Clinical Considerations And Recommendations
How should individual breast cancer risk be assessed?
Health care providers periodically should assess breast cancer risk by reviewing the patients history. Breast cancer risk assessment is based on a combination of the various factors that can affect risk Box 1610111213. Initial assessment should elicit information about reproductive risk factors, results of prior biopsies, ionizing radiation exposure, and family history of cancer. Health care providers should identify cases of breast, ovarian, colon, prostate, pancreatic, and other types of germline mutation-associated cancer in first-degree, second-degree, and possibly third-degree relatives as well as the age of diagnosis. Women with a potentially increased risk of breast cancer based on initial history should have further risk assessment. Assessments can be conducted with one of the validated assessment tools available online, such as the Gail, BRCAPRO, Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm, International Breast Cancer Intervention Studies , or the Claus model 34.
Is screening breast self-examination recommended in women at average risk of breast cancer, and what should women do if they notice a change in one of their breasts?
Should practitioners perform routine screening clinical breast examinations in average-risk women?
When should screening mammography begin in average-risk women?
How frequently should screening mammography be performed in average-risk women?
Symptoms Of Angiosarcoma Of The Breast
Another rare form of breast cancer, angiosarcoma forms inside the lymph and blood vessels. Only a biopsy may definitively diagnose this type of cancer. Angiosarcoma can cause changes to the skin of your breast, such as the development of purple-colored nodules that resemble a bruise. These nodules, if bumped or scratched, may bleed. Over time, these discolored areas may expand, making your skin appear swollen in that area. You may or may not have breast lumps with angiosarcoma. If you also have lymphedema, which is swelling caused by a buildup of lymphatic fluid, angiosarcoma may occur in the affected arm. Cancer treatment sometimes damages the lymph vessels, which may lead to lymphedema.
Malignant And Benign Tumors On Mri Scan
During the MRI scan, a malignant lesion will tend to demonstrate a rapid increase in signal intensity after the contrast injection. This intensity is often followed by a wash-out of contrast on images which appear in the minutes that follow.
Benign lesions, on the other hand, tend to exhibit a slow, progressive rise in intensity of the signal with no wash-out of contrast. Radiologists classify the contrast enhanced lesion according to the morphology of the contrast, and also by the kinetics or changes in time of the contrast enhancing areas.
In addition, please note that MRI scan improves contrast and definition and not just cancer. MRI scan also improves definition in non-cancerous and pre-cancerous conditions, such as:-
Read Also: Nipple Piercing And Breast Cancer
Stage Of Breast Cancer
When breast cancer is diagnosed, your doctors will give it a stage. The stage describes the size of the cancer and how far it has spread, and is used to predict the outlook.
Ductal carcinoma in situ is sometimes described as stage 0. Other stages of breast cancer describe invasive breast cancer and include:
- stage 1 the tumour measures less than 2cm and the lymph nodes in the armpit are not affected. There are no signs that the cancer has spread elsewhere in the body
- stage 2 the tumour measures 2 to 5cm, the lymph nodes in the armpit are affected, or both. There are no signs that the cancer has spread elsewhere in the body
- stage 3 the tumour measures 2 to 5cm and may be attached to structures in the breast, such as skin or surrounding tissues, and the lymph nodes in the armpit are affected. There are no signs that the cancer has spread elsewhere in the body
- stage 4 the tumour is of any size and the cancer has spread to other parts of the body
This is a simplified guide. Each stage is divided into further categories: A, B and C. If you’re not sure what stage you have, talk to your doctor.
Imaging Tests To Look For Breast Cancer Spread
If you have been diagnosed with breast cancer, you might need more imaging tests. Your doctor will talk with you about which of these tests you may need.
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. Imaging tests might be done for a number of reasons including:
- To look at suspicious areas that might be cancer
- To learn how far cancer might have spread
- To help determine if treatment is working
- To look for possible signs of cancer coming back after treatment
Don’t Miss: Did Anne Hathaway Have Breast Cancer
How To Calculate Breast Cancer Risk Factors
We all know that breast cancer kills our mothers, sisters and daughters. But unfortunately the exact causes of breast cancer have not been determined till now. Health experts have found very few or rare reasons that may cause this killer disease, but theses are not exact reasons.
So far we have informed that pressing, massaging or touching breasts never may be the reasons or carriers of breast cancer and this is not a contagious disease. There is no chance if you get contact with any victim of this disease.
But researchers have found some reasons or factors that may create situations for developing breast cancer. These factors are identified as the risk factors for breast cancer. And the chance of breast cancer attack is increased by these risk factors.
We are now going to discuss the risk factors in brief in this article and this may help us in preventing breast cancer.
The older you grow, the more the chance of breast cancer increases. Maximum patients were detected among the women of age group 50 to 60 years.
More Information About The Tnm Staging System
The T category describes the original tumor:
- TX means the tumor can’t be assessed.
- T0 means there isn’t any evidence of the primary tumor.
- Tis means the cancer is “in situ” .
- T1, T2, T3, T4: These numbers are based on the size of the tumor and the extent to which it has grown into neighboring breast tissue. The higher the T number, the larger the tumor and/or the more it may have grown into the breast tissue.
The N category describes whether or not the cancer has reached nearby lymph nodes:
- NX means the nearby lymph nodes can’t be assessed, for example, if they were previously removed.
- N0 means nearby lymph nodes do not contain cancer.
- N1, N2, N3: These numbers are based on the number of lymph nodes involved and how much cancer is found in them. The higher the N number, the greater the extent of the lymph node involvement.
The M category tells whether or not there is evidence that the cancer has traveled to other parts of the body:
- MX means metastasis can’t be assessed.
- M0 means there is no distant metastasis.
- M1 means that distant metastasis is present.
Also Check: Stage 3a Cancer
How Does The Test Work
The testing lab typically uses a specialized staining process on the breast tissue sample to see if hormone receptors are present. The technical name for this procedure is an immunohistochemical staining assay or an ImmunoHistoChemistry . Findings will be included in a pathology report given to your doctor. If the cancer is deemed estrogen-receptor-positive , its cells have receptors for the estrogen hormone. That means that the cancer cells likely receive signals from estrogen to promote growth. About two out of every three breast cancers contain hormone receptors.
If the cancer is progesterone-receptor-positive , its cells have receptors for progesterone. This hormone could then promote the growth of the cancer.
The cancer cells being estrogen and/or progesterone receptor-positive is a good prognostic factor to have, usually leading to a better prognosis.
When You Need Themand When You Dont
When you learn that you have breast cancer, its normal to want to do everything you can to treat it and be sure it doesnt come back. But its not always a good idea to get all the tests that are available. You may not need them. And the risks may be greater than the benefits.
The information below explains when cancer experts recommend imaging tests and tumor marker testsand when they dont.
Imaging tests, such as CT, PET, and bone scans, take pictures to help find out if the cancer has spread in your body. Another test, called a tumor marker test, is a kind of blood test. Tumor markers are also called biomarkers or serum markers. They are higher than normal in some cancer patients. The tests you need depends on the stage of your breast cancer.
Read Also: Stage Three Breast Cancer
Who Gets Breast Cancer
Breast cancer is the most common cancer among women other than skin cancer. Increasing age is the most common risk factor for developing breast cancer, with 66% of breast cancer patients being diagnosed after the age of 55.
In the US, breast cancer is the second-leading cause of cancer death in women after lung cancer, and it’s the leading cause of cancer death among women ages 35 to 54. Only 5 to 10% of breast cancers occur in women with a clearly defined genetic predisposition for the disease. The majority of breast cancer cases are “sporadic, meaning there is no definitive gene mutation.
What Is Breast Cancer Staging
To determine the stage of your cancer, doctors look at how large your tumor is, where it is, and if it has spread. They also look at your medical history, physical exams, diagnostic tests, and tests of your tumor and lymph nodes.
- Early-stage breast cancer includes stages 0, I, II and IIIA .
- In stage 0, there are abnormal cells in the ducts or lobes of the breast. They have not broken through the wall of the duct or spread.
- In stages I, II, and IIIA, there is a tumor. It may have spread to lymph nodes under the arm, but it has not spread anywhere else.
Also Check: Estrogen Positive Breast Cancer Survival
What If You Have Early
If you have early-stage breast cancer but no symptoms to suggest the cancer has spread, you should not get an imaging test to look for cancer in other places in your body. The chance that your cancer has spread is very small. Studies show that breast cancer spreads to the liver and bones in fewer than 6 out of 100 people. And this is usually in patients with stage III breast cancer.
Common Q& as On Mri Scan And Malignancy Detection

When would a patient have an MRI scan ?
a patient would have an MRI scan after a biopsy that is positive for cancer, and your doctor needs more information about the extent of the disease.
In certain situations, such as for women with high risk of breast cancer, breast MRI may be useful with mammograms as a screening tool for detecting breast cancer.
Why is MRI done?
Breast MRI is most often used to screen for breast cancer in women thought to have a high risk of the disease. Your doctor may recommend a breast MRI scan if you have a diagnosis of breast cancer to determine the extent of the cancer.
MRI scans are also useful if you have a:-
- leak or rupture of a breast implant
- high risk of breast cancer
- strong family history of breast cancer
- very dense breast tissue and mammogram didnt detect a prior breast cancer
- history of precancerous breast changes such as atypical hyperplasia or lobular carcinoma in situ
- strong family history of breast cancer and dense breast tissue
What does an MRI Scan show?
Like CT scans, MRI creates cross-section pictures of your insides. But MRI uses strong magnets, instead of radiation, to make the images.
An MRI scan can take cross sectional views from many angles, as if someone were looking at a slice of your body from the front, from the side, or from above your head.
MRI creates pictures of soft tissue parts of the body that are sometimes hard to see using other imaging tests. MRI is very good at finding and pinpointing some cancers.
Also Check: 3a Breast Cancer
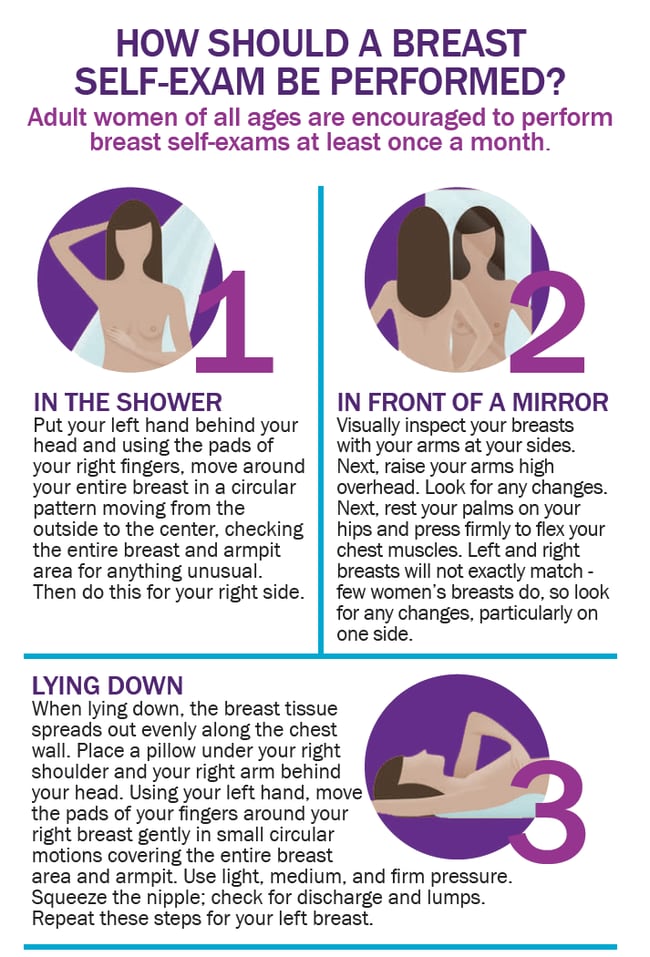
How To Make Breast Self
Make it routine. The more you examine your breasts, the more you will learn about them and the easier it will become for you to tell if something has changed. Try to get in the habit of doing a breast self-examination once a month to familiarize yourself with how your breasts normally look and feel. Examine yourself several days after your period ends, when your breasts are least likely to be swollen and tender. If you are no longer having periods, choose a day that’s easy to remember, such as the first or last day of the month.
Get to know your breasts’ different neighborhoods. The upper, outer area near your armpit tends to have the most prominent lumps and bumps. The lower half of your breast can feel like a sandy or pebbly beach. The area under the nipple can feel like a collection of large grains. Another part might feel like a lumpy bowl of oatmeal.
Start a journal where you record the findings of your breast self-exams. This can be like a small map of your breasts, with notes about where you feel lumps or irregularities. Especially in the beginning, this may help you remember, from month to month, what is normal for your breasts. It is not unusual for lumps to appear at certain times of the month, but then disappear, as your body changes with the menstrual cycle .
Learn more about Breastcancer.org’s recommendations on when to begin annual mammograms.
N Categories For Breast Cancer
N followed by a number from 0 to 3 indicates whether the cancer has spread to lymph nodes near the breast and, if so, how many lymph nodes are involved.
Lymph node staging for breast cancer is based on how the nodes look under the microscope, and has changed as technology has gotten better. Newer methods have made it possible to find smaller and smaller groups of cancer cells, but experts haven’t been sure how much these tiny deposits of cancer cells influence outlook.
Its not yet clear how much cancer in the lymph node is needed to see a change in outlook or treatment. This is still being studied, but for now, a deposit of cancer cells must contain at least 200 cells or be at least 0.2 mm across for it to change the N stage. An area of cancer spread that is smaller than 0.2 mm doesn’t change the stage, but is recorded with abbreviations that indicate the type of special test used to find the spread.
If the area of cancer spread is at least 0.2 mm , but still not larger than 2 mm, it is called a micrometastasis . Micrometastases are counted only if there aren’t any larger areas of cancer spread. Areas of cancer spread larger than 2 mm are known to influence outlook and do change the N stage. These larger areas are sometimes called macrometastases, but are more often just called metastases.
NX: Nearby lymph nodes cannot be assessed .
N0: Cancer has not spread to nearby lymph nodes.
N1c: Both N1a and N1b apply.
N3: Any of the following:
N3a: either:
N3b: either:
Also Check: Breast Cancer Prognosis Stage 3
What Happens After The Local Breast Cancer Treatment
Following local breast cancer treatment, the treatment team will determine the likelihood that the cancer will recur outside the breast. This team usually includes a medical oncologist, a specialist trained in using medicines to treat breast cancer. The medical oncologist, who works with the surgeon, may advise the use of the drugs like tamoxifen or anastrozole or possibly chemotherapy. These treatments are used in addition to, but not in place of, local breast cancer treatment with surgery and/or radiation therapy.
After treatment for breast cancer, it is especially important for a woman to continue to do a monthly breast examination. Regular examinations will help you detect local recurrences. Early signs of recurrence can be noted in the incision area itself, the opposite breast, the axilla , or supraclavicular region .
Maintaining your follow-up schedule with your physician is also necessary so problems can be detected when treatment can be most effective. Your health care provider will also be able to answer any questions you may have about breast self-examination after the following procedures.
Blood Testing For Her2/neu
Sometimes, especially when there is not enough tumor tissue available to perform the test, a blood sample is drawn from the patients arm to collect similar data. This blood test is called a serum HER2/neu test, and it can be used as part of the initial workup upon cancer diagnosis or to monitor the effectiveness of treatment. If initially the level of serum HER2/neu is elevated to more than 15ng/mL and then it falls, the treatment is likely working. However, if the serum level remains elevated, this indicates the treatment is not working. If the serum level declines but then, upon later testing, is elevated once again, this is a sign that the cancer could be recurring.
When all three of the tests come back negative for receptors for hormones and negative for HER2, triple negative breast cancer may be the diagnosis.
Materials on this page courtesy of:
Read Also: Invasive Breast Cancer Meaning
How Do I Know My Risk For Breast Cancer Recurrence
After completing treatment for breast cancer, many patients may focus on their risk of recurrence. While this risk is individualized, there are certain factors your doctor may consider to determine whether you are at a higher or lower risk for the cancer returning.
Each persons breast cancer diagnosis is different, and includes unique factors that affect risk, says Erica Mayer, MD, MPH, a breast oncologist in the Susan F. Smith Center for Womens Cancers at Dana-Farber. Therapies recommended for each patient can be quite different and individualized.