Benefits Of Mammographic Screening
The ACS systematic review also examined the effect of screening mammography on life expectancy. Although the review concluded that there was high-quality evidence that mammographic screening increases life expectancy by decreasing breast cancer mortality, the authors were not able to estimate the size of the increase 23.
Myth #: I Had A Normal Mammogram Last Year So I Dont Need Another One This Year
Fact: Mammography is detection, not prevention. Having a normal mammogram is great news, but it does not guarantee that future mammograms will be normal, says Dr. Zeb. “Having a mammogram every year increases the chance of detecting the cancer when it is small and when it is most easily treated which also improves survival.”
How Accurate Are Mammograms
The diagnostic accuracy for mammograms increases for women over 50 years of age. That means that the older you get, the less likely it is that your mammogram will produce a false positive report. The technology used today can usually detect breast abnormalities before they can be felt during a breast exam.
While mammography is the best method available for early detection of breast cancer and more accurate than breast sonography, its not perfect. Below are some important statistics:
- About 7%-10% of women who have a screening mammogram are asked to come back for more testing .
- An estimated 17% of breast cancers may be missed by mammography. The number may rise as high as 30% for women with dense breasts, making the inclusion of a clinical breast exam in overall diagnosis even more important.
- Combining mammography with a clinical exam can diagnose about 4% more cancers than just mammography.
Recommended Reading: Hormone Therapy For Breast Cancer Stage 4
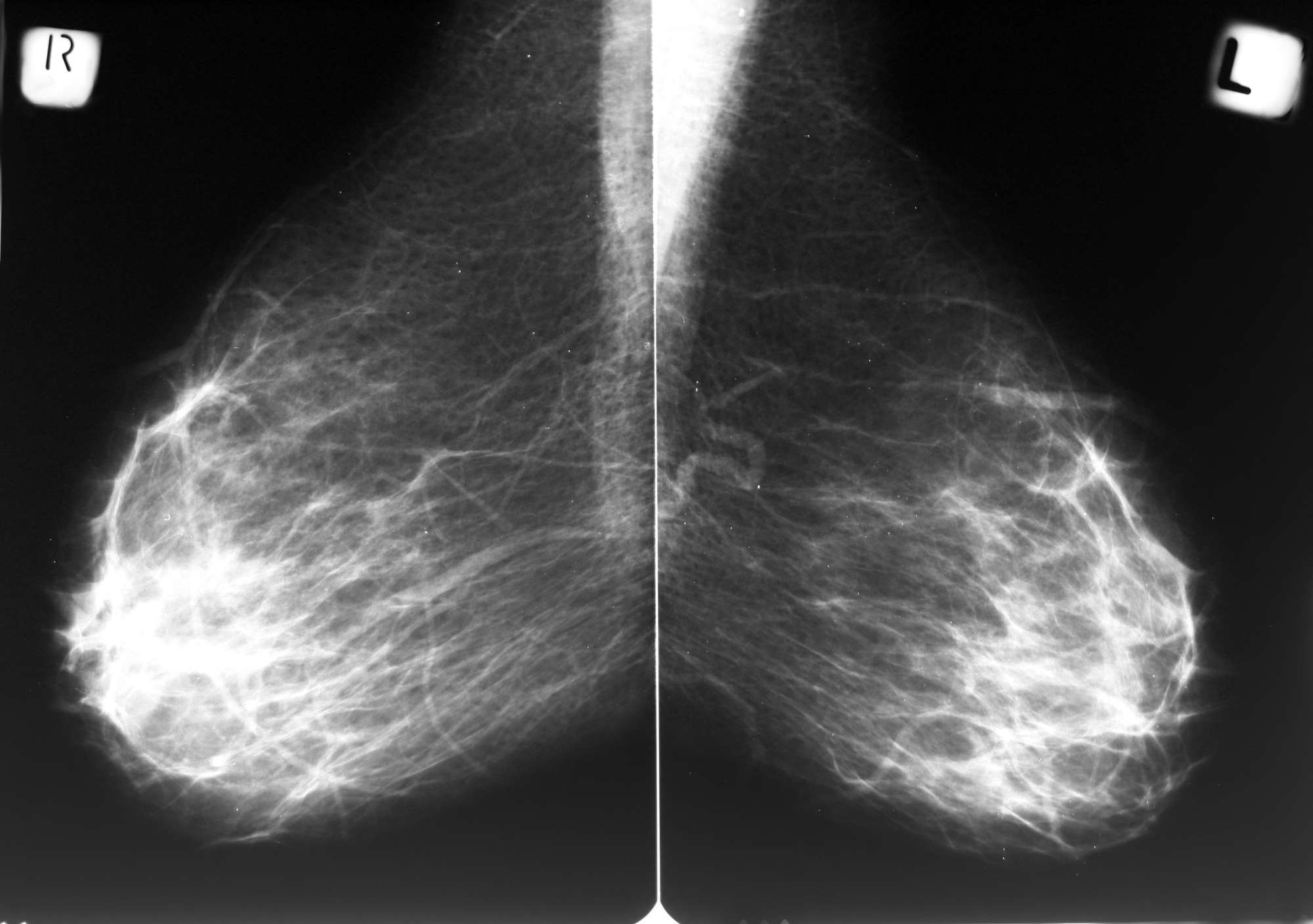
How Does Breast Density Affect Mammography
Young women have a higher proportion of glandular and fibrous tissue compared to fatty tissue. These tissues appear dense and have a light grey or white appearance on a mammogram, while fatty tissue appears darker. Cancers also appear light grey or white so this can make them more difficult to detect amongst the background tissue. This is why mammography is not routinely used for breast screening in young women under the age of 40 .
The proportion of dense glandular tissue naturally declines after menopause making mammograms easier to read. However, women taking hormone replacement therapy have higher breast density, making mammography results less accurate. Annual screening is recommended in this group.
Women with high breast density may also be recommended to have annual rather than two-yearly screening.
Whats The Procedure Like

Getting a mammogram shouldnt take you more than 1 hour. Once you check in for your appointment, you will be guided to an examination area, where you will be asked to remove your clothing above your waist. It can help to wear shirts that are easy to remove and put back on. The facility will provide some type of cover or gown for your mammogram.
You may also be asked ahead of time to not wear any deodorants, perfumes, lotions, or powders during your mammogram. These can make it difficult for the machine to compress your breast tissue, and may show up as white spots on the final pictures.
The mammogram itself wont take long, but the exact time depends on the individual. You should be able to complete your entire appointment in about 30 minutes .
Some people find the scan itself painful due to awkward positioning and the pressure of the two plates on your breast tissue. But this pressure is applied for only a few seconds at a time.
When the scan is complete, you will be able to get dressed and leave your appointment. Dont expect your results right away. Depending on the facility, it can take you a few days to several weeks to receive a final report.
Also Check: Breast Cancer Curable
What Happens If My Mammogram Is Not Normal
An abnormal mammogram does not always mean that there is cancer. You will need to have additional mammograms, tests, or exams before your provider can tell for sure. You may also be referred to a breast specialist or a surgeon. But it does not necessarily mean you have cancer or need surgery. You would see one of these doctors because they are experts in diagnosing breast problems.
Where Can I Go To Get Screened
You can get screened for breast cancer at a clinic, hospital, or doctors office. If you want to be screened for breast cancer, call your doctors office. They can help you schedule an appointment.
Most health insurance plans are required to cover screening mammograms every one to two years for women beginning at age 40 with no out-of-pocket cost .
Are you worried about the cost? CDC offers free or low-cost mammograms. Find out if you qualify.
Recommended Reading: Stage 6 Breast Cancer
Radiation From Ct Scans X
What do you think is more likely to cause breast cancer: chemicals such as BPA, phthalates, and pesticides or imaging tests such as X-rays and CT scans? The surprising answer: the imaging tests, particularly CT scans but also X-rays and even the mammograms used to detect breast cancer.
The Institute of Medicine, the nonprofit health arm of the National Academy of Sciences, reviewed possible causes of breast cancer in 2012 and found that no product or chemical could be conclusively linked to the malignancy. Not so for radiation-based imaging tests. The report, “Breast Cancer and the Environment: A Life Course Approach,” concluded that about 2,800 breast-cancer cases a year among U.S. women stem from medical radiation.
While these represent a small proportion of all breast cancers, theyre important because they can potentially be reduced, said Rebecca Smith-Bindman, M.D., director of the Radiology Outcomes Research Laboratory at the University of California at San Francisco, in an analysis of the findings.
The IOM concluded that one of the most important steps women can take to reduce their breast-cancer risk is to avoid unnecessary imaging tests.
Learn more about the dangers of CT scans and X-rays and check our advice on screening tests for breast cancer and other malignancies.
Is There Any Harm Or Other Risk From Breast Cancer Screening Using Mammography
Finding cancer at an early stage does not always reduce a womans risk of dying from breast cancer. Even though mammography can detect malignant tumours that cannot be felt, treating a small tumour does not always mean that the woman will not die from the cancer. A fast-growing or aggressive cancer may have already spread to other parts of the body before it is detected. Screening might not help prolong the life of women with such tumours, but women with such tumours would live a longer period of time knowing that they may have a fatal disease. In addition, screening mammograms might not help prolong the life of a woman who is suffering from other, more serious health conditions.
X-rays have the potential to cause cancer. Mammograms require small doses of radiation, so the risk of harm from this radiation exposure is low. The benefits of mammography screening in organized programmes outweigh the potential harm from the radiation exposure.
Over a 20-year period, about 1 out of 5 women regularly participating in screening will receive a false-positive result that can be clarified without invasive procedures. Over the same period, about 1 out of 10 women will require an invasive procedure without an operation, and up to about 1 out of 100 women will undergo an operation to check the result of the mammography.
You May Like: Mayo Clinic Breast Cancer Symptoms
Benefits Of Breast Screening
Breast cancers found by screening are generally at an early stage. Very early breast cancers are usually easier to treat, may need less treatment, and are more likely to be cured.
The current evidence suggests that breast screening reduces the number of deaths from breast cancer by about 1,300 a year in the UK.
Almost all women diagnosed with breast cancer at the earliest possible stage survive for at least 5 years after diagnosis and are likely to be cured.
Mammography Selectively Detects More Favorable Tumors
Mammography has a tendency to selectively identify tumors with favorable molecular features, which are features that make breast cancer treatment easier, offering a better prognosis. This is due to the fact that tumors with favorable characteristics tend to grow more slowly, so there is a larger window of time in which they can be detected by screening mammography. When screening mammography is used, these favorable tumors tend to be diagnosed long before they would begin to cause symptoms. This phenomenon is called length-bias sampling and refers to a statistical distortion of results that occurs when screening identifies disease cases before the onset of symptoms, making it appear as though survival time is increased for the particular disease due to screening. However, favorable tumors typically respond to treatment equally effectively at clinical presentation as they do when diagnosed via mammography, so earlier detection through screening mammography does not translate into a reduction in breast cancer mortality .
You May Like: Is Estrogen Positive Breast Cancer Hereditary
Conflicts Of Interest And Mammography Recommendations
There is significant bias in the medical literature regarding mammography. This has led to significant breast cancer overdiagnosis and overtreatment, while also significantly influencing womens perceptions about the purported effectiveness of mammography.
A literature review of 171 articles in the journal Evidence-Based Medicine found that a significant number of studies examining the effectiveness of mammography were published by interest groups and authors with vested interests in mammography screening. Scientific journal articles on breast cancer screening written by authors who have a vested interest in the practice of mammography tend to emphasize the potential benefits of mammography, while downplaying or outright rejecting the major harms such as overdiagnosis and overtreatment. Authors may have a vested interest in promoting mammography if they are receiving income from mammography screening programs or if they are contributing to scientific journals tied to political interest groups such as the American Cancer Society, which has financial ties with the makers of mammography equipment .
Due to conflicts of interest, the research being used to develop recommendations for mammography screening protocols is biased and is not a true representation of the efficacy of mammography for reducing breast cancer mortality. This has had a large-scale impact on the development of mammography screening programs 00393-3/abstract” rel=”nofollow”> 18).
How Is The Procedure Performed
Mammography is performed on an outpatient basis.
During mammography, a specially qualified radiologic technologist will position your breast in the mammography unit. Your breast will be placed on a special platform and compressed with a clear plastic paddle. The technologist will gradually compress your breast.
Breast compression is necessary in order to:
- Even out the breast thickness so that all of the tissue can be visualized.
- Spread out the tissue so that small abnormalities are less likely to be hidden by overlying breast tissue.
- Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged.
- Hold the breast still in order to minimize blurring of the image caused by motion.
- Reduce x-ray scatter to increase sharpness of picture.
You will be asked to change positions between images. The routine views are a top-to-bottom view and an angled side view. The process will be repeated for the other breast. Compression is still necessary for tomosynthesis imaging in order to minimize motion, which degrades the images. During screening breast tomosynthesis, two-dimensional images are also obtained or created from the synthesized 3-D images.
You must hold very still and may need to hold your breath for a few seconds while the technologist takes the x-ray. This helps reduce the possibility of a blurred image. The technologist will walk behind a wall or into the next room to activate the x-ray machine.
The examination process should take about 30 minutes.
You May Like: Symptoms Stage 4 Breast Cancer
Where Can You Get A Mammogram
You can get a mammogram at a hospital, specialty clinic, or doctors office. A primary care doctor or gynecologist can discuss breast cancer screening with you and help you set up an appointment. Some facilities even offer walk-in mammogram screenings
The Food and Drug Administration has also created a national directory of facilities that perform mammograms. You can search the directory by state or zip code.
What Is A Mammogram For Breast Cancer Screening
A mammogram is a type of X-ray used to examine breast tissue for cancers and other irregularities. Similar to a regular X-ray used to look at the structures inside your body, a mammogram uses waves of radiation to produce an image of whats inside your body.
During a mammogram, you wont stand in front of an X-ray machine or have one pass over you. Instead, a mammogram machine uses two plates to compress breast tissue during the scan. This makes the examination area thinner and allows the technicians to capture an image with lower doses of radiation than a traditional X-ray.
Screening mammograms usually take a view of your breast tissue from at least two different angles.
You May Like: Invasive Ductal Carcinoma Grade 3 Treatment
Psychological Harms Of False
Generic questionnaires cannot capture fully the psychological consequences of breast screening.22 A Danish study was therefore based on a specially designed questionnaire that was developed using focus groups.22 Even after three years, women who had experienced a false-positive diagnosis had an anxiety level and other psychological problems that fell between that for women with breast cancer and women who were told they did not have cancer.22 Thus, the psychological harms of screening are substantial and long-lasting, and they affect a huge number of women, as the cumulative risk of a false-positive result after 10 mammograms is in the range of about 20% to 60%.1 Added to this comes the psychological harms inflicted on all the overdiagnosed women who do not know they are overdiagnosed but think they suffer from a fatal disease.
How Often Should I Have A Mammogram
Your risk of breast cancer goes up as you age. But experts disagree about when you should have your first mammogram.
The American Cancer Society recommends that women ages 40 to 44 should have a choice to start yearly screening mammograms. Women 45 to 54 should have a mammogram each year, and those 55 years and over should get mammograms every 1 to 2 years. But the U.S. Preventive Services Task Force recommends screening every 2 years from ages 50 through 74 and says the decision to start yearly screening mammograms before age 50 should be an individual one. Talk with your doctor about when you should start getting them.
If your doctor tells you you’re at high risk for breast cancer, or if you have close family members who got the disease at an early age, you might want to consider getting screened earlier.
Most experts recommend that you continue to have these screenings as long as you are in good health and are expected to live at least another 10 years.
Mammograms are an important part of your health history. If you go to another health care provider or move, take the film with you.
Read Also: Breast Cancer Stage 3 Treatment
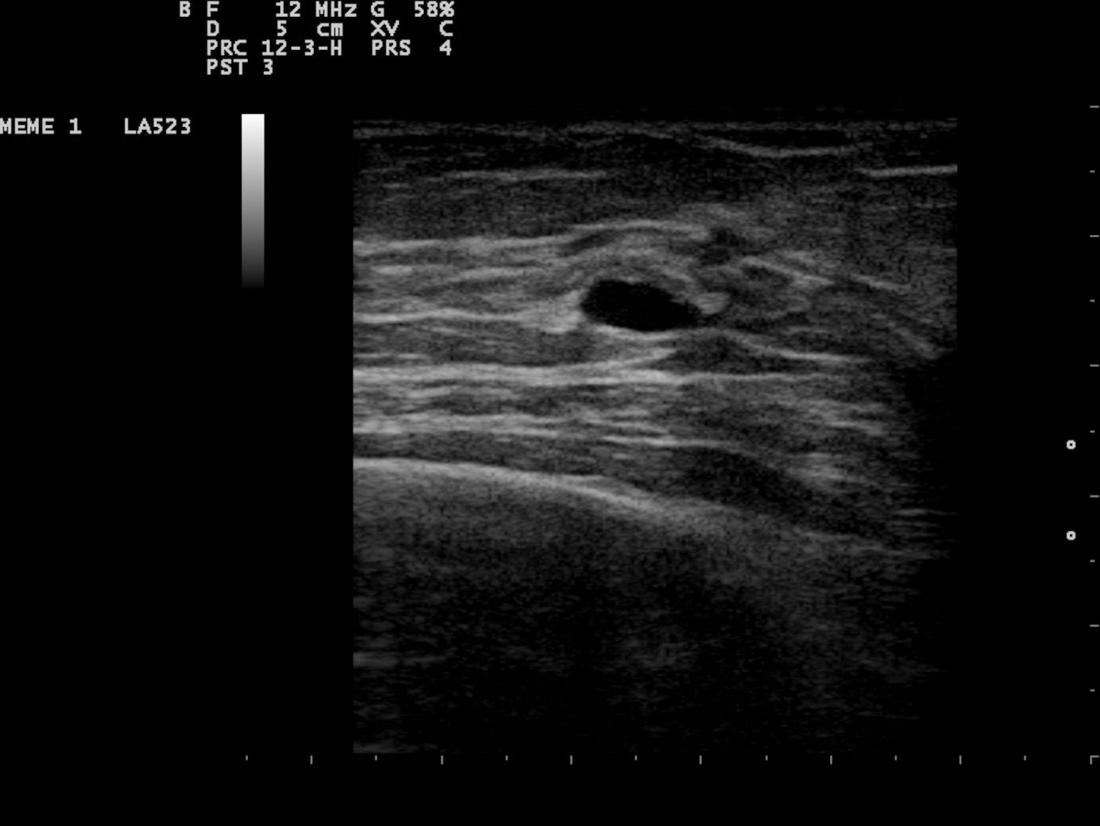
Why Do I Need An Ultrasound After A Mammogram
One of the main reasons your doctor may recommend an ultrasound after a mammogram is if you have dense breast tissue. Dense breast tissue isnt abnormal however, it can make it more difficult for a mammogram to detect cancer cells that may be hidden in the tissue.
An ultrasound can help provide a better diagnose after an abnormal mammogram because:
- A mammogram uses regular X-ray technology. Fatty tissue shows up as gray and dense tissue shows up as white. A cancerous tumor, however, also shows up as white.
- A breast ultrasound uses sound waves that bounce off tissue, with different tissues making different echo patterns. These patterns are studied to detect whether there are any cancer cells or abnormal tissue.
- While a mammogram shows a full picture of the breast and where the dense tissue is located, an ultrasound focuses on that dense tissue and shows what is inside it. It can therefore indicate whether there is a suspicious mass that needs to be confirmed through needle biopsy.
Radiation From Mammography May Increase Risk Of Breast Cancer
The cumulative effect of routine mammography screening may increase womens risk of developing radiation-induced breast cancer . The current recommendations for mammography screening have led women to start screening at a younger age and also to receive more frequent screening this has amplified the amount of radiation to which the breasts are being exposed, and the effects are not trivial. In addition, women who are exposed to radiation for other purposes or women who are carriers of the BRCA gene are at an even higher risk of experiencing adverse effects from mammography radiation .
While not a direct reflection of the impact of mammography on breast cancer risk, other studies examining the effect of diagnostic chest x-rays on breast cancer risk have found that medical radiation exposure increases breast cancer risk .
Also Check: What Is Stage Three Cancer
Myth #: I Dont Have Any Symptoms Of Breast Cancer Or A Family History So I Dont Need To Worry About Having An Annual Mammogram
Fact: The American College of Radiology recommends annual screening mammograms for all women over 40, regardless of symptoms or family history. Early detection is critical, says Dr. Sarah Zeb. If you wait to have a mammogram until you have symptoms of breast cancer, such as a lump or discharge, at that point the cancer may be more advanced . According to the American Cancer Society, early-stage breast cancer has a five-year survival rate of 99 percent. Later-stage cancer has a survival rates of 27 percent.
More than 75 percent of women who have breast cancer have no family history.
Screening Directs Resources Away From Treatment
There are significant harms associated with mammography screening and no reliable evidence of benefit. It is time to discontinue routine mammograms for all healthy women of a particular age. Resources should be shifted toward surveillance of women at higher risk for breast cancer, diagnostic workup for women with a change in their breast that does not go away and for ensuring that women receive timely treatment for a confirmed invasive breast cancer.
Population-based mammography screening has opportunity costs for the health care system, not to mention the social, financial, interpersonal and emotional costs to women and their families.
Recommended Reading: Hr Positive Breast Cancer Treatment