Mechanism Of Action Of Her2
As discussed above, the HER2 receptor is a transmembrane tyrosine kinase receptor that belongs to the human epidermal growth factor receptors . It is expressed at a low level on the surface of epithelial cells, and is needed for development in several tissue types, such as the breast, ovary, central nervous system, lung, liver and kidney . It is overexpressed in 2530% of breast cancer cells. As shown in Figure 1, HER2 forms homodimers or heterodimers with other members of the human epidermal growth factor receptors. The HER2 protein can exist in an inactivated state, and dimerize independent of the binding of a ligand. The binding of a ligand induces phosphorylation of the receptors, which in turn activates the MAPK pathway and the PI3K pathways.
HER2 signaling pathway, mechanism of action of targeted therapies, and resistance mechanisms. 1. The truncated P95HER2 isoform results in the loss of the extracellular binding site for trastuzumab. 2.3. Overexpression of other tyrosine kinase receptors, such as IGF1-R and C-met, can continue to trigger downstream signaling despite blockade by trastuzumab. 4. Mutations or loss of PTEN constitutively activates the PI3K signaling pathway.
Questions To Ask Your Doctor About Her2
- What are my treatment options?
- What is the best course of treatment for my cancer, and why?
- Whats the overall goal of treatment in my case?
- When should I start treatment?
- Can I still work and manage my regular activities during this time?
- How often will I be coming in to see you for treatment?
- Will I be coming here for all my visits and treatments, or going elsewhere?
- What short-term side effects and long-term risks are associated with my treatment?
- What are the next steps if the desired treatment doesnt work?
- How likely is it for my cancer to come back in the future? What symptoms should I be aware of?
- What is the cost of my treatment?
- What should I discuss with my insurance company?
What Are The Symptoms Of Her2
Its not possible to self-determine whether you have HER2-positive breast cancer. If your doctor suspects cancer, further testing will reveal whether you are HER2-positive.
Overall, its important to see your doctor right away if you notice any of the following symptoms:
- any new or changing lumps in your breast or armpit areas
- clear, colored, or bloody nipple discharge
- unexplained pain in your breasts
- changes in your nipples or breast skin, such as dimpling, reddening, or scaliness
- nipples that turn inward
Hormone treatments may be an option for cancer thats also HR-positive.
Also Check: Can Baby Powder Cause Breast Cancer
What Tumor Factors Threaten My Life More
There are important tumor biology factors not well reflected in survival statistics by breast cancer stage. Below we list a few important factors that carry a higher risk to life beyond just the stage of cancer. You must ask your surgeon or medical oncologist to explain your receptor status and give you a copy of your biopsy pathology report.
Triple Negative Receptor breast cancer
Triple negative breast cancer is considered a more aggressive breast cancer. Invariably it does require chemotherapy. If you have triple negative breast cancer the risk of dying is higher than the standard statistics usually quoted for a particular stage of breast cancer . Learn more about Triple Negative Breast Cancer with our video lesson
HER2-Positive breast cancer
HER2-positive breast cancers are also more aggressive tumors. But the good news is that we now have incredibly effective, targeted chemotherapy and immunotherapy for HER2-positive cancers. Our video lesson covers HER2-Positive Breast Cancer in more detail .
Breast Cancer at a Young Age
Women younger than 40 have a higher chance of being diagnosed with a more advanced stage breast cancer. Also, the specific cancer type younger women develop has a higher chance of being more aggressive . As a result, age is a relative risk factor for survival.
Untreated breast cancer
Teaching everyone to be an expert in their own breast cancer care.
Survival Rates And Mortality Rates
Survival depends on mortality. You start with 100 percent of the people in the group.
100 percent mortality rate = survival rate
Say, the mortality rate in the group of people is 5 percent. Survival would be 95 percent .
Similarly, the number of people in a group who survive depends on the number of people who die. Say, 500 people are in the group and 1 person dies. This means 499 people survived .
Don’t Miss: Where Can Breast Cancer Be
What This Means For You
If youve been diagnosed with metastatic HER2-positive breast cancer that has grown while being treated with an anti-HER2 medicine and chemotherapy, and you and your doctor are considering second-line treatments, these results are extremely promising. You may want to bring up this study and ask if Enhertu is a good option for you.
If you decide that Enhertu is right for you and your unique situation, its important to know that interstitial lung disease can be a severe side effect of the medicine. You should be closely monitored for signs of interstitial lung disease and tell your doctor right away if you experience:
Histological Grade And Ki67
Histological grade information was available from the ICD-O-3 code and categorized as low , intermediate and high according to the Elston-Ellis modification of the Scarff-Bloom-Richardson grading system . Women with anaplastic carcinoma were excluded, leaving n=24,137 women for the analysis . Ki67 has been recorded routinely since 2011 and was categorized as low , intermediate or high according to cutoffs in the Norwegian treatment guidelines .
Read Also: Signs Of Men Breast Cancer
Hormone Receptor Positive And Her2+ Mbc
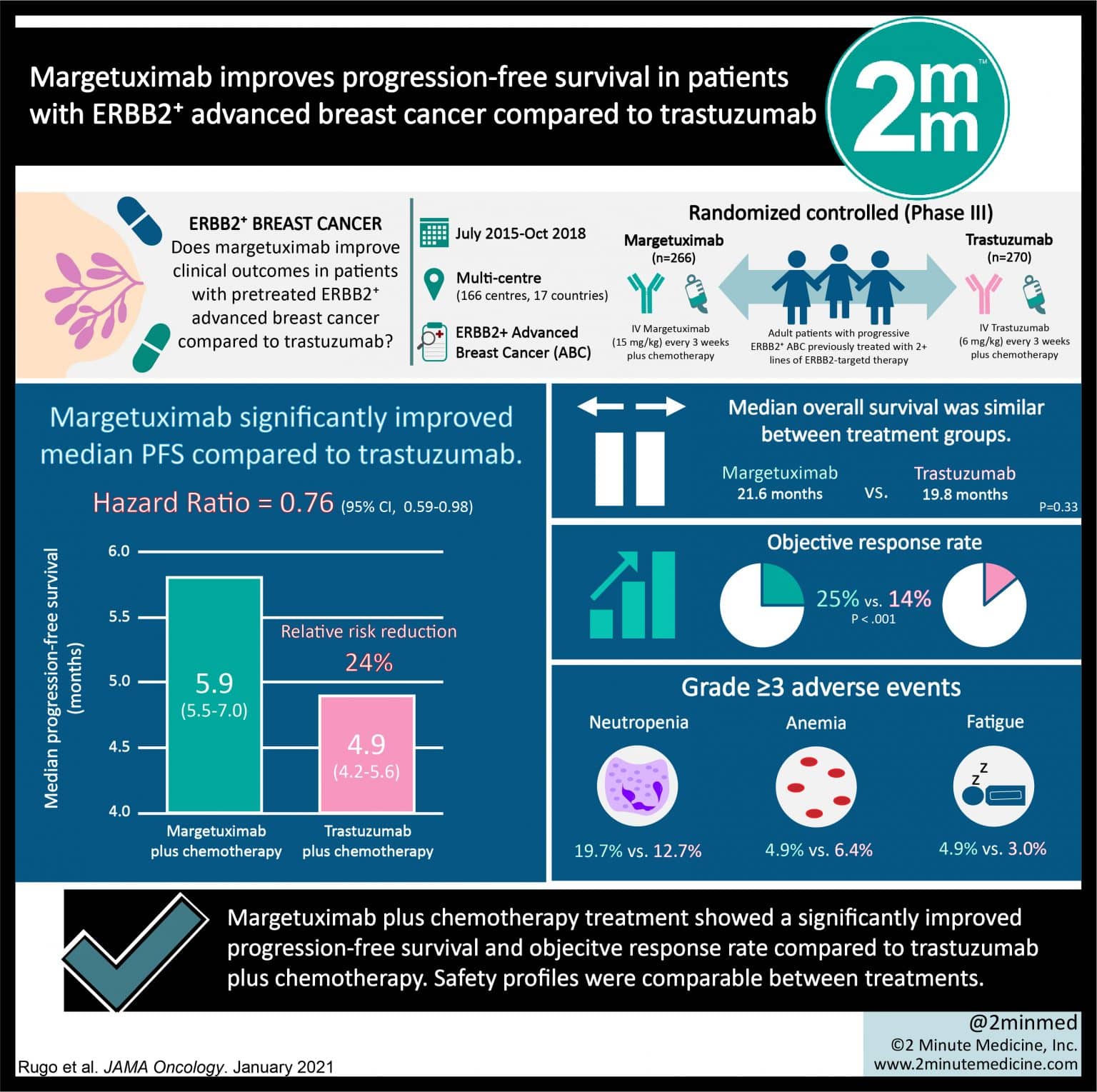
About 50% of the HER2+ patients are also hormone receptor positive . There are important biological differences underlying pure HER2+/hormone receptor negative tumours and HER2+/HR+ tumours. When HR is overexpressed, the molecular profile of these tumours resembles the so-called luminal B subtype of breast cancer . Cross-talk between HER2 and HR leads to resistance to hormonal agents, and resistance can be partially overcome by anti-HER2 therapies. In the phase III Trastuzumab and Anastrozole Directed Against oestrogen receptor -Positive HER2-Positive Mammary Carcinoma trial, 207 postmenopausal women with HER2+/HR+ disease were assigned to anastrozole alone or with trastuzumab. The combination arm showed significant improvement in PFS but not in the OS. However, there was a 70% cross-over rate to the combination arm in this study . Similarly, combination of letrozole with lapatinib was found to be more effective than letrozole alone in patients with HER2+/HR+ MBC . It is an acceptable approach to start with a combination of an anti-oestrogen and an anti-HER2 therapy in the metastatic setting especially if the disease burden is limited without visceral crisis.
Tumour Size Nodal Status And Tnm Stage
Pathologic T and N status was coded according to AJCC 4th edition for 20052008 and AJCC 6th edition for 20082015 and categorized as pT1 , pT2 , pT3 , pT4, pN0 , pN1 , pN2 , pN3 and pN+ , and combined as pT1pN0, pT2pN0, pT1-2pN+ and pT3-4pN0/+ according to Norwegian treatment guidelines. Patients receiving neoadjuvant treatment were missing pTN status. Pathologic TNM stage was categorized into I, IIA, IIB, IIIA, IIIB or IV . This was combined with a SEER summary stage variable based on clinical data when pTNM missing into a TNM stage variable .
Recommended Reading: Is Malignant Breast Cancer Curable
Availability Of Data And Materials
The dataset analysed in the current study is not publicly available, but was obtained from the Cancer Registry of Norway under a specific ethical approval by the Regional Committee for Medical and Health Research Ethics in the South East Health Region of Norway. Researchers with appropriate approvals can apply for Norwegian health registry data from .
Living With Stage : The Breast Cancer No One Understands
Editor’s note: We’re bringing back this piece from October 2014 for Metastatic Breast Cancer Awareness Day and to honor Jody Schoger, featured in the story. Schoger died of metastatic breast cancer in May. Want to learn more about MBC? Look for our tweets at the Northwest Metastatic Breast Cancer Conference this Saturday at Fred Hutch.
A no-nonsense Texan of 60 years, Jody Schoger* has a very no-nonsense way of educating people about her metastatic breast cancer.
âSomeone will say, âWhen are you done with treatment?â and Iâll tell them, âWhen Iâm dead,ââ said Schoger, a writer and cancer advocate who lives near Houston. âSo many people interpret survivorship as going across the board. That everybody survives cancer now. But everybody does not survive cancer.â
An estimated 155,000-plus women in the U.S. currently live with âmets,â or metastatic breast cancer. This type of cancer, also called stage 4 breast cancer, means the cancer has metastasized, or traveled, through the bloodstream to create tumors in the liver, lungs, brain, bones and/or other parts of the body. Between 20 and 30 percent of women with early stage breast cancer go on to develop metastatic disease. While treatable, metastatic breast cancer cannot be cured. The five-year survival rate for stage 4 breast cancer is 22 percent median survival is three years. Annually, the disease takes 40,000 lives.
Read Also: Can Breast Cancer Cause Fatigue
Mortality Rates Versus Number Of Breast Cancer Deaths
Sometimes its useful to have an estimate of the number of people expected to die from breast cancer in a year. This numbers helps show the burden of breast cancer in a group of people.
Numbers, however, can be hard to compare to each other. To compare mortality rates in different populations, we need to look at mortality rates rather than the number of breast cancer deaths.
Ongoing Trials In First
Improving outcomes in the first-line setting is always important for patients with MBC, especially if survival rates are significantly improved. The MARIANNE trial is evaluating the role of first-line T-DM1 in HER2+ MBC. More than 1000 patients have been randomized to one of the three arms, taxane plus trastuzumab, T-DM1 alone or T-DM1 plus pertuzumab. Results of this trial are awaited with great interest because they may change clinical practice.
You May Like: How To Help Someone With Breast Cancer
Subcutaneous Herceptin Now An Option
Dr. Jackisch M.D. and colleagues from Germany reported the results of an open-label, multi-center, international clinical trial to compare the effectiveness and safety of subcutaneous and IV Herceptin in patients with HER2-positive ESBC.
A total of 596 individuals were enrolled in the clinical trial between October 19, 2009, and December 1, 2010 and have now been followed for 6 years.
Patients were given 8 cycles of standard chemotherapy and either a fixed-dose of subcutaneous or IV Herceptin for 10 after surgery to complete 1 year of anti-HER2 therapy.
The overall survival and progression free survival were essentially identical for IV and subcutaneous Herceptin. Moreover, the rates of significant cardiac and other serious side effects were similar.
The study suggests that subcutaneous Herceptin is as an effective alternative route of administration for patients with HER2-positive ESBC.16
References:
Taxol/herceptin Effective In Stage I Her2
The combination of Taxol® and Herceptin® followed by Herceptin alone showed benefit and was well tolerated by women with stage I HER2-positive, node-negative breast cancer.
The APT study included 406 women with HER2-positive, node-negative tumors that measured less than 3 cm. The study was a nonrandomized prospective trial to define the outcomes in a uniformly treated cohort. Patients received Taxol/Herceptin for 12 weeks followed by 9 months of Herceptin.
After a median follow-up of 3.6 years, disease-free survival was 98.7 percent and recurrence or death occurred in 2.5 percent of patients. There were no new contralateral primary breast cancers. Distant recurrences were observed in two patients. By hormone receptor status, disease-free survival rates were 98.5 percent in receptor-positive patients and 99.2 percent in receptor-negative patients.
Two patients developed symptomatic congestive heart failure. Few other adverse events were noted.
The limitations of the study were that it was a non-randomized, single-arm study and about 20 percent of patients had T1a tumors, which are already associated with a favorable prognosis. Still, the researchers concluded that this adjuvant regimen should be considered a standard strategy to prevent recurrence in stage I HER2-positive, node-negative breast cancer.15
Recommended Reading: Will You Die From Stage 4 Breast Cancer
Understanding Breast Cancer Survival Rates
Prognosis varies by stage of breast cancer.
Non-invasive and early-stage invasive breast cancers have a better prognosis than later stage cancers .
Breast cancer thats only in the breast and has not spread to the lymph nodes has a better prognosis than breast cancer thats spread to the lymph nodes.
The poorest prognosis is for metastatic breast cancer . This is when the cancer has spread beyond the breast and nearby lymph nodes to other parts of the body.
Learn more about breast cancer treatment.
Cancer And The Female Breast
Figure: Breast and Adjacent Lymph Nodes
Figure: The female breast along with lymph nodes and vessels. An inset shows a close-up view of the breast with the following parts labeled: lobules, lobe, ducts, nipple, areola, and fat.
Inside a woman’s breast are 15 to 20 sections, or lobes. Each lobe is made of many smaller sections called lobules. Fibrous tissue and fat fill the spaces between the lobules and ducts . Breast cancer occurs when cells in the breast grow out of control and form a growth or tumor. Tumors may be cancerous or not cancerous .
Additional Information
Kohler BA, Sherman RL, Howlader N, Jemal A, Ryerson AB, Henry KA, Boscoe FP, Cronin KA, Lake A, Noone AM, Henley SJ, Eheman CR, Anderson RN, Penberthy L. Annual Report to the Nation on the Status of Cancer, 1975-2011, Featuring Incidence of Breast Cancer Subtypes by Race/Ethnicity, Poverty, and State. J Natl Cancer Inst. 2015 Mar 30 107:djv048. doi: 10.1093/jnci/djv048. Print 2015 Jun.
Read Also: Can Teenage Girl Get Breast Cancer
What Is The Outlook
According to research estimates, more than 3.5 million women in the United States have a history of breast cancer.
The outlook for people with HER2-positive breast cancer varies. Advancements in targeted therapies continue to improve the outlook for people with early stage or metastatic disease.
Once treatment for nonmetastatic breast cancer ends, youll still need periodic testing for signs of recurrence. Most side effects of treatment will improve over time, but some may be permanent. You can work with your healthcare team to manage any lasting effects.
Metastatic breast cancer isnt considered curable. Rather, treatment relieves and manages symptoms, and can continue as long as its working. If a particular treatment stops working, you can switch to another.
Er Pr Her2 And Ihc Subtypes
Information on ER, PR and HER2 status was obtained from pathology reports for the whole study period . From 2005 to January 2010, tumours were classified as ER negative if < 10% ER expression, and from February 2010 onwards if < 1% ER expression. PR-negative tumours were defined as < 10% PR expression throughout the study period. HER2 expression was routinely assessed with IHC and verified with in situ hybridization if the IHC results were borderline. We created six IHC subtypes: ER+PR+HER2, ER+PRHER2, ER+PR+HER2+, ER+PRHER2+, ERPRHER2+ and ERPRHER2 . Women with the rarer combinations ERPR+HER2 or ERPR+HER2+ were set to missing in the analysis . In total, n =21,786 women had known IHC subtype, while n =2351 women lacked information on ER, PR or HER2 status .
Table 1 Clinicopathologic characteristics by IHC subtype for women with invasive breast cancer, Norway 20052015 age 2074 years
Recommended Reading: Who Is More Likely To Get Breast Cancer
Survival Rates And Statistics
A relative survival rate helps give an idea of how long a person with a particular condition will live after receiving a diagnosis compared with those without the condition.
For example, if the 5-year relative survival rate is 70%, it means that a person with the condition is 70% as likely to live for 5 years as someone without the condition.
It is important to remember that these figures are estimates. A person can talk with a doctor about how their condition is likely to affect them.
Some factors affecting a personâs survival rate with breast cancer include:
- individual factors, such as the personâs age and overall health
- the stage of the cancer at diagnosis
- the treatment the person receives
HER2-positive cancers are than HER2-negative cancers. With treatment, however, the chances of survival are high, especially with an early diagnosis. In some cases, they may be higher than for HER2-negative breast cancer due to effective targeted treatment.
According to the , the likelihood of living for another 5 years with HER2-positive cancer, compared with a person who does not have breast cancer, is as follows. These statistics are based on figures for the years 2011â2017.
| Stage |
|---|
What Do The Test Results Mean
The results of HER2 testing will guide you and your cancer care team in making the best treatment decisions.
It is not clear if one test is more accurate than the other, but FISH is more expensive and takes longer to get the results. Often the IHC test is done first.
- If the IHC result is 0, the cancer is considered HER2-negative. These cancers do not respond to treatment with drugs that target HER2.
- If the IHC result is 1+, the cancer is considered HER2-negative. These cancers do not usually respond to treatment with drugs that target HER2, but new research shows that certain HER2 drugs might help in some cases .
- If the IHC result is 2+, the HER2 status of the tumor is not clear and is called “equivocal.” This means that the HER2 status needs to be tested with FISH to clarify the result.
- If the IHC result is 3+, the cancer is HER2-positive. These cancers are usually treated with drugs that target HER2.
Some breast cancers that have an IHC result of 1+ or an IHC result of 2+ along with a negative FISH test might be called HER2-low cancers. These breast cancers are still being studied but appear to benefit from certain HER2-targeted drugs.
Triple-negative breast tumors dont have too much HER2 and also dont have estrogen or progesterone receptors. They are HER2-, ER-, and PR-negative. Hormone therapy and drugs that target HER2 are not helpful in treating these cancers. See Triple-negative Breast Cancer to learn more.
Recommended Reading: What Is Breast Cancer Index