistical difference is significant is still a matter of interpretation. However, the T1 threshold seems to be significant among physicians, and these larger tumors, even if 90% of the tumor is still DCIS, are thought to be more worrisome.
Don’t Miss: What Does Invasive Breast Cancer Mean
Oncogene Expression May Negatively Affect Breast Cancer Outcome
A relatively new addition to the discussion of breast cancer survival statistics and prognosis is oncogene expression.
An oncogene is a tiny fragment of genetic material which is carried in a chromosome and can cause normal cells to become malignant.
The oncogene HER-2, in particular, has been linked to more aggressive breast cancers.
Around one-third of all breast tumours produce the HER-2 oncogene, and these patients tend to have higher rates of recurrence and lower overall breast cancer survival rates.
According to a 2013 Canadian scientific study, the overall 5-year survival rate of HER-2 positive breast cancer is 88.6%. Furthermore, the relapse-free survival rate for 5 years is 79.4%.
Recommended Reading: What Are Common Treatments For Breast Cancer
Checking For Ductal Breast Cancer In Lymph Nodes
The goal of invasive ductal carcinoma treatment is to get the cancer out of the breast. But we also may need to remove lymph nodes if the cancer has spread there, Wright explains.
Your lymph nodes are part of your immune system. Lymph fluid from the breast drains into the axillary lymph nodes. The number and location of axillary lymph nodes may be different from person to person.
A sentinel lymph node biopsy is a test that can help your doctor determine if removing lymph nodes may be part of your cancer surgery.
The sentinel lymph node is where cancer from invasive ductal carcinoma is likely to show up first. Your doctor can identify the sentinel lymph node by injecting dye into the breast and seeing which node takes up the dye first: This is the sentinel. A sample of tissue from this node can reveal if cancer has spread there.
If theres no cancer in the sentinel node, the other nodes are OK and dont need to be removed, says Wright. If theres a small amount of cancer present, well leave nodes in place and treat the area with radiation or use chemotherapy.
If we see a lot of cancer in the lymph nodes or if four or more lymph nodes are affected, we perform an axillary lymph node dissection: surgery to remove the nodes.
Did you know? Men can get breast cancer, too
About 1 in 100 breast cancers occurs in men. Though men do not have enough lobular tissue to produce milk, they do have milk ducts, and cancer can arise there.
Also Check: Effects Of Breast Cancer On A Person
How Long Does It Take To Recover From Invasive Ductal Carcinoma Treatment
People who undergo surgery for invasive ductal carcinoma usually recover in about two to four weeks. Healing may take longer if lymph nodes are removed or if you choose to undergo breast reconstruction.
Recovery after chemotherapy, radiation therapy, targeted therapy or immunotherapy may take several weeks or several months, depending on the location and stage of the tumor. Your healthcare provider can tell you about how long your treatment should take.
What Is The Prognosis Of Invasive Ductal Carcinoma Of Breast
You May Like: Breast Cancer Stage 1 Grade 3
Invasive Ductal Carcinoma Treatment
Most women with IDC have surgery to remove the cancer. The treatment options are usually:
- Lumpectomy: The surgeon only removes the tumor and a bit of the tissue around it to help make sure all the cancer cells have been removed. You might hear it called breast-conserving surgery
- Mastectomy: The surgeon removes an entire breast.
Which one you get depends on the size of your tumor and how much it has spread throughout your breast and surrounding lymph nodes.
In addition to surgery, other treatments may include:
- Radiation: This usually follows your surgery.
- Hormone therapy: Youâll get it if your cancer is hormone receptor-positive . These drugs block or lower the amount of estrogen in your body.
- Chemotherapy: These medications target cancer cells throughout your body. Doctors may also use It before surgery to shrink tumors and after to kill any cancer cells left behind.
- Targeted therapy: These medications block cancer cell growth. You might get them along with chemotherapy.
You might get one treatment or a combination.
What Is Lobular Carcinoma In Situ
LCIS, like DCIS, is another type of in situ breast cancer. A doctor would detect it through a biopsy.
Researchers are unsure if LCIS is a type of pre-cancer as it rarely transforms into an invasive cancer. However, people with LCIS have a higher risk of developing breast cancer in the future.
Doctors tend to find LCIS after conducting a biopsy for another reason, as it does not usually show up on mammograms and is rarer than DCIS.
Also Check: Ductal Invasive Carcinoma Survival Rate
Don’t Miss: Inflammatory Breast Cancer Age Range
Grading Of Invasive Ductal Carcinoma
In 1957, Bloom and Richardson first developed a histology grading system for invasive ductal carcinoma of the breast, based on the degree of tubule formation, cell nuclear pleomorphism and mitotic count. This system was replaced or modified in 1991 by the Nottingham grading system, which is still based on a points scoring system of the histologic features of the cancer mild, moderate or severe or Grade 1, 2 or 3 .
Recommended Reading: Is Triple Negative Breast Cancer Curable
What Is Breast Cancer
Click to see larger diagrams of the anterior viewimage icon and cross-section viewimage icon of the breast.
Breast cancer is a disease in which cells in the breast grow out of control. There are different kinds of breast cancer. The kind of breast cancer depends on which cells in the breast turn into cancer.
Breast cancer can begin in different parts of the breast. A breast is made up of three main parts: lobules, ducts, and connective tissue. The lobules are the glands that produce milk. The ducts are tubes that carry milk to the nipple. The connective tissue surrounds and holds everything together. Most breast cancers begin in the ducts or lobules.
Breast cancer can spread outside the breast through blood vessels and lymph vessels. When breast cancer spreads to other parts of the body, it is said to have metastasized.
Recommended Reading: How Long Can U Live With Stage 4 Cancer
Myoepithelial Cells As Regulators Of Tissue Polarity
Reversal of inside-out acini by addition of myoepithelial cells. Luminal cells make inside-out acini in collagen. Luminal epithelial cells were double-stained for MUC1 and ESA . In the presence of myoepithelial the acinar polarity is rescued as evidenced by apical expression of MUC1 and ESA . Bar, 25 μm. ).
Improvements In Breast Cancer Screening Mammography Has Lead To Increased Detection Of Microinvasive Dcis
Improvements in the quality and interpretation of breast cancer screening mammograms, as well as a general increase in the number of women participating in breast cancer screening programs, has lead to an increase in findings of ductal carcinoma in situ, with a corresponding increase in Ductal carcinoma in situ with evidence of microinvasion. DCIS is usually diagnosed by mammography, and usually because of the presence of microcalcifications without a detectable mass. If on mammography there appear to be clusters of microcalcifications in several locations, that would be a clue as to a multi-focal presentation of DCIS.
is
Ultrasound rarely diagnoses DCIS on its own. Usually mammography occurs before ultrasound, so if there is a suspicious finding on mammography, ultrasound sometimes helps to clarify the situation.
An ultrasound image of a microinvasive breast cancer lesion will likely appear as an irregularly shaped hypoechoic lesion without shadowing.The ultrasound image of microinvasive ductal carcinoma in situ shown below features faintly detectable calcifications.
Read Also: Stage 3 Cancer
Types Of Invasive Ductal Carcinoma
Most invasive ductal carcinomas are the general type. However, there are four additional sub-types that are much less common:
- Medullary ductal carcinoma – these tumors look aggressive, but are often slow-growing. They are named because they look similar to a part of the brain called the medulla. They are often found in women whose ages are the late 40s to early 50s. The BRCA1 gene raises the risk for this kind of tumor.
- Mucinous ductal carcinoma – this is a less aggressive tumor where cancer cells are surrounded by a puddle of mucin . This cancer most often develops in women in their 60s and beyond.
- Papillary carcinoma – these are very rare kinds of IDC that have a tumor with fingers that grow out and reach toward nearby healthy cells. They most often occur in women after menopause. Sometimes the cells are abnormal and grow very quickly.
- Tubular ductal carcinoma – a less aggressive, slow-growing tumor that grows in very small tube shapes. It is most often found in women in their early 50s.
Age At The Time Of Diagnosis Affects Breast Cancer Survival Rates
It has always been known that curiously, young women have a poorer prognosis than older ones
Indeed, one cohort study examined 4,453 women with breast cancer between 1961 and 1991 who were all treated at the same center.
This study found that both ends of the age spectrum fared less well. So, women under the age of 40 years at diagnosis and those over 80 years had a statistically poorer prognosis.
However, for younger women, this may be due to the fact that they often present with higher-grade tumors that tend to be more aggressive and less likely to be hormone receptor-positive. This means that breast cancer may not respond as well to treatment.
So, it is important to bear in mind other factors discussed in this post, such as stage, grade and hormone receptor status play an important role in prognosis.
You May Like: Malignant Neoplasm Of Breast Treatment