Deficiency Of Brca1 Expression Is Likely Tumorigenic
DNA damage appears to be the primary underlying cause of cancer, and deficiencies in DNA repair appears to underlie many forms of cancer. If DNA repair is deficient, DNA damage tends to accumulate. Such excess DNA damage may increase mutational errors during DNA replication due to error-prone translesion synthesis. Excess DNA damage may also increase epigenetic alterations due to errors during DNA repair. Such mutations and epigenetic alterations may give rise to cancer. The frequent microRNA-induced deficiency of BRCA1 in breast and ovarian cancers likely contribute to the progression of those cancers.
Does Health Insurance Cover The Cost Of Genetic Testing For Brca1 And Brca2 Variants
People considering BRCA1 and BRCA2 variant testing may want to confirm their insurance coverage for genetic counseling and testing. Genetic counselors can often help answer questions about insurance coverage for genetic testing.
Some genetic testing companies may offer testing for inherited BRCA1 and BRCA2 variants at no charge to patients who lack insurance and meet specific financial and medical criteria.
What Happens If My Test Is Positive For Hereditary Breast Cancer Risk
If testing confirms you are at risk, your care provider can work with you on a plan to safeguard your health, which could include:
- High-risk evaluation and monitoring
- Screening schedules, including digital mammography and clinical breast exams
- Hormonal therapy medications designed to prevent the development of breast cancer
Preventive surgery, such as mastectomy with breast reconstruction, is necessary only for patients at very high risk for aggressive breast cancer.
A comprehensive breast center offers a safe and supportive environment where you can ask questions and get the best answers for you, Ninan says. Every patients decision about how to handle their risk of developing breast cancer is managed with sensitivity and an understanding about the complexity of these decisions.
Don’t Miss: Lymph Nodes Cancer Stage 3
How Is Hboc Identified
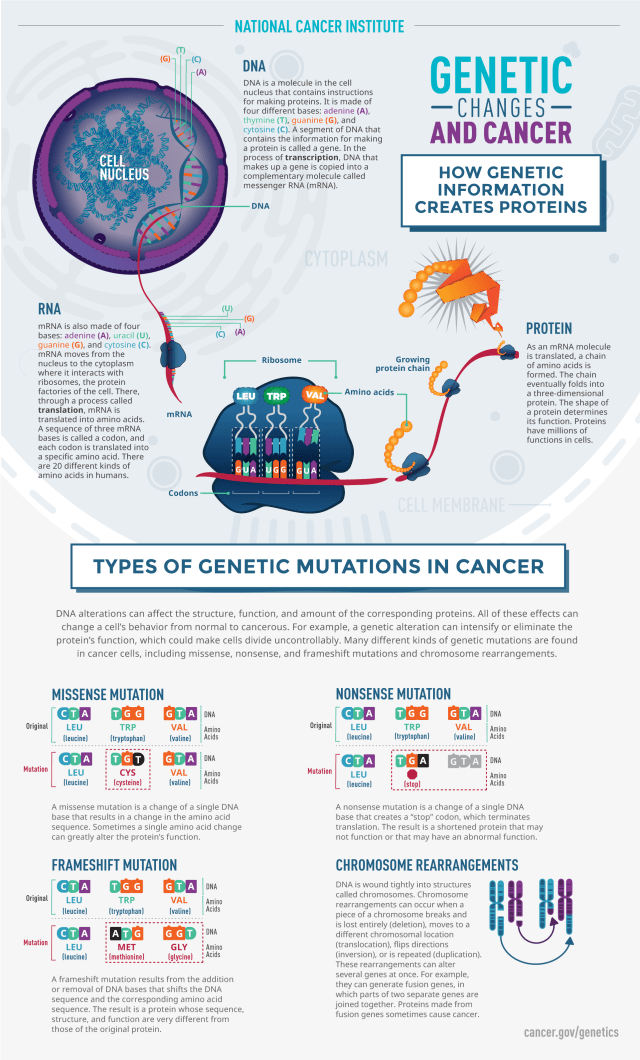
Mutations in the BRCA1 or BRCA2 genes can be identified through a blood or saliva test. The usual method of testing, called standard gene sequencing, can find most BRCA mutations. There are other types of mutations called rearrangements, which include deletions or duplications in BRCA1 and BRCA2 that also may cause an increased risk for these cancers. Testing is also available for large rearrangements in BRCA1 and BRCA2.
After initial BRCA1 and BRCA2 genetic testing, additional testing may be recommended if:
- The results were negative, meaning no genetic mutation was detected
- A variant of uncertain significance was detected, which means that there is a genetic change, but it is not known how that change could affect cancer risk
Talk with your health care team and/or a genetic counselor for more information.
Most, but not all, insurance providers, including Medicare and Medicaid, cover the cost of complete BRCA1 and BRCA2 testing. Many genetic specialists offer multigene panels, which may include 6, 20, 40, or more genes depending on your personal and family history. The multigene panel tests may often be done at the same time as BRCA1 and BRCA2 testing. Talk with your genetic counselor for more information on the type of testing you will have and your insurance coverage before testing begins.
Common Breast Cancer Mutations
Researchers have identified several key gene changes linked to breast cancer. Some of these pose a high risk, while others seem to be less significant.
BRCA1 and BRCA2
The BRCA1 and BRCA2 inherited gene mutations are the most common cause of hereditary breast cancer. Mistakes in these genes account for up to 10% of all breast cancers. BRCA mutations also raise your chances for ovarian cancer, pancreatic cancer, and, in men, prostate cancer. A BRCA mutation may raise your chances of colon cancer. Women with a BRCA1 or BRCA2 mutation have up to a 72% chance of breast cancer during their lifetime.
PALB2
Normally, the PALB2 gene makes a protein that works with the BRCA2 gene protein to repair damaged DNA and stop tumor growth. But defects in the gene can lead to a higher likelihood of breast cancer. Some studies suggest that women with a PALB2 mutation have a 14% chance of breast cancer by age 50 and a 35% chance by age 70.
PIK3CA
HER2
The HER2 gene makes a protein called HER2 . This protein is found on the surface of all breast cells and that helps them grow. If the HER2 gene malfunctions and makes too many copies of itself, it tells cells to make too much HER2 protein. This causes the cells to grow out of control.
PTEN
TP53
CDH1
Researchers have discovered many other genes related to breast cancer.
Changes in the following genes may also raise your chances:
- BARD1
Read Also: Stage 3 Invasive Ductal Carcinoma
Genetic Testing For Cancer
If youre concerned about your cancer risk due to your family history, a healthcare provider can help you determine whether genetic testing for cancer is right for you. Depending on your individual situation, the results of your genetic testing may empower you to take steps to reduce your risk or to schedule cancer screenings for earlier detection and treatment.
That said, genetic testing is not alwayshelpful and cant predict the futurewhich means your test results could also lead to stress and anxiety or even a misunderstanding of the results. According to the American Cancer Society , its best to talk to a trained genetic counselor rather than diving in on your own with an at-home genetic test.
Evaluation Of Suspected Hereditary Predisposition To Breast Cancer
Individuals with a family and personal history suspicious for a familial syndrome should be referred to a genetic counselor for a comprehensive evaluation. Testing for mutations in cancer-associated genes is individually based, and requires a high index of suspicion for a particular gene based on the clinical situation. In general, when a family history is suggestive, it is best to test the individual with a cancer diagnosis, as this increases the probability of a positive test result. Standard clinical BRCA1 and BRCA2 testing has been carried out using PCR amplification and Sanger sequencing. For the Ashkenazi Jewish population, testing can be initially targeted to the three major founder mutations. In 2007, testing for large rearrangements was added for secondary analysis after research studies published that 6%18% of individuals who are BRCA mutation negative by sequencing can be explained by large insertions and deletions in the BRCA1 and BRCA2 genes using multiplex ligation-dependent probe amplification technology . If a mutation is identified, targeted testing can be done for other members of the family to assess risk. Possible outcomes of genetic testing are a true positive, a true negative , uninformative , or a variant of unknown significance . By definition, a VUS is a detected genetic change without a good description of any correlating clinical risk.
Recommended Reading: Life Expectancy Of Breast Cancer Survivors
Is Breast Cancer Hereditary
If one of your close family members, such as your mother, father, sister or daughter, has been diagnosed with breast cancer, you may have concerns about your own chances of developing breast cancer.
If youve been diagnosed with breast cancer yourself, you may worry about what this means for other members of your family.
How Common Are Breast Cancer Gene Mutations
Breast cancer gene mutations arent common in the general population, Dr. Eng says, but they are common in people who have breast cancer. About 10% to 15% of people with breast cancer have one of the breast cancer gene mutations.
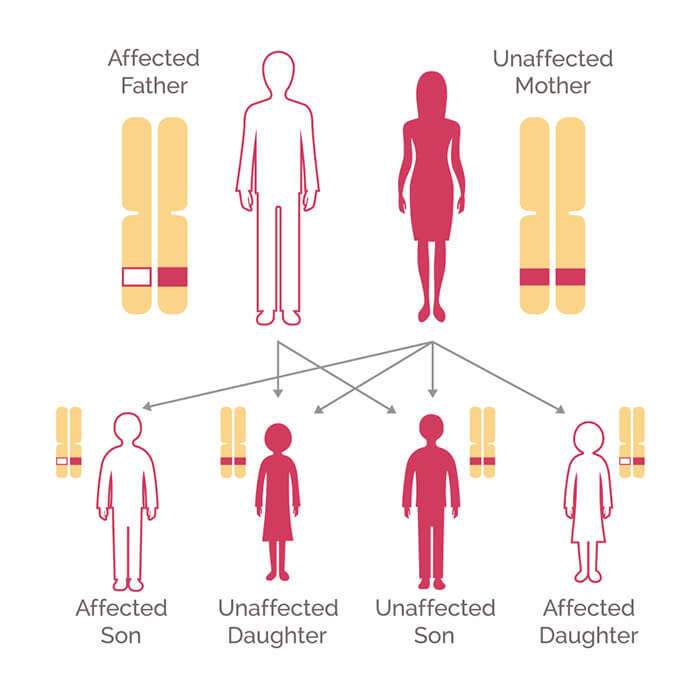
You can inherit these gene mutations from either of your biological parents, and the cancers theyre linked to can affect both men and women so consider all your relatives when thinking about your family history.
Recommended Reading: What Causes Hormonal Breast Cancer
Is Breast Cancer A Genetic Disease
Yes, some breast cancers occur as a result of inheriting genes that contain certain mutations. But, hereditary breast cancer accounts for only 5 to 10% of all breast cancer diagnoses. Among these diagnoses, a family may have one of these inherited gene mutations or genetic conditions that increase their cancer risk:
- BRCA1 or BRCA2. Mutations of these genes are related to an increased risk for breast and ovarian cancer
- Li-Fraumeni Syndrome is caused by mutations in the TP53 gene
- Cowden Syndrome caused by mutations in the PTEN gene
- ATM, CHEK2, PALB2. Mutations in these genes are associated with a moderately increased risk for breast cancer
How Accurate Is Genetic Testing For Breast Cancer
Generally speaking, genetic testing is quite accurate at detecting known genetic variants. But these tests cannot tell you whether youll eventually develop breast cancer.
Receiving a positive result means that, compared to the general population, youre at an increased risk of developing breast cancer. Different gene variations can be linked to different levels of risk.
A positive result doesnt mean that youre certain to get breast cancer in the future. In fact, its possible youll never develop breast cancer. Your genetic counselor can give you a better idea of your breast cancer risk.
Similarly, a negative result doesnt mean that youll never develop breast cancer.
Tests dont always cover a broad range of gene variations. Its possible that you may have a harmful variation that wasnt covered by your test.
Recommended Reading: Can Breast Cancer Cause Stomach Pain
Combinations Of Polymorphisms In Different Genes
One study examined the four polymorphisms in the CYP1A1 gene and the GSTM1 and GSTT1 polymorphisms. None of these polymorphisms, either separately or combined, was associated with increased breast cancer risks. Others analysed a combination of the m2 polymorphism in the CYP1A1 gene and the GSTM1 polymorphism and again no associations were found. One study examined the m1 polymorphisms in the CYP1A1 gene and the polymorphisms in the CYP17 and COMT genes. The presence of at least two putative high risk genotypes was associated with an increased risk of breast cancer .
In conclusion, in a few studies with small sample sizes, combinations of polymorphisms were examined.
Low Expression Of Brca1 In Breast And Ovarian Cancers

BRCA1 expression is reduced or undetectable in the majority of high grade, ductal breast cancers. It has long been noted that loss of BRCA1 activity, either by germ-line mutations or by down-regulation of gene expression, leads to tumor formation in specific target tissues. In particular, decreased BRCA1 expression contributes to both sporadic and inherited breast tumor progression. Reduced expression of BRCA1 is tumorigenic because it plays an important role in the repair of DNA damages, especially double-strand breaks, by the potentially error-free pathway of homologous recombination. Since cells that lack the BRCA1 protein tend to repair DNA damages by alternative more error-prone mechanisms, the reduction or silencing of this protein generates mutations and gross chromosomal rearrangements that can lead to progression to breast cancer.
Recommended Reading: Signs And Symptoms Of Breast Cancer Stage 1
How Does Genetic Testing For Breast Cancer Work
Genetic testing for breast cancer risk typically uses a sample of blood, saliva, or cells from the inside of your cheek. After the sample is collected, its sent to a lab specializing in genetic testing to be analyzed.
Several gene variations that increase breast cancer risk have been found. The most important are those in the BRCA1 and BRCA2 genes. According to the National Cancer Institute, about people have a harmful BRCA variation.
About of females with harmful BRCA1 and 45 to 69 percent of females with harmful BRCA2 variations will develop breast cancer by age 80. Their risk of getting breast cancer in the other breast is also higher.
Other gene variants that may raise breast cancer risk include:
- PALB2
. A healthcare professional or genetic counselor will contact you and discuss your results.
Results you can receive include:
- Positive: A known gene variation that increases your risk of breast cancer was detected.
- Negative: A known gene variation that raises your risk of breast cancer was not detected.
- Variant of unknown significance: A variant has been found in a gene, such as BRCA1 or BRCA2, but its impact on breast cancer risk is currently unknown.
Genetic testing results can be complex. Work with a genetic counselor to help understand what your results mean, so you can plan for next steps.
How Much Does An Inherited Harmful Variant In Brca1 Or Brca2 Increase A Womans Risk Of Breast And Ovarian Cancer
A womans lifetime risk of developing breast and/or ovarian cancer is markedly increased if she inherits a harmful variant in BRCA1 or BRCA2, but the degree of increase varies depending on the mutation.
Breast cancer: About 13% of women in the general population will develop breast cancer sometime during their lives . By contrast, 55%72% of women who inherit a harmful BRCA1 variant and 45%69% of women who inherit a harmful BRCA2 variant will develop breast cancer by 7080 years of age . The risk for any one woman depends on a number of factors, some of which have not been fully characterized.
Like women with breast cancer in general, those with harmful BRCA1 or BRCA2 variants also have an increased risk of developing cancer in the opposite breast in the years following a breast cancer diagnosis . The risk of contralateral breast cancer increases with the time since a first breast cancer, reaching 20%30% at 10 years of follow-up and 40%50% at 20 years, depending on the gene involved.
Ovarian cancer: About 1.2% of women in the general population will develop ovarian cancer sometime during their lives . By contrast, 39%44% of women who inherit a harmful BRCA1 variant and 11%17% of women who inherit a harmful BRCA2 variant will develop ovarian cancer by 7080 years of age .
Also Check: What Organs Does Breast Cancer Affect
How Do I Decide Whether To Be Tested
Given the limitations of testing for hereditary breast cancer, should an individual at high risk get tested? Genetic counselors can help individuals and families make decisions regarding testing.
For those who do test positive for the BRCA1 or BRCA2 gene, surveillance can help detect the disease at an early stage. A woman who tests positive can also consider taking the drug tamoxifen, which has been found to reduce the risk of developing breast cancer by almost 50 percent in women at high risk. Clinical trials are now under way to determine whether another drug, raloxifene, is also effective in preventing breast cancer.
What Is Hereditary Breast And Ovarian Cancer
A diagnosis of Hereditary Breast and Ovarian Cancer Syndrome is considered when there are multiple cases of breast cancer and/or ovarian cancer on the same side of the family. The chance that a family has HBOC increases in any of these situations:
-
1 or more women are diagnosed at age 45 or younger
-
1 or more women are diagnosed with breast cancer before age 50 with an additional family history of cancer, such as prostate cancer, melanoma, and pancreatic cancer
-
There are breast and/or ovarian cancers in multiple generations on the same side of the family, such as having both a grandmother and an aunt on the fathers side both diagnosed with these cancers
-
A woman is diagnosed with a second breast cancer in the same or the other breast or has both breast and ovarian cancers
-
A male relative is diagnosed with breast cancer
-
There is a history of breast cancer, ovarian cancer, prostate cancer, and/or pancreatic cancer on the same side of the family
-
Having Ashkenazi Jewish ancestry
You May Like: Nipple Piercing Breast Cancer
Brca1 Promoter Hypermethylation In Breast And Ovarian Cancer
BRCA1promoter hypermethylation was present in only 13% of unselected primary breast carcinomas. Similarly, BRCA1 promoter hypermethylation was present in only 5% to 15% of EOC cases.
Thus, while BRCA1 expression is low in these cancers, BRCA1 promoter methylation is only a minor cause of reduced expression.
Family History Of Breast Cancer And Inherited Genes
Some people have a higher risk of developing breast cancer than the general population because other members of their family have had particular cancers. This is called a family history of cancer.
Having a mother, sister or daughter diagnosed with breast cancer approximately doubles the risk of breast cancer. This risk is higher when more close relatives have breast cancer, or if a relative developed breast cancer under the age of 50. But most women who have a close relative with breast cancer will never develop it.
UK guidelines help GPs to identify people who might have an increased risk of cancer due to their family history.
Also Check: Red Mill Baking Soda Cancer
Who Should Be Tested For Hboc
Most breast and ovarian cancers occur by chance with no known cause, so testing for BRCA1 or BRCA2 gene mutations may not be beneficial for the average person. Genetic testing is recommended primarily for people who have a personal and/or family history that suggests HBOC. However, women younger than 60 with triple-negative breast cancer , are at risk of having a BRCA mutation, regardless of family history.
For women with a previous diagnosis of breast cancer or ovarian cancer and/or a family history of breast or ovarian cancer, the National Comprehensive Cancer Network provides recommendations for when genetic counseling and testing may be needed. These recommendations are based on your familys history of cancer and how closely related you are to the person who developed cancer. Here are some important definitions to know:
-
“First-degree relatives” include parents, siblings, and children.
-
“Second-degree relatives” include aunts/uncles, grandparents, grandchildren, and nieces/nephews.
-
“Third-degree relatives” include first cousins, great-grandparents, or great-grandchildren.
Genetic testing should be considered if a person or family meets 1 or more of the criteria listed below:
How Can A Person Who Has Inherited A Harmful Brca1 Or Brca2 Gene Variant Reduce Their Risk Of Cancer
Several options are available for reducing cancer risk in individuals who have inherited a harmful BRCA1 or BRCA2 variant. These include enhanced screening, risk-reducing surgery , and chemoprevention.
Enhanced screening. Some women who test positive for harmful BRCA1 and BRCA2 variants may choose to start breast cancer screening at younger ages, have more frequent screening than is recommended for women with an average risk of breast cancer, or have screening with magnetic resonance imaging in addition to mammography.
No effective ovarian cancer screening methods are known. Some groups recommend transvaginal ultrasound, blood tests for the CA-125 antigen , and clinical examinations for ovarian cancer screening in women with harmful BRCA1 or BRCA2 variants. However, none of these methods appear to detect ovarian tumors at an early enough stage to improve long-term survival .
The benefits of screening men who carry harmful variants in BRCA1 or BRCA2 for breast and other cancers are not known. Some expert groups recommend that such men undergo regular annual clinical breast exams starting at age 35 . The National Comprehensive Cancer Network guidelines recommend that men with harmful germline variants in BRCA1 or BRCA2 consider having a discussion with their doctor about prostate-specific antigen testing for prostate cancer screening starting at age 40 .
You May Like: Did Anne Hathaway Have Cancer