Questions For Your Breast Surgeon:
- Am I a candidate for a sentinel lymph node biopsy?
- If I have a positive node how will that change my treatment plan?
- Under what situations might I need an axillary dissection?
- What will you do if you find one or two nodes with cancer?
- What are the side effects of the biopsy?
- Can I avoid lymph node surgery altogether?
Sensitivity And False Negatives Of Cancer Metastisis
As mentioned, the average sensitivity of the SLN biopsy is about 90% with a false negative rate of about 10%. A positive lymph nodes result means that malignant cancer cells have metastized beyond the original cancer site to some of the sentinel lymph nodes. Negative, means that the sentinel lymph nodes are clear. False negatives are generally the result ofa) not finding a sentinel lymph node orb) the absence of a sentinel lymph node,c) metastasis of the primary tumor to some area besides the axillary region, ord) because the lymphatic channels have already been corrupted by the tumor cells, and/or tumor metastasis to axillary lymph nodes has already occurred.
In older patients, a false negative assessment might also be attributed to an excessive amount of fatty tissue within the lymphatic channels which impairs the absorption of the investigative fluids.
A Swollen Arm Or Hand
You are at risk of long term swelling in your hand and arm after surgery to remove your lymph nodes in the armpit. This is swelling caused by lymph fluid that can’t drain away. It can happen any time after surgery and radiotherapy to your armpit.
Not everyone will get this and it is less likely to happen if you only have a few nodes removed. But it is very important to speak to your specialist nurse or surgeon if you think your arm or hand may be swollen.
Unfortunately, once you have lymphoedema it cant be cured. But early treatment can help to control it. Your nurse will talk to you about ways of preventing lymphoedema.
Don’t Miss: Carcinoma Left Breast
Are There Any Risks To The Test
You may have a little bleeding, pain, or bruising at the biopsy site. There is also a small risk of infection, which can be treated with antibiotics. Allergic reactions to the tracer are rare and usually mild.
There is very little exposure to radiation in a sentinel lymph node biopsy. While radiation exposure from the tracer in a sentinel lymph node biopsy is safe for most adults, it can be harmful to an unborn baby. So be sure to tell your provider if you are pregnant or think you may be pregnant.
Significance Of Regional Nodal Involvement In Breast Cancer
The significance of tumor lymphatics and their role in tumor progression is debated. Whether the presence of tumor cells in regional nodes is merely a sign of regional progression or an indicator of systemic dissemination of disease is yet to be settled . However, axillary nodal involvement is already established as an indicator of poor prognosis, with the 5-year survival decreasing by approximately 28% to 40% in patients with such a condition . Thus, axillary surgery not only serves as a staging tool but also improves locoregional control, which may result to improved survival.
Read Also: Chemotherapy Cycles For Breast Cancer
Lymph Node Surgery For Breast Cancer
If breast cancer spreads, it typically goes first to nearby lymph nodes under the arm. It can also sometimes spread to lymph nodes near the collarbone or near the breastbone . Knowing if the cancer has spread to your lymph nodes helps doctors find the best way to treat your cancer.
If you have been diagnosed with breast cancer, its important to find out how far the cancer has spread. To help find out if the cancer has spread outside the breast, one or more of the lymph nodes under the arm are removed and checked in the lab. This is an important part of staging. If the lymph nodes have cancer cells, there is a higher chance that cancer cells have also spread to other parts of the body. More imaging tests might be done if this is the case.
Lymph node removal can be done in different ways, depending on whether any lymph nodes are enlarged, how big the breast tumor is, and other factors.
Negative Sentinel Node Biopsy Usually Means All Axillary Lymph Nodes In The Breast Are Cancer Free
The main advantage of the sentinel node biopsy is that a negative result will, in most cases, spare the breast cancer patient the ordeal of axillary node biopsies and dissections.
In fact, the SLN biopsy is so accurate the current debate is whether or not axillary dissections are necessary at all.
A positive sentinel node biopsy finding, means that malignant cells are present in the sentinel lymph node. Sometimes, the sentinel lymph is mysteriously absent.
Positive sentinel nodes would warrant an immediate follow-up with a thorough axillary node assessment. But, sentinel lymph node biopsies, when negative, indicate that the axillary nodes are cancer free. So, medics consider a negative sentinel node biopsy result to be about 95% accurate.
However, a negative sentinel node result can cause a great deal of anxiety. This is because there may be discussion and consultation between the breast cancer patient and the treatment team as to whether or not the sentinel lymph node biopsy is good enough.
You May Like: Stage 3 Invasive Ductal Carcinoma
So You Have A Positive Sln Then What
Sentinel lymph node biopsies are very accurate and reliable when they are negative for tumor cells. But if there is a positive result there is still a lack of clarity regarding the prognostic indications. If the sentinel lymph node is tumor-positive , it does not necessarily mean that the cancer will metastasise to the other non-sentinel lymph nodes.
Sometimes the biopsy results show a mix of negative and positive nodes. In this case the risk of spread to the axillary lymph nodes is still quite low, at around 10%. A CLND may not always be necessary.
Other factors that tend to suggest an increase in the probability of involvement of the other lymph nodes include the:-
- size of the lesion on the affected sentinel node
- size of the primary tumor
- presence or absence of lymphovascular invasion in the primary tumor
- amount of lymph node removal.
Are There Any Side Effects From The Biopsy
Since lymph vessels are cut during the biopsy, lymph fluid can sometimes accumulate in that area, causing a seroma . Any time lymph nodes are removed from the axilla there is also a risk of lymphedema. This can be an ongoing problem, but physical therapy and other treatments can help. Patients may also experience loss of sensation and decreased range of motion in the area.
Read Also: Estrogen Receptive Breast Cancer Prognosis
What If My Report Mentions Her2/neu Or Her2
Some breast cancers have too much of a growth-promoting protein called HER2/neu . The HER2/neu gene instructs the cells to make this protein. Tumors with increased levels of HER2/neu are referred to as HER2-positive.
The cells in HER2-positive breast cancers have too many copies of the HER2/neu gene, resulting in greater than normal amounts of the HER2 protein. These cancers tend to grow and spread more quickly than other breast cancers.
All newly diagnosed breast cancers should be tested for HER2, because women with HER2-positive cancers are much more likely to benefit from treatment with drugs that target the HER2 protein, such as trastuzumab , lapatinib , pertuzumab , and T-DM1 .
Testing of the biopsy or surgery sample is usually done in 1 of 2 ways:
- Immunohistochemistry : In this test, special antibodies that will stick to the HER2 protein are applied to the sample, which cause cells to change color if many copies are present. This color change can be seen under a microscope. The test results are reported as 0, 1+, 2+, or 3+.
- Fluorescent in situ hybridization : This test uses fluorescent pieces of DNA that specifically stick to copies of the HER2/neu gene in cells, which can then be counted under a special microscope.
Many breast cancer specialists think that the FISH test is more accurate than IHC. However, it is more expensive and takes longer to get the results. Often the IHC test is used first:
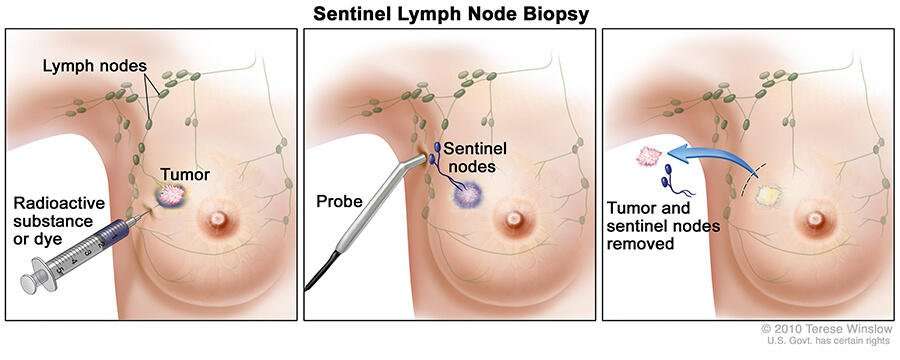
What Does Sentinel Mean
Sentinel refers to an age-old military practice of posting a guard far away from the home-base. The guard is a lookout for early detection of an approaching enemy.
Here is a sentinel tower that gives some protection to the poor soldier.
Similarly, the first lymph node to encounter cancer cells , is the sentinel lymph node.
In a sentinel node biopsy, surgeons remove only this initial lymph node, the sentinel lymph node. Radiographers identify the sentinel lymph node with a dye. This dye is either a weak radioactive dye or a blue dye that stains the lymph tissue a bright blue color.
This page is still fantastic for research. However, we have a new page with more up-to-date information on sentinel lymph node biopsies. Check it out!
Don’t Miss: Is Stage 3 Breast Cancer Terminal
Meaning Of The Presence Of Tumor In The Sentinel Lymph Node
The presence of tumor in the sentinel lymph node must be considered according to different stages. In case of:
Macro metastases : There is a high risk of axillary residual disease .
Micro metastases : There is an axillary residual disease in 10% of patients.
Isolated tumor cells : Rarely associated with an axillary residual disease and have no proven prognostic significance.
These slides show how difficult and random it is to carry out in both cases an examination during surgery.
This is why an immuno-histochemical analysis makes the diagnosis more reliable. Thus, it will be the final analysis of the node that will allow a finer diagnosis and the discovery of isolated tumor cells. While this result may not affect future treatment, it has the advantage of avoiding diagnostic errors.
What Does It Mean If My Carcinoma Is Called Invasive Ductal Carcinoma Invasive Lobular Carcinoma Or Carcinoma With Ductal And Lobular Features
Breast carcinomas are often divided into 2 main types: invasive ductal carcinoma and invasive lobular carcinoma, based on how they look under the microscope. In some cases, the tumor can have features of both and is called a mixed ductal and lobular carcinoma. Another term for invasive ductal carcinoma is invasive mammary carcinoma of no special type, because it is the most common type of breast carcinoma.
Both invasive ductal carcinomas and invasive lobular carcinomas arise from the cells lining the ducts and lobules in the breast. In general, invasive lobular and invasive ductal carcinomas of the breast arent treated differently.
Don’t Miss: Breast Cancer Secondary Cancer
The Pathologist Looks For Radioactive Hot Spots In The Sentinel Node
It will take at least 40-60 minutes for the re-injected technetium sulphur colloid to migrate to the sentinel lymph nodes. Some protocols even recommend up to 4 hours between injection and subsequent mapping. The blue dye however, is very rapidly taken up by the lymphatic system and must be injected less than 10 minutes before the anticipated surgical extraction.
Tumors are typically hard, and are difficult to inject into. If one attempted to inject inside the tumor, most of it would leak out along the needle track, into a peritumoral location anyway. Because of this, injection sites will typically either be intra or peritumoral, subdermal above the tumor , or given in the subareolar region .
The practice of using these procedures to locate the sentinel lymph node and to trace the movement of lymphatic flow, is called lymphoscintigraphy.
Types Of Lymph Node Surgery
Even if the nearby lymph nodes are not enlarged, they will still need to be checked for cancer. This can be done in two different ways. Sentinel lymph node biopsy is the most common way and only a few lymph nodes are removed. But in some cases, an axillary lymph node dissection , which removes more lymph nodes, might be needed.
Lymph node surgery is often done as part of the main surgery to remove the breast cancer, but sometimes it might be done as a separate operation.
Recommended Reading: Non Hormonal Breast Cancer
Slnb In Clinically Positive Axilla
The status of SLNB in patients with cN+ axilla who achieve complete clinical response after NACT is controversial. Initial studies evaluating SLNB in this setting have revealed high FNR of > 25% . In a large retrospective study, the identification rate of SLN after NACT was significantly low , although FNR was comparable to upfront approach . A recent meta-analysis of 1,395 patients with cN1 axillary disease reported an SLN identification rate after NACT of 92.3% and FNR of 15.1% . Further, this meta-analysis showed lower SLN identification rate with the use of blue dye alone than radiotracer or a combination of these techniques.
Three recent prospective observational studies, namely, ACOSOG Z1071, SENTINA, and SN FNAC, have provided additional insights in this subject . These three studies had slightly different designs, but all of them evaluated SLNB in patients with cN+ axilla who achieved ycN0 status after NACT . The following conclusions can be drawn from these studies to optimize SLNB after NACT: use of dual tracer lymphatic mapping identification and retrieval of > 2 SLNs use of IHC for disease detection in SLNs and performance of completion ALND in patients with pN disease.
Is Sentinel Node Biopsy Always Accurate
In a small number of women, the sentinel node doesnt have cancer cells, even though there are cancer cells in other lymph nodes in the armpit. This is called a false-negative result.
A false-negative result sometimes occurs because lymphatic vessels running to the lymph nodes that have cancer cells in them are blocked by cancer cells. This means that the dye goes into other normal lymph nodes instead.
To minimise the chance of a false-negative result, the surgeon may remove any enlarged nodes that are found at the time of surgery, even if they do not contain the dye.
Don’t Miss: How Fast Does Breast Cancer Grow
Discussion And Literature Review
Knowledge of sentinel lymph node status remains the most powerful prognostic factor in defining the adjuvant strategy of the majority of solid tumors .
The difficulty of the methods described demonstrates the necessity of having an experienced pathologist to evaluate extemporaneously micro metastases or isolated metastasis cells. As proposed by the American Society of Breast Surgeons, accreditation should be given to surgeons practicing sentinel node examination in breast cancer after teaching and evaluating their technique.
The axillary dissection gives only a prognostic indication . The tumors being diagnosed smaller and smaller, the technique of the GS has taken its place. The adjuvant therapeutic strategies depend on its results.
Indeed, the presence of isolated tumor cells has no predictive value for residual axillary disease. No pejorative prognostic value either the presence of micro metastases is associated in 1012% of cases with residual axillary disease. No significant prognostic difference in terms of overall survival and survival without recurrence . Therefore no complementary axillary clearing is use full .
In the literature, it is interesting to note that no per– unsure of meaning of per operative examination has been carried out to date.
What If My Report Mentions Lymph Nodes
If breast cancer spreads, it often goes first to the nearby lymph nodes under the arm . If any of your underarm lymph nodes were enlarged , they may be biopsied at the same time as your breast tumor. One way to do this is by using a needle to get a sample of cells from the lymph node. The cells will be checked to see if they contain cancer and if so, whether the cancer is ductal or lobular carcinoma.
In surgery meant to treat breast cancer, lymph nodes under the arm may be removed. These lymph nodes will be examined under the microscope to see if they contain cancer cells. The results might be reported as the number of lymph nodes removed and how many of them contained cancer .
Lymph node spread affects staging and prognosis . Your doctor can talk to you about what these results mean to you.
Don’t Miss: Stage 1 Breast Cancer Prognosis
Technical Consider Another Word Choice Like Technique Or Method
Histologically, it is necessary to cut the lymph node every 2 mm and examine all sections extemporaneously. Particular attention must be paid to avoid using all material and allow for proper standard histological examination after fixation.
It is also necessary carrying out cytological fingerprints.
Checking Lymph Nodes During Surgery

The sentinel node is the first node that fluid drains to from the breast into the armpit. This means its the first lymph node the breast cancer could spread to.
Your surgeon usually carries out a sentinel lymph node biopsy during the operation to remove your breast cancer. You have about 1 to 3 nodes removed to see if they contain cancer cells.
Also Check: Is Stage 3a Breast Cancer Curable
Findings From A Sentinel Node Biopsy
- Lymph node-negative. None of the sentinel nodes contain cancer. So, its unlikely other lymph nodes have cancer. Surgery to remove more lymph nodes wont be needed.
- Lymph node-positive. At least one sentinel node contains cancer. More lymph nodes may be removed with a procedure called axillary dissection. The goals of axillary dissection are to check how many lymph nodes have cancer and to reduce the chances of cancer returning in the lymph nodes.
The Sentinel Lymph Node In Breast Cancer: Problems Posed By Examination During Surgery A Review Of Current Literature And Management
- 1Department of Gynecology Obstetrics, Cantonal Hospital, HFR, Fribourg, Switzerland
- 2Argotlab and Synlab Laboratories, Department of Pathology, Lausanne, Switzerland
The presence of tumor cells can be identified in the lymph node when metastasis has occurred from the primary cancer site into the lymph node If the sentinel lymph node ganglion is negative for the presence of tumor cells at the time of histological examination, the other lymph nodes are also negative in 99% of cases. If no tumor cells are identified in the sentinel lymph node ganglion by histological examination, the other lymph nodes are also negative for the presence of tumor cells in 99% of cases. The sentinel lymph node advantageously replaces axillary dissection as a staging method in breast cancer T1 and T2 . Approximately 40% of breast cancers metastasize to axillary lymph nodes and metastatic extension depends on disease stage. Sentinel lymph nodes are affected in the following stages: T1a , T1b , T1c , T2 , T3 .
Don’t Miss: Stage 3a Breast Cancer Survival