Research Performed Three Decades Ago Enhances Targeted Therapy Today
In 1990, Dr. Mary-Claire King, an assistant professor at UC Berkeley, was the first scientist to demonstrate that a gene on chromosome 17q21, named BRCA1 one year later, was responsible for hereditary early-onset breast cancers. In 1994, Drs. Michael Stratton and Richard Wooster in the UK identified BRCA2. Three decades later, mutations in the BRCA1 and BRCA2 genes become a critical indication to enhance the targeted therapy with Olaparib. It tells us that converting research discoveries to patient-impacting benefits takes pretty long. We need to continue to support basic research today so that new therapies can continue to save patients lives in the future.
To recognize Dr. Mary-Claire Kings fundamental contribution to the genetic understanding of cancer, the National Foundation for Cancer Research awarded Dr. Mary-Claire King the Szent-Györgyi Prize for Progress in Cancer Research in 2016 in Washington DC. Learn more about this award and Dr. Mary-Claire Kings research here.
Olaparib offers survival benefits and brings new hopes to patients with early triple-negative breast cancer. As the patients have to be selected by an FDA-approved blood test before the treatment, patients should work with their doctors to determine whether they are eligible for the treatment before receiving the treatment.
Sign up here to receive our monthly e-newsletter featuring healthy living information, stories of inspiration, support resources, cancer prevention tips, and more.
References:
Here’s What Study Shows
In a new study, researchers from Boston University Chobanian & Avedisian School of Medicine demonstrated that proper control of a cellular pathway known as the Hippo pathway prevents the development of triple-negative breast cancer.
These findings appear online in the journal Nature Communications.
“We found that when this pathway is dysregulated or impaired, luminal epithelial cells in the mammary gland rapidly transition to a basal-like state and develop into triple negative carcinomas,” explained corresponding author Bob Varelas, PhD, associate professor of biochemistry.
In an experimental model, the researchers conditionally deleted the Lats1 and Lats2 genes, two components of the Hippo pathway, in the luminal epithelium of the mammary glands. When these genes were deleted, the models rapidly develop basal-like mammary carcinomas resembling human basal-like breast cancers. They found that the development of these carcinomas depended on the activity of the Hippo pathway effector proteins YAP and TAZ, and that deletion of these two proteins reversed carcinoma development in their model.
What Are Symptoms Of Triple Negative Breast Cancer
TNBC symptoms are the same as other common breast cancers. And many breast cancer symptoms are similar to other less serious conditions. That means having certain symptom doesnt mean you have breast cancer. Possible breast cancer symptoms include:
- A new lump or mass.
- Swelling in all or part of a breast.
- Nipple retraction, when your nipple turns inward.
- Nipple or breast skin thats dry, flaking, thickened or red.
- Nipple discharge that is not breast milk.
- Swollen lymph nodes. This symptom happens when breast cancer spreads to the lymph nodes under your arm or near your collarbone.
Also Check: Radiation Machine For Breast Cancer
Repurposing An Experimental Treatment
Seviteronel was originally developed as a standalone therapy for breast and prostate cancers that carry the androgen receptor and was proven safe for patients in Phase II clinical trials.
Our research has revealed that seviteronel may be far more beneficial as an adjunct therapy. We found that androgen inhibition blocks cancer cell state switching, locking cancer cells in a chemotherapy-sensitive state. This is why chemotherapy plus seviteronel treatment was more effective than chemotherapy alone at targeting cancer in our preclinical studies, says Dr Perez San Juan.
We hope that this new combination treatment approach will drastically reduce drug resistance to improve the effectiveness of standard-of-care chemotherapy and, ultimately, improve outcomes for patients.
For further information about the 4CAST clinical trial or to register your interest for the trial, please contact St Vincents Hospital Sydney Research Office,
–ENDS
The clinical trial is sponsored by St Vincents Hospital Sydney and supported by Kembi Therapeutics Pty Ltd. The trial was made possible by research supported by The NELUNE Foundation, The Paramor Family, Australias National Health & Medical Research Council, Cancer Institute NSW, the National Breast Cancer Foundation, the Girgensohn Foundation and the St Vincents Hospital Research Foundation.
The research has ethics approval from St Vincents Hospital Human Research Ethics Committee .
Signs And Symptoms To Know
The signs and symptoms of triple-negative breast cancer are the same as with all breast cancers. It may present as a lump, which is more commonly hard, painless and irregular, but can also be soft, round and painful. Other signs include:
- Breast swelling
- A nipple that turns inward
- Skin changes on the breast or nipple, including redness, dryness, thickening or flaking
Read Also: Survival Rate Inflammatory Breast Cancer
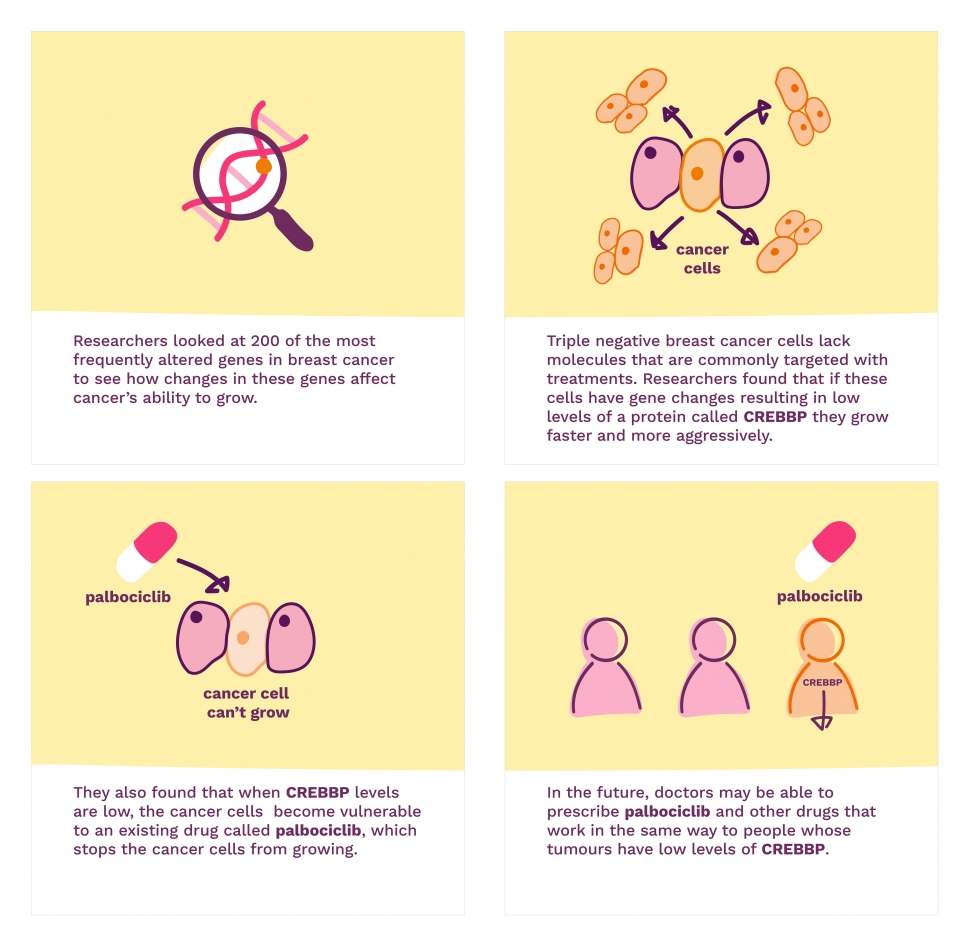
Sights Set On First Targeted Therapy For Triple
A new study is seeking new drugs to combat triple-negative breastcancer, an aggressive form of the disease that doesnt rely on thehormones estrogen and progesterone or the protein HER2, which fuel thegrowth of most breast cancers.
The projects goal? Find new drugs to combat the cancer, which doesnt rely on the hormones estrogen and progesterone or the protein HER2, which fuel the growth of most breast cancers.
Given this, the drugs that treat most breast cancers by blocking their ability to use those three things to survive dont work on triple-negative breast cancer, says Stacy Moulder, M.D., associate professor of Breast Medical Oncology and the trials principal investigator.
Instead, doctors are left to treat triple-negative patients with traditional chemotherapy drugs, surgery and radiation.
Typically, patients with a triple-negative breast tumor thats larger than one centimeter and hasnt spread to other parts of the body are given chemo before surgery. In nearly half of these patients, chemo works well. It kills all or nearly all of the cancer cells, and little to no cancer in the breast or lymph nodes is present at the time of surgery.
This is associated with an extremely good prognosis, Moulder says.
But the other half of patients who do not respond well to chemo face a high probability their cancer will come back within three years after treatment. When the disease returns, prognosis is poor.
You May Like: Milk Duct Cancer Symptoms
Brca1 Inherited Gene Mutations And Tnbc
Most breast cancers related to a BRCA1 inherited gene mutation are both triple negative and basal-like .
TNBC may also be related to a BRCA2 inherited gene mutation .
The National Comprehensive Cancer Network recommends people diagnosed with TNBC at age 60 or younger get genetic testing .
Learn more about genetic testing.
Don’t Miss: How Common Is Her2 Positive Breast Cancer
Molecular Subtypes And Characteristics Of Triple
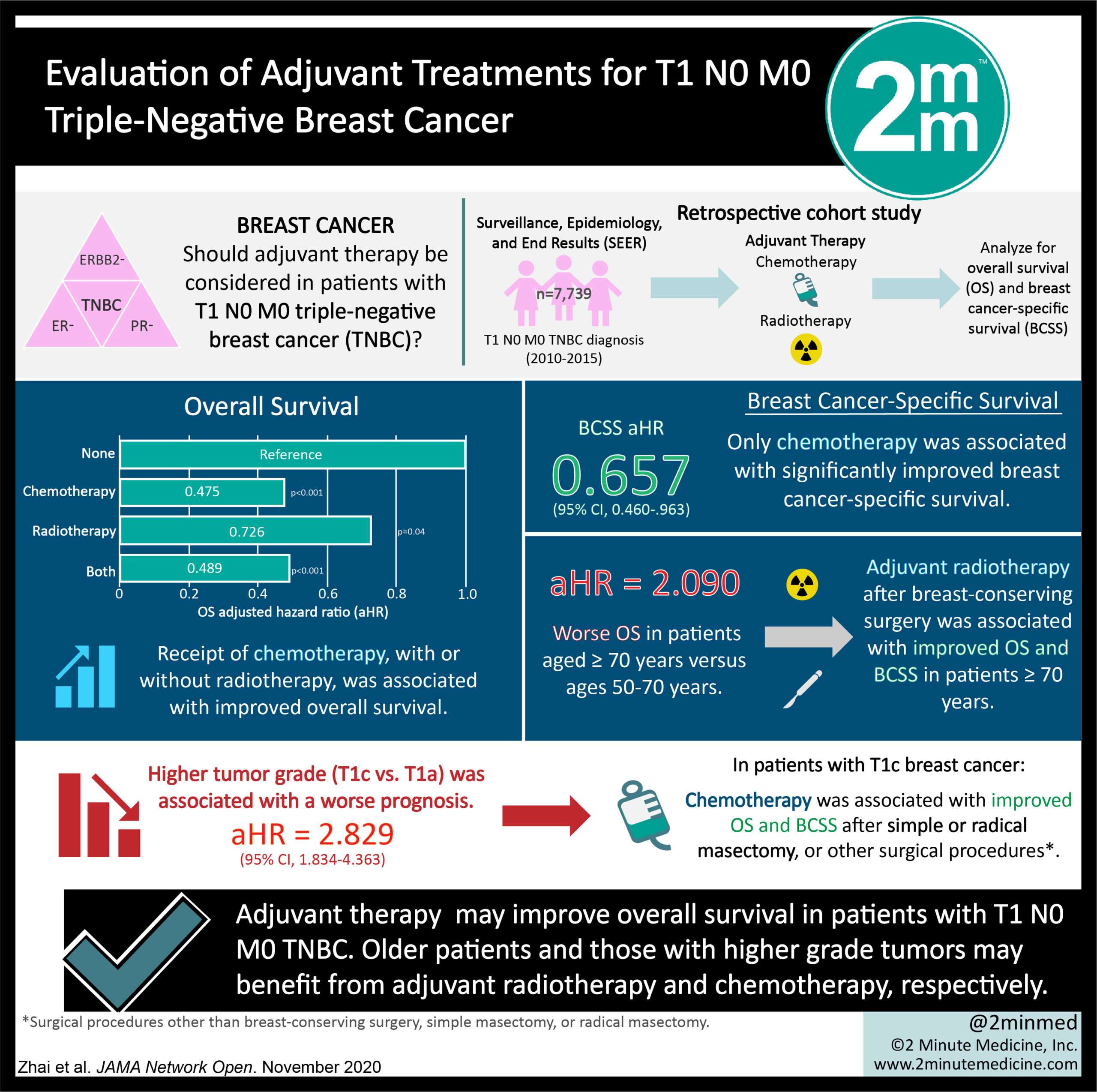
To avoid blindly developing therapeutic strategies, identifying the complex TNBC subtypes and molecular hallmarks is necessary given that these features are closely linked with clinical outcomes, for example, response to chemotherapy, the pattern of recurrence, and prognosis. Different approaches, including somatic DNA mutation, copy number aberrations, gene expression profiling, and immune metagene information, were applied to analyze TNBCs as a highly diverse group of cancers.
Additionally, molecular alterations were assessed to explore various potential targets for TNBC treatment. It is worth mentioning that a deficiency in homologous recombination, which is partly associated with the loss of breast cancer susceptibility gene function in BC, is correlated with a good response to cisplatin treatment . In an early phase II clinical trial, patients with BRCA-mutant TNBC showed an overall response rate of 80% with single cisplatin therapy . A deficiency in homologous recombination means failure to repair DNA double-strand breaks and damaged DNA replication forks. Therefore, these individuals are also sensitive to poly-adenosine diphosphate -ribose polymerase inhibitors , as PARP is the enzyme that responds to repair DNA single-strand breaks and maintain genome stability.
Fig. 1
Excelerate Your Healing Journey By Joining Our Free Breast Health Educational Program All Happening This Month Hosted By Experts From Around The Globe And As A Limited
About 15% of all breast cancer cases are Triple Negative. It is considered the most aggressive and treatment-resistant, cancer often recurring soonest if treatment fails. Since traditional chemo treatments focus on and target hormone-positive cancers, they dont have much to offer in terms of TNBC. TNBC cells dont have receptors for estrogen, progesterone, and Her2/neu, so they have nothing to grab onto. Additionally, since it is a less-targeted treatment, it is even more toxic to the body. But this doesnt mean it is all gloom and doom.
You May Like: Thyroid Cancer And Breast Cancer
Clinical Trial To Test Potential New Combination Therapy For Aggressive Breast Cancer
Associate Professor Christine Chaffer
Media Release: 21 June 2022
NSW researchers are calling for volunteers for a new clinical trial to test a new strategy in cancer treatment: using a new therapy to target a defence switch on cancer cells that alerts cancer to the threat of chemotherapy.
The trial aims to improve survival rates for patients with triple negative breast cancer, a treatment-resistant form of cancer that can quickly adapt against chemotherapy.
It will be led by Associate Professor Christine Chaffer and Dr Beatriz San Juan from the Garvan Institute of Medical Research, and Senior Staff Specialist in medical oncology Dr Rachel Dear of St Vincents Hospital Sydney. The trial will be conducted at The Kinghorn Cancer Centre in Darlinghurst.
The research leading to the trial has been supported by the NELUNE Foundation, which awarded Associate Professor Chaffer with the Rebecca Wilson Fellowship in Cancer Research in 2017 enabling her to bring her research back to Sydney from the USA. The Fellowship is a lasting legacy to sports journalist the late Rebecca Wilson.
Triple negative breast cancer is an aggressive disease with a greater likelihood of spreading around the body and recurring within five years than other breast cancers.
In preclinical studies, we found that an experimental drug, seviteronel, combined with chemotherapy, could be twice as effective in reducing the size of tumours than chemotherapy alone, says Associate Professor Chaffer.
Breakaway Breast Cancer Cells Can Travel To The Brain: Scientists Plot Path In Quest To Block Entry
Science Translational Medicine
One of the most puzzlingand devastatingaspects of cancer is its potentially lethal wanderlust, the spread of the disease from a primary tumor to a new and distant site.
The process, of course, is formally called metastasis, which at its most basic is recognized as cancer cells on-the-move. Having broken away from a primary tumor these malignant migrants hitch a ride aboard the blood or lymphatic systems to seed new tumors. As countless studies have shown, certain forms of cancer have preferential destinies.
Scientists at Université de Fribourg in Switzerland are studying the development of brain metastases in patients with breast cancer. Knowing how these cancer cells make their way to the brain helps lay the groundwork for interventions that block tumor cells’ well-beaten path. Blocking the cells from a target tissue is vital because metastatic cancer is inevitably worse in terms of its aggression and harder to fight than a primary tumor, oncologists say.
“Brain metastasis is a complication of increasing incidence in patients with breast cancer at advanced disease stage,” writes Dr. Girieca Lorusso whose laboratory focuses on experimental and translational oncology. “It is a severe condition characterized by a rapid decline in quality of life and poor prognosis. There is a critical clinical need to develop effective therapies to prevent and treat brain metastases,” Lorusso added.
More information:Science Translational Medicine
Recommended Reading: How Big Are Breast Cancer Tumors
Combination Therapies In Tnbc
From the results of current TNBC clinical trials, the benefit of a single conventional anticancer therapy or immunotherapy is not sufficient due to tumor heterogeneity, tumor evolution and drug resistance. Therefore, combination therapy is currently the preferred option for TNBC treatment, and we summarize the primary endpoints of clinical trials in Table and the current drug combination trials for TNBC in Fig. . From these studies, patients with nonadvanced TNBC had good responses after combination therapy however, the prognosis of advanced TNBC still remained poor. Among them, PD-L1+ patients treated with conventional chemotherapy combined with immunotherapy as first-line therapy had a good prognosis , as described in the Sect. . In addition, those patients with BRCA-associated mutations have achieved a better prognosis after combination targeted therapy . In second-line treatment, the novel ADC drug sacituzumab govitecan has been demonstrated undeniable effects , and the combination therapy of ADC is worth exploring and looking forward to. Undoubtedly, precise personalized treatment of TNBC relies on the study of molecular expression characteristics and tumor biological mechanisms. Therefore, routine immunomolecular expression assessment and mutation analysis of TNBC tumor tissues are recommended, which will provide solid evidence for determining TNBC combination therapy regimens.
Table 7 Clinical trials evaluating adoptive cell therapy in patients with TNBC
What To Drink And Eat
Matcha Tea: Every morning is just better when it starts with tea, or really any time of day for that matter! Once you know that this type of tea contains epigallocatechin-3-gallate , which can kill cancer cells by limiting angiogenesis, prevent DNA damage, and may stop the production of breast cancer stem cellsit is even more of a treat! Matcha tea provides up to 137 times more EGCG than regular green tea! So drink upI suggest 2 cups a day of this type of Matcha Tea. It is also packed with antioxidants, vitamin C, tocopherols, carotenoids, selenium, zinc, chromium, and manganese. Matcha also detoxifies heavy metals and toxic chemicals while burning fat and boosting your metabolism.
Drinking tea is also a great life metaphor. We are like teawe dont know our strength until we are in hot water -says many revolutionary women. Right now, you are realizing just how strong you are and then finding even more power, my dear conqueror. Buy Matcha Tea.
Blueberries: A berry delicious way to increase the number of cancer destroying Natural Killer cells in the body and slow or stop the growth of Breast Cancer Stem Cells is to enjoy a handful of organic blueberries every day. This study found that these berries can cause apoptosis in TNBC cells! You can also order a blueberry concentrate from Life Extension if you are trying to keep your sugars down. Here is my full report on these little superheroes, and I highly suggest this delectable Blueberry Chia Pudding!
You May Like: What Percentage Of Men Get Breast Cancer
Treatment Options In The Earlier Stages
Early-stage breast cancer is generally considered to be stages 0 through 3, Bora Lim, M.D., assistant professor in the Breast Medical Oncology department at the University of Texas MD Anderson Cancer Center, tells SELF.
Because there are no approved targeted therapies available in the earlier stages of triple negative breast cancer, the standard of care is chemotherapy, according to the NCI. This is a systemic therapy, meaning it affects cells throughout your body, says Dr. Nanda, who specializes in the treatment of triple negative breast cancer along with early-onset, hereditary, and locally advanced breast cancers. It involves taking drugs orally, via injection, through infusion, or even topically. These drugs then travel throughout the bloodstream and destroy or halt the division of cancer cells. The chemo that we use is the same regimen as for any type of breast cancer, Dr. Nanda says.
Typically, you will receive chemo in combination with surgery . Sometimes chemo comes after surgery, but your doctor might suggest doing it before, Wendy Y. Chen, M.D., M.P.H., breast oncologist at the Dana-Farber Cancer Institute and assistant professor of medicine, at Harvard Medical School, tells SELF. This helps shrink the tumor as much as possible before removing it, which has an added benefit: The more knowledge about the treatment responsiveness of the tumor that someone has, the more we know about their prognosis, Dr. Chen explains.
Combinations Of Immune Checkpoint Inhibitors
However, most patients with TNBC do not respond well to PD-1 or PD-L1 monotherapy therefore, inducing a favorable tumor immune microenvironment appears to be particularly important. Conventional chemotherapeutic agents, such as taxane, cisplatin, and cyclophosphamide, can enhance tumor antigen release, improve the tumor microenvironment, and add the possibility of an antitumor response . Biopsies before and after NAC showed that the immune microenvironment was altered from low TIL to high TIL, and patients with high TIL levels exhibited improved survival . For example, paclitaxel has pleiotropic immune-modulating effects because it helps mature dendritic cells shift the T-helper phenotype to promote the secretion of proinflammatory cytokines and enhance the activity of CD8+ T cells . An animal model has shown evidence that cisplatin markedly induces tumor regression and improves survival when combined with anti-PD-1 and anti-cytotoxic lymphocyte antigen 4 . These studies suggest that ICB combined with chemotherapy may achieve a synergistic or additive clinical effect.
In addition to the combination of PARPi and immunotherapy, a series of trials of immunotherapy in combination with other drugs have entered clinical studies . For example, alternative PD-1/PD-L1 ICB combined with tyrosinase inhibitors has entered phase III studies .
Table 4 Unpublished phase III trials of immunotherapy for TNBC
Recommended Reading: What Are Five Methods For Detecting Breast Cancer
Study Finds Nanomedicine Targeting Lymph Nodes Key To Triple Negative Breast Cancer Treatment
In mice, nanomedicine can remodel the immune microenvironment in lymph node and tumor tissue for long-term remission and lung tumor elimination in this form of metastasized breast cancer.
Research from the University of Michigan Rogel Cancer Center could provide a new approach to treating an aggressive form of breast cancer.
A study led by Duxin Sun, Ph.D., found that targeting the immune microenvironment in lymph nodes and tumors simultaneously led to long-term tumor remission in mice models of metastatic triple negative breast cancer. Further, using nanoparticles to deliver these immune-altering drugs increases treatment efficacy. These results appear in Science Translational Medicine.
Immunotherapy combined with chemotherapy has been long approved as standard treatment option for triple negative breast cancer but only shows a limited response in patients. Many believe that the tumor immunosuppressive microenvironment is one of the main contributing factors for the poor responses in those with TNBC.
Sun,Charles R. Walgreen Jr. Professor of Pharmacy and Professor of Pharmaceutical Sciences at the U-M College of Pharmacy, says that previously developed immunomodulators work well in animal models, but fail in clinical trials. He and his team wanted to come up with a better approach that would treat TNBC patients long-term that could withstand the rigor of clinical trials. To do this, they had to look beyond just the tumor microenvironment to the lymph nodes.