The Cost Of Breast Cancer Genetic Testing
A genetic test for breast cancer does not cost as much as most people believe, including health care professionals. BRCA testing can cost up to $2,000 depending on the lab doing the test.
What is important to know is that most labs will only test for the BRCA genes. They do not look at any other cancer genes. While this genetic information is valuable, it is much too expensive and limited.
When the news of BRCA and its relation to breast cancer, Myriad Genetics patented it, so they were the only ones who could test for the BRCA genes. They monopolized the market, so they were able to charge as much as they wanted.
When the Supreme Court invalidated the patent, more companies were allowed to test for the BRCA genes driving the cost down. Breast cancer genetic testing cost has been reduced so much that most people can now afford it without the help of health insurance.
Taking The Next Step With Genetic Testing
Screening for hereditary cancer is a powerful tool, especially if you have a personal or family history of certain types of cancers such as breast cancer or colorectal cancer. The good news is that this type of testing is readily available for people who could benefit from it. TruGenX is a trusted source for precision medicine, offering genetic testing for cancer screening.
Contact TruGenX if you would like to learn more about how you may benefit from understanding the potential risks you may face in terms of developing cancer and how this testing can positively impact your treatment by allowing you to predict and prevent cancer before symptoms occur.
Medicare Expands Next Generation Sequencing In 2020
Two years later in 2020, CMS expanded coverage for Next Generation Sequencing tests to people with any stage of female breast or ovarian cancer to determine if they have hereditary-associated mutations.
For example, several types of breast cancer exist, and some types are inherited. Genetic testing can help determine whether a patient has an inherited cancer and identify more tailored treatment options.
Unlike CMS earlier determination, Medicare beneficiaries with breast and ovarian cancer who meet the criteria no longer need to be in the advanced stages of cancer to undergo genetic testing.
NGS testing is now also available if you have:
- Ovarian or breast cancer
- A clinical indication for hereditary breast or ovarian cancer
- A high-risk factor for inherited breast or ovarian cancer
According to the national coverage determination, diagnostic tests using NGS must be ordered by a treating physician and analyzed in a certified lab.
The test must also be approved or have clearance from the U.S. Food and Drug Administration, and test results must be provided to the treating physician in a report that specifies treatment options.
People with other cancers may still qualify for Medicare coverage of NGS testing.
Businesses that process Medicare claims in specific regions called Medicare Administrative Contractors can decide on a case-by-case basis whether to cover NGS tests for any cancer at any stage.
Read Also: What Is Estrogen Positive Breast Cancer
Does Medicaid Cover Genetic Testing For Breast Cancer
Medicaid covers genetic testing for breast cancer in all states except three. Those three states are:
These three states do not cover the cost of genetic testing for hereditary cancer risk.
Multigene panel testing is not covered by most Medicaid programs.
Despite Medicaid covering breast cancer genetic testing cost more than Medicare and many health insurance providers, there is still a testing eligibility criteria. This eligibility criterion does differ by state. Genetic counselors help people understand if they meet the Medicaid guidelines for genetic testing in their state.
Does Medicare Cover Genetic Testing For Cancer
Are you at risk of developing cancer? Its a question many think about and are seeking an answer to.
One big risk factor for cancer is genetics. And, thanks to recent scientific advances, genetic testing for cancer is more accurate and widely available than ever.
It could also involve more frequent cancer screenings. The goal there would be to catch cancer as early as possible. Because early detection and treatment can help produce more favorable outcomes for those with cancer.
These tests are also helpful for family members who want to understand their risks of developing certain cancers.
With the popularity of genetic testing for cancer increasing, a more common question many have is Does Medicare cover genetic testing for cancer?
In this article, we answer that question in clear, plain English. You will also find the average costs of genetic testing for cancer and other helpful info.
Read Also: How To Cure Breast Cancer With Baking Soda
Medicaid Disallows Payment For Outpatient And Inpatient On Same Date Of Service
Medicaid utilizes a Diagnosis Related Group payment methodology for services provided on an inpatient basis . The DRG facility payment is all inclusive and includes all services provided the patient during the inpatient stay. To enforce the policy, New York State Medicaid recently implemented a payment edit to reinforce billing policy that disallows payment for an outpatient visit concurrent with an inpatient stay.
The only exception to this policy is for emergency service procedures done in an Emergency Department. When emergency services are provided on the same date as the date of discharge and the primary diagnosis is different, the Emergency Department visit is Medicaid reimbursable.
Policy questions on this matter may be directed to the Division of Program Development and Management at 518-473-2160.
- Requiring > 21% oxygen use for =28 days post-birth or
- Infant with acyanotic heart disease receiving medication to control congestive heart failure and will require cardiac surgery or
- Infant with moderate to severe pulmonary hypertension or
- Potentially, infant with cyanotic heart disease, with consultation by cardiologist
The updated palivizumab ) worksheet provides instructions for completing the prior authorization process.
Multigene Panel Testing For Inherited Genetic Mutations
A multigene panel is a type of genetic test that looks for inherited mutations in more than one gene at the same time. It might include testing for BRCA1 and BRCA2 mutations in addition to mutations in other genes such as ATM, PALB2, CHEK2, etc. Medicare covers panel testing when:
- the patient has pretest genetic counseling with a genetics professional who does not work for a testing laboratory
- the patient has a post-test genetic counseling appointment with a genetics professional who does not work for a testing laboratory
- the patient has a cancer diagnosis and meets the BRCA testing criteria listed above and
- the genetic test will affect their cancer treatment options and
- all of the genes included in the test panel are relevant based on their personal and family history and
- the patient also meets criteria for at least ONE other hereditary cancer syndrome for which NCCN guidelines provide clear genetic testing criteria and management recommendations
Medicare coverage of multigene panel testing is available in all Medicare regions, although eligibility for this testing varies by Medicare Administrative Contractor . First Coast Service Options and Novitas Solutions MACs have more narrow testing policies. Broader coverage is available under Noridian Healthcare Solutions, Palmetto, Wisconsin Physicians Service Insurance, and CGS Administrators.
You May Like: Breast Cancer Symptoms Nausea
What Do I Need Post
There are several products you may want or need following your mastectomy. Not all items are covered by Medicare.
Post-Mastectomy Products Covered by Medicare
- Silicone breast prostheses
- Non-silicone breast prostheses
You must get a prescription or written order from your doctor before Medicare will cover these items.
Medicare doesnt specify a limit on the quantity of bras or camisoles it will cover. Instead, your doctor will determine what is reasonable and necessary on a case-by-case basis.
Mastectomy bras and camisoles are covered under Medicare Part B. You will owe 20 percent of the cost for each item.
Coverage And Utilization Of Services
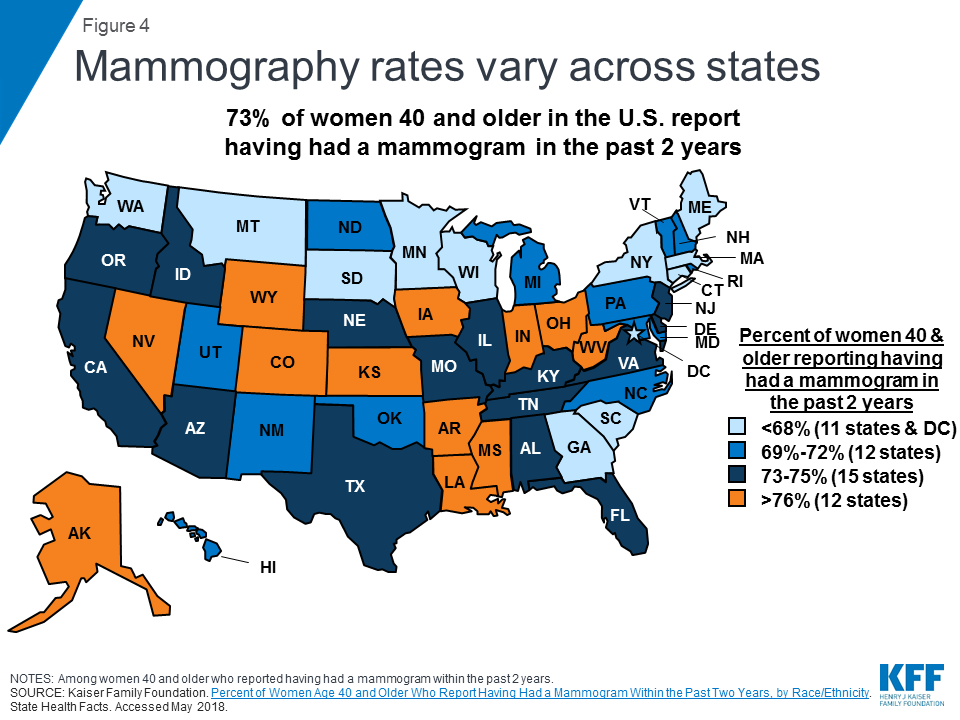
Most women with public and private insurance have coverage for breast cancer screening services, but the scope of coverage can differ based on the type of insurance plan, how they qualify for Medicaid, and in the case of Medicare, where they live. While there are programs to assist uninsured and underserved women, these programs only reach a fraction of eligible women.
You May Like: What Is Hr Positive Breast Cancer
Why Is Genomics Important
Genomics plays a role in 9 of the 10 leading causes of death,5 including:
- Heart disease
- Diabetes
- Alzheimers disease
Genetic tests for the leading causes of death and disability are becoming available. Family health history features prominently in a number of evidence-based recommendations. The U.S. Food and Drug Administration requires genetic testing to guide the use of many drugs. The Centers for Medicare and Medicaid Services provides coverage for certain genetic tests.6 As scientific evidence on the health benefits of available tests and interventions is strengthened, new evidence-based recommendations will emerge.
Evidence-based recommendations, like those from the USPSTF, can have an impact on access and use of genetic services. The proportion of women with a family health history of breast or ovarian cancer who received genetic counseling increased from 34.6% to 52.9% from 2005 to 2010.7 In addition, the Affordable Care Act covers genetic counseling as a preventive service with no out-of-pocket costs for women who have a family health history consistent with increased risk for BRCA mutations.8
Scamming In The Shadow Of A Major Military Outpost
The alleged cancer genetic testing fraud was not a centralized effort, but instead was spread across the United States and indictments were handed down for separate operations in multiple states.
The schemes varied by site, but generally involved inclusion of a physician or telemedicine company, as well as testing laboratories and some kind of Medicare beneficiary recruitment operation.
Medscape Medical News reviewed the indictment of two Texas physicians for insight into the alleged fraud.
In 2019, Sekhar Rao, MD, an interventional radiologist, and Vinay Parameswara, MD, an internist, both of Travis County, were charged with health care fraud and conspiracy to commit health care fraud. In exchange for kickbacks, the physicians “signed” cancer genetic screening test orders as well as toxicology tests for the ADAR Group, an outpatient toxicology testing laboratory in Killeen, near Fort Hood, a US Army installation. Both physicians allegedly provided ADAR Group with signature stamps that employees used to order the tests. False diagnostic codes such as “malignant neoplasm of the lip” were placed on claims in an attempt to gain acceptance and payment, according to the indictment.
Staff at ADAR Group allegedly enticed beneficiaries of Tricare, which is the military’s health plan and a federal program, with Walmart gift cards to provide urine and saliva specimens, and collected samples from as many as 200 beneficiaries a day.
Don’t Miss: Define Stage 3 Cancer
What Genetic Tests Are Covered By Medicare
Original Medicare typically does not cover preventative genetic tests.
Medicare Part B medical insurance may cover genetic testing in the following situations:
- You have signs or symptoms that may be able to be diagnosed with a genetic test
- Your metabolism of certain drugs needs to be assessed
- You have a personal history of breast cancer and meet other specific criteria
- You have a history of epithelial ovarian cancer, fallopian tube cancer or primary peritoneal cancer
Medicare Part B may also cover a screening test for colorectal cancer once every 3 years.
If your genetic test is not covered by Medicare, you may be responsible for 100 percent of the cost.
Does Insurance Cover Genetic Testing For Cancer
There are different ways that insurance covers genetic testing for cancer. First, determine with your healthcare provider which type of testing you should get, and then explore what is covered by your particular insurance plan.
Private Insurance Companies
Generally speaking, federal law and most state laws do not require private insurance companies to cover predictive testing, which can include BRCA testing insurance varies, however, as do the particular stipulations in each policy. For example, federal healthcare laws say that genetic testing should be covered for some women at higher risk of breast cancer.
Medicare
Does Medicare cover BRCA testing? There are limits to who is covered, but here is a list of some of the conditions that may allow you to access coverage:
- A breast cancer diagnosis at age 45 or earlier
- A close relative with a BRCA1 or BRCA2 gene mutation
- Ethnicity with a higher rate of BRCA mutation frequency, such as Ashkenazi Jewish
ClarityX can help you determine whether your insurance covers the genetic cancer screening you need.
Does Medicare cover genetic testing for cancer more broadly? Medicare also covers Lynch Syndrome testing in limited cases.
Read Also: Breast Cancer Stage 4 Life Expectancy
Breast Cancer Genetic Testing Cost
By Dr. Brandon Colby MD, a physician-expert in the fields of genetic testing and personalized preventive medicine.
Many people turn away from breast cancer genetic testing because of the cost. Despite the value of knowing whether someone has the BRCA1 or BRCA2, people feel the investment in the information is not worth the cost. They take a chance and decide to rely on early detection through breast self-exams and mammograms.
The only issue with this is those with a family history of the BRCA1 and BRCA2 gene mutations are missing out on the opportunity to decrease their cancer risk. By knowing whether someone has the BRCA1 or BRCA2 mutation, people can work with a genetic counselor and health care provider to reduce their chances of developing breast cancer.
Learn More: Breast Cancer Genetic Testing: Pros and Cons
Pharmacogenomics And Other Genetic Tests
Since 1998, Medicare has covered cytogenetic studies in specific situations.
Cytogenetics involves testing samples of tissue, blood or bone marrow in a lab to identify changes in chromosomes.
Medicare covers these tests when they are necessary for the diagnosis or treatment of certain kinds of leukemia and rare blood cancers.
Cytogenetic studies may also be covered when they are used to diagnose or treat genetic disorders in a fetus or failure of sexual development.
Also Check: Treatment For Stage Iv Breast Cancer
Who Should Have Genetic Testing
Genetic testing isnt something that everyone needs or should have. In general, this type of testing is aimed at individuals with a particular family or personal history of cancer. This is why, in addition to finding out is genetic testing for cancer covered by insurance, you should discuss with your doctor whether you are a good candidate for these exams.
New York State Medicaid Management Information System Update Provider Training Opportunities
The New York State Department of Health and Xerox Healthcare, LLC, are pleased to announce that training opportunities are now available for the new New York State Medicaid Management Information System – NYMMIS.
The interim website, www.interimnymmis.com is the source for the most current information on NYMMIS. The current schedule of training sessions is available under the Training and Events Calendar link on the website.
As previously advised in the August 2015 Medicaid Update, training includes a variety of in-person and web- based learning sessions, with the in-person sessions offered in several regional locations. In addition, training opportunities will be available in a variety of methods including self-taught computer based training and on-site provider training by field representatives from Xerox. The Training and Events Calendar will be updated as additional sessions are scheduled.
Current Training Session Descriptions:
The Training and Events Calendar will display a complete list of all training dates, times, and locations. All efforts are being taken to develop the trainings in a manner that will maximize learning and minimize impact to the provider.
To sign up for training on the new system, please send registration requests via email to with the following information: attendee name, organization, email address, phone number, requested date, time, and location. Classroom sizes are limited and will be confirmed on a first come, first served basis.
Recommended Reading: Lymphatic Cancer Stage 3
Does Medicaid Cover Genetic Testing
- Does Medicaid cover genetic testing? Learn more about tests available and when testing is covered, including Medicaid coverage for children and pregnant women.
Genetic testing can be a powerful tool for health care providers. Its used to confirm diagnoses, identify the possibility of future illness, detect if someone carries a gene that they may pass on and predict a response to therapy. If a condition is identified through genetic testing, doctors may be able to intervene early to reduce severity or prevent the condition developing altogether. However, the costs involved may be daunting, so its important to know whether Medicaid covers genetic testing.
Does Insurance Cover Brca Testing
In the United States, BRCA testing is usually covered by insurance if the patient meets certain criteria. Insurance coverage and criteria varies by insurance plan, and genetic counselors will review potential costs and insurance coverage with you during your appointment.
Some insurance companies have specific testing criteria or do not cover testing in certain situations, even when it is considered medically appropriate. For example, Medicare has specific BRCA testing criteria that only includes individuals with a personal history of cancer. Therefore, Medicare does not cover someone with a known mutation in the family who has no personal history of cancer. Medicaid coverage typically varies by state.
Also Check: Chances Of Breast Cancer Returning
Is Genetic Testing For Cancer Covered By Insurance
Many people find themselves asking, Is genetic testing for cancer covered by insurance? Unfortunately, the answer isnt always straightforward.If you know some basic information, you can pursue some testing such as BRCA testing . This kind of testing can help you estimate your chances of developing cancer, and it is available for specific types of cancer. It can be an invaluable resource regarding healthcare planning with your doctor.
Beware Of Medicare Genetic Testing Scams

Cases of scammers offering free genetic testing services to Medicare beneficiaries has been on the rise in recent years.
According to the U.S. Administration for Community Living, unscrupulous people will often target Medicare enrollees via telemarketing calls, booths at public events and door-to-door visits offering free genetic tests.
They often claim that the testing is covered by Medicare and free of charge to the beneficiary.
If a company bills Medicare for genetic testing, and Medicare denies the claim, the beneficiary could be responsible for the entire cost of the test which often totals around $10,000, Rebecca Kinney, acting director of the Office of Healthcare Information and Counseling, wrote in a government news release.
In September 2019, the Justice Department took down a massive fraud scheme involving genetic cancer testing. Thirty-five people were charged for unlawfully billing Medicare more than $2.1 billion.
The DOJ said recruiters or marketers often approached seniors at health fairs or during door-to-door visits. They would obtain the beneficiarys Medicare information for identity theft or fraudulent billing purposes.
The recruiter would then get a doctor to sign off on the genetic test so it could be processed by a lab.
The doctors received a kickback in exchange for ordering the test. After the lab was reimbursed for the test by Medicare, the lab shared proceeds of that payment with the recruiter.
Read Also: Can Cancer Come Back In The Same Breast