Get To And Stay At A Healthy Weight
Being overweight or obese can increase your risk for many types of cancer. You can control your weight with the choices you make about healthy eating and exercise:- Avoiding excessive weight gain throughout life- Balance the calories you take in with the amount of physical activity you do
If you are overweight, try to get to a healthy weight and stay there. Losing even a small amount of weight has health benefits and is a good place to start. Watching your portion sizes is an important part of weight control especially for foods high in fat and sugar. Low-fat and fat-free doesnt always mean low-calorie, so read labels and try to eat vegetables, fruits, and whole grains in the place of higher-calorie foods.
All women are at risk from Breast Cancer, which affects one in eight women in the world today. Many risk factors are things that you have no or little control over, such as your family history or your race.
It is important to remember that three-quarters of women who get Breast Cancer were not at increased risk, and we dont fully understand why different women get cancer yet. Even if you have all these risk factors, it only highlights the need to be careful and check your breasts regularly. It does not mean you are going to get Breast Cancer.
So what are the risk factors for Breast Cancer and how can you deal with them? You can separate risk factors into three groups:
Breast Cancer Screening Saves Lives
Screening tests can find breast cancer early, when the chances of survival are highest. Getting screened regularly means your doctor is likely to know sooner if theres a problem, so you can get effective treatment as early as possible. There are more than 3.5 million breast cancer survivors in the U.S. todaymore than any other group of cancer survivorslargely thanks to advances in screening and treatment.
You May Like: What Is Stage 3b Cancer
Risks Of Mammography For Women Ages 40
Over-diagnosis and over-treatment are risks of mammography. Over-diagnosis and over-treatment occur when a mammogram finds a cancer that never would have caused symptoms or problems if it had never been diagnosed and had been left untreated.
Another drawback of mammography in women ages 40-49 is a high rate of false positive results .
Younger women are more likely than older women to have a false positive result on a mammogram. This is due to a number of reasons including the low number of breast cancers that occur in younger women and higher breast density in younger women.
Getting a false positive result means these women will be told they have an abnormal finding and undergo follow-up tests, only to find they dont have breast cancer. Follow-up tests may include a follow-up mammogram , breast ultrasound or even a biopsy.
Don’t Miss: Stage 2 3 Breast Cancer
Effectiveness Of Early Detection And Treatment
Primary Screening With Conventional Mammography
An updated meta-analysis by Nelson and colleagues of RCTs of screening mammography found similar RR reductions in breast cancer mortality by age group as the previous USPSTF evidence review. The combined RRs were 0.92 for women aged 39 to 49 years, 0.86 for women aged 50 to 59 years, 0.67 for women aged 60 to 69 years, and 0.80 for women aged 70 to 74 years.2, 3
None of the trials nor the combined meta-analysis demonstrated a difference in all-cause mortality with screening mammography.2
Observational studies of screening mammography reported a wide range of breast cancer mortality reduction rates. Recent meta-analyses from the EUROSCREEN Working Group showed an approximate 25% to 31% relative reduction in breast cancer deaths in women aged 50 to 69 years who were invited to screening. In comparison, meta-analysis of RCTs that used an intention-to-treat analysis found a 19% to 22% breast cancer mortality reduction in women in the same age range.2, 3
Primary Screening With DBT
No studies evaluated the effect of screening for breast cancer with DBT on important health outcomes, such as mortality, treatment-related morbidity, or quality of life.13
Adjunctive Screening in Women With Dense Breasts
No studies evaluated the effects of adjunctive screening with any method in women with dense breasts on breast cancer rates, quality of life, or mortality.17, 18
Place Your Hands On Your Hip
Strip to the waist and stand before a mirror. You will need to see both breasts at the same time. Stand with your hands on your hips and check the overall appearance of your breasts.
Look at the size, shape, and contour.
Note changes, if any, in the color or texture of the skin on your breasts as well as on your nipples and areolas.
Recommended Reading: Did Anne Hathaway Have Breast Cancer
Why Do Some Women Get A Letter About Breast Cancer Screening
Breast cancer screening is so important that Cancer Care Ontario, an agency of the Ontario Ministry of Health and Long-Term Care, sends letters to eligible women to invite them to have a mammogram. Women also get letters that tell them their screening results and remind them when it is time to return for screening. It is your choice to be screened or not.
Women At Higher Risk Of Breast Cancer
Factors that greatly increase breast cancer risk include :
- A personal history of invasive breast cancer or ductal carcinoma in situ
- A personal history of lobular carcinoma in situ or atypical hyperplasia
- Radiation treatment to the chest area between ages 10-30
- Li-Fraumeni, Cowden/PTEN or Bannayan-Riley-Ruvalcaba syndrome
- An ATM, BARD1, BRIP1, CDH1, CHEK2, NBN, NF1, PALB2, PTEN, RAD51C, RAD51D, STK11 or TP53 inherited gene mutation
- A greater than 20 percent lifetime risk of invasive breast cancer based mainly on family history
Figure 3.5 below outlines the National Comprehensive Cancer Network breast cancer screening guidelines for women at higher than average risk up to age 75.
The NCCN recommends women older than 75 talk with their health care providers about a breast cancer screening plan thats right for them.
Figure 3.6 below outlines the American Cancer Society breast cancer screening guidelines for women at higher than average risk .
|
Figure 3.5: NCCN breast cancer screening recommendations for women at higher than average risk |
|
Risk factor |
Recommended Reading: Can Stage 3 Breast Cancer Be Cured
Read Also: Stage 2 Breast Cancer Metastasis
Cancer Screening Guidelines By Age
The choices you make about diet, exercise, and other habits can affect your overall health as well as your risk for developing cancer and other serious diseases.
Its also important to follow recommendations for cancer screening tests. Screening tests are used to find cancer in people who have no symptoms. Regular screening gives you the best chance of finding cancer early when its small and before it has spread.
Health care facilities are providing cancer screening during the COVID-19 pandemic with many safety precautions in place. Learn how you can talk to your doctor and what steps you can take to plan, schedule, and get your regular cancer screenings in Cancer Screening During the COVID-19 Pandemic.
The tabs below provide information on healthy lifestyle choices that can help lower your cancer risk, and cancer screening test recommendations by age.
Donât Miss: Malignant Neoplasm Of Female Breast
British Columbia Specific Information
Breast cancer is the most common type of cancer in women in British Columbia. Breast cancer can occur in men as well, but it is not as common. Tests and treatments for breast cancer vary from person to person, and are based on individual circumstances. Certain factors such as your age, family history, or a previous breast cancer diagnosis may increase your risk of developing breast cancer. For information about your specific risk factors, speak with your health care provider.
A number of screening methods, including mammograms in women, can help find and diagnose breast cancer. The decision to have a mammogram or use any other screening method may be a difficult decision for some women. While screening for breast cancer is often recommended, it is not mandatory. Speak with your health care provider for information regarding how to get screened, the facts and myths about screening tests, how to maintain your breast health, and to get help making an informed decision.
For more information about breast cancer and breast cancer screening, visit:
If you have questions about breast cancer or medications, speak with your health care provider or call 8-1-1 to speak with a registered nurse or pharmacist. Our nurses are available anytime, every day of the year, and our pharmacists are available every night from 5:00 p.m. to 9:00 a.m.
Don’t Miss: Healing Cancer With Baking Soda
Where To Get Screened
Women ages 50 to 74 can call the nearest Ontario Breast Screening Program location to make an appointment .
Women in the North West and Hamilton Niagara Haldimand Brant regions may be eligible for screening in one of our mobile screening coaches.
If you think you may be at high risk for breast cancer, talk to your doctor about a referral to the High Risk Ontario Breast Screening Program based on family or medical history.
What This Means For You
- high-quality mammography
- family history of breast or other related cancers
- any test results for gene mutations linked to a high risk of breast cancer
- results of past breast biopsies, even if they were benign
- personal history of being treated with radiation to the face and/or chest before age 30
- breast density
- whether or not you had a full-term pregnancy or breastfed
Written by: Jamie DePolo, senior editor
Read Also: Breast Cancer Secondary Cancer
No : Unusual Swelling
If there is no reason for your breasts to swell such as the hormonal changes that occur when getting your period or during pregnancy, an infection from breastfeeding, or an injury a change in the size or shape of your breasts could be a sign of breast cancer. Also, be aware of swelling in your armpit or near your collarbone, which could indicate breast cancer that has spread to the lymph nodes. Even if there isnt a lump you can feel, and even though other conditions may cause breast swelling as well, this is still a change worth telling your doctor about.
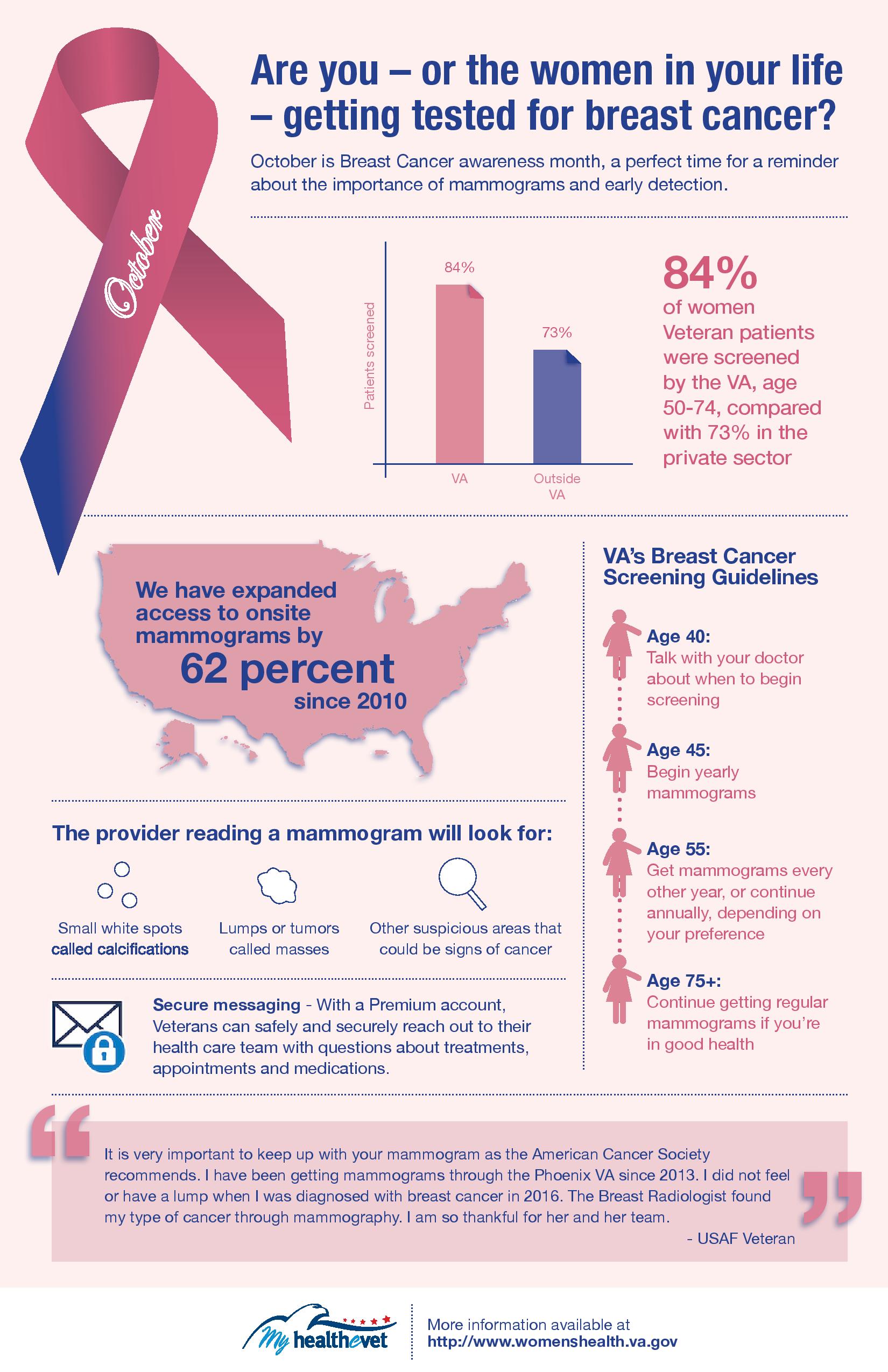
Breast Cancer Screening: Understanding The Guidelines
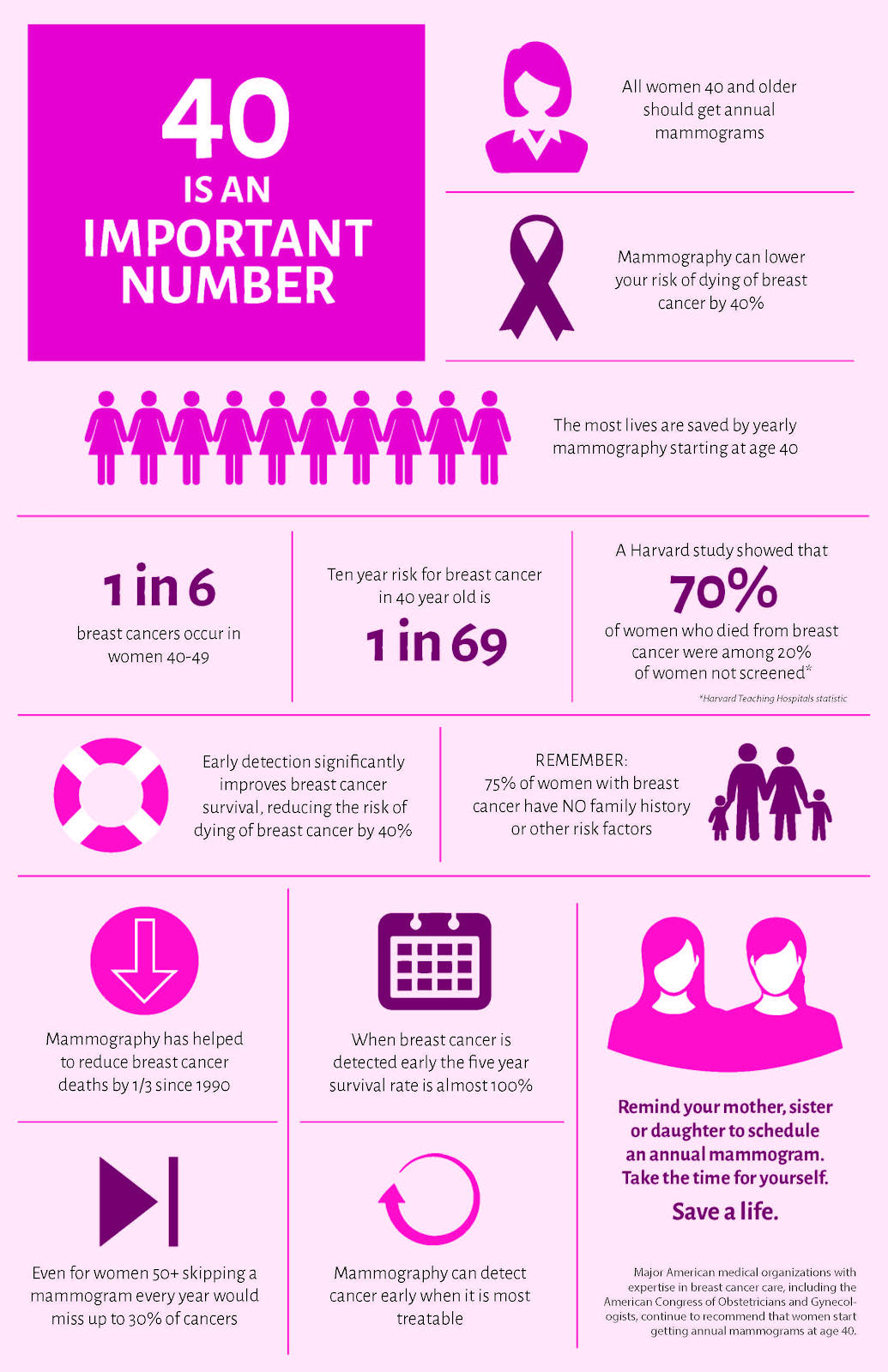
Approximately one in eight women will develop invasive breast cancer during her lifetime, according to the American Cancer Society . This post is designed to outline breast cancer screening guidelines.
Mammography is a very important screening tool for early breast cancer detection, but there are several different guidelines for when to start and how often to undergo mammography, says Dr. Giess. This can be confusing for many women.
The American College of Radiology recommends annual screening mammography beginning at age 40. The ACS guidelines emphasize screening based on a womans individual risk of developing breast cancer and her personal preferences.
Recommended Reading: Stage Iii A Cancer
When To Start Screening
Clinical trials, observational studies, and modeling studies all demonstrate that the likelihood of avoiding a breast cancer death with regular screening mammography increases with age, and this increase in benefit likely occurs gradually rather than abruptly at any particular age. In contrast, the harms of screening mammography either remain constant or decrease with age. For example, about the same number of breast biopsies are performed as a result of screening mammography in women aged 40 to 49 years as in those aged 60 to 69 years, but many more of these biopsies will result in a diagnosis of invasive cancer in the older age group. Thus, the balance of benefit and harms improves with age .
It is, however, a false dichotomy to assume that the only options are to begin screening at age 40 or to wait until age 50 years. As women advance through their 40s, the incidence of breast cancer rises. The balance of benefit and harms may also shift accordingly over this decade, such that women in the latter half of the decade likely have a more favorable balance than women in the first half. Indeed, the CISNET models suggest that most of the benefit of screening women aged 40 to 49 years would be realized by starting screening at age 45.7, 8
Where Can I Go To Get Screened
You can get screened for breast cancer at a clinic, hospital, or doctors office. If you want to be screened for breast cancer, call your doctors office. They can help you schedule an appointment.
Most health insurance plans are required to cover screening mammograms every one to two years for women beginning at age 40 with no out-of-pocket cost .
Are you worried about the cost? CDC offers free or low-cost mammograms. Find out if you qualify.
You May Like: Estrogen Dependent Breast Cancer
High Risk Screening Program
We offer a screening and prevention program for women at high risk of developing breast cancer. Our team of medical oncologists, surgical oncologists, and staff members works with you to help you gain a clear understanding of your breast cancer risk factors, how your risk of developing the condition evolves as your life changes, and what you can do to manage your risk.
Our screening and prevention program is tailored to healthy women who are at high risk of developing breast cancer.
Through this program, each woman receives a thorough physical examination, a review of her medical history by an oncologist, and routine and advanced screening examinations that may consist of clinical breast exams, mammograms, ultrasounds, and MRIs.
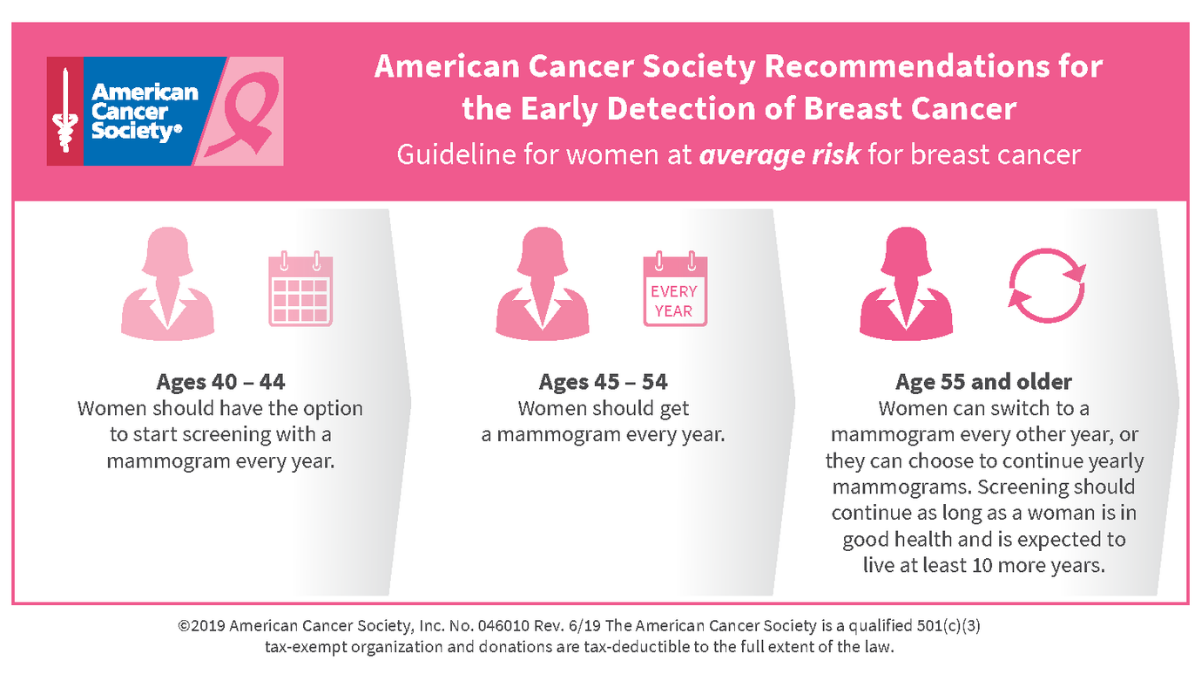
For Women At Average Risk
According to the American Cancer Society , youre at average risk if you meet the following criteria:
- No personal history of breast cancer
- No immediate family history of breast cancer
- No genetic mutations that increase the risk of breast cancer, like a BRCA gene mutation
- No past radiation therapy in the chest area before age 30
Women who meet these criteria are then split into age groups.The guidelines of the American College of Radiology and the American College of Surgeon’s National Accreditation Program for Breast Centers state that:
- Women at average risk start getting annual mammograms at the age of 40.
- Women at average risk between the ages of 55 and 74 should get mammograms every one to two years.
- Women at average risk who are over 75 should continue to get mammograms depending on their overall health, including a life expectancy of 10 or more years.
Recommended Reading: 3b Breast Cancer
Why Choose A Provider At Intermountain Healthcare
Intermountain Healthcare is focused on care in your community. Our network of specialists includes OB-GYNs and other experts on womens health. We are dedicated to listening to you and your needs. Use our find a provider tool today to schedule an appointment to learn more about breast cancer screening.
*This article is for informational purposes only and is not intended to be a substitute for medical advice or diagnosis from a physician or qualified healthcare professional.
Benefit And Harms Of Screening And Early Treatment
The USPSTF found adequate evidence that mammography screening reduces breast cancer mortality in women aged 40 to 74 years. The number of breast cancer deaths averted increases with age women aged 40 to 49 years benefit the least and women aged 60 to 69 years benefit the most. Age is the most important risk factor for breast cancer, and the increased benefit observed with age is at least partly due to the increase in risk. Women aged 40 to 49 years who have a first-degree relative with breast cancer have a risk for breast cancer similar to that of women aged 50 to 59 years without a family history. Direct evidence about the benefits of screening mammography in women aged 75 years or older is lacking.
The USPSTF found adequate evidence that screening for breast cancer with mammography results in harms for women aged 40 to 74 years. The most important harm is the diagnosis and treatment of noninvasive and invasive breast cancer that would otherwise not have become a threat to a womans health, or even apparent, during her lifetime . False-positive results are common and lead to unnecessary and sometimes invasive follow-up testing, with the potential for psychological harms . False-negative results also occur and may provide false reassurance. Radiation-induced breast cancer and resulting death can also occur, although the number of both of these events is predicted to be low.
Read Also: Breast Cancer Nodes
Vpfw Now Offers Mammograms At Our St Francis Location
VPFWs St. Francis office is excited to have opened a new mammography suite this winter. St. Francis joins our Midlothian Turnpike, West Creek, and Prince George locations in offering mammograms that are read by our colleagues with Radiology Associates of Richmond.
With mammography on site, planning for your annual exam and mammogram together could not be easier! Our phone staff is ready to answer questions about scheduling, especially regarding the COVID-19 vaccine. We are also happy to discuss specific risk-related questions. Learn more on our mammography page.
To schedule a mammogram at a VPFW office near you, you can call us at or set an appointment online.
About the Author
American College Of Physicians Guidelines
A 2019 guidance statement from the American College of Physicians , based on a review of existing guidelines, addresses mammography in women at average risk, which is defined as the absence of the following:
- History of breast cancer or previous diagnosis of a high-risk lesion
- Genetic mutations such as BRCA1/2 or another familial breast cancer syndrome
- History of radiation therapy to the chest in childhood
The ACP provides the following recommendations to clinicians for breast cancer screening in average-risk women, according to age :
- Ages 40 to 49 years: Discuss whether to screen for breast cancer with mammography before age 50 years. The discussion should include the potential benefits and harms and the womanâs preferences. For most women in this age group, the potential harms outweigh the benefits.
- Ages 50 to 74 years: Offer screening for breast cancer with biennial mammography.
- Ages 75 years or older or in women with a life expectancy of 10 years or less: Discontinue screening for breast cancer.
- All ages: Do not use clinical breast examination to screen for breast cancer.
Recommended Reading: Did Anne Hathaway Have Breast Cancer
Recommended Reading: Stage 1 Breast Cancer Survival Rate