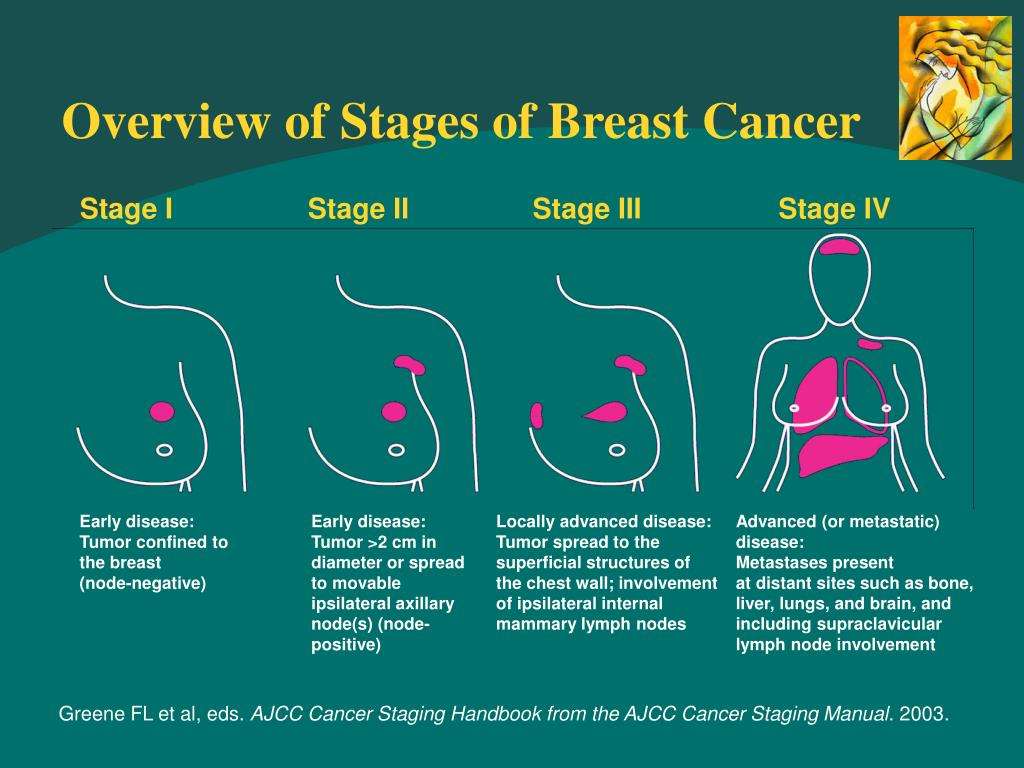
Stage 4 Breast Cancer
Stage 4 breast cancer is also known as secondary breast cancer.
Stage 4 breast cancer means:
- The tumour can be any size
- The lymph nodes may or may not contain cancer cells
- The cancer has spread to other parts of the body such as the bones, lungs, liver or brain
If your cancer is found in the lymph nodes under the arm but nowhere else in the body you do not have stage 4 breast cancer.
Donât Miss: Chemotherapy For Breast Cancer Stage 3
Pagets Disease Of The Nipple
This is a rare form of breast cancer that affects the nipple and the area around the nipple . Many people with Pagets disease also have breast cancer in other parts of the breast. The main signs of Pagets disease is a change in the nipple and/or areola area of the breast including the area becoming hard, lumpy or crusty redness, discharge or bleeding from the nipple and appearance of a lump.
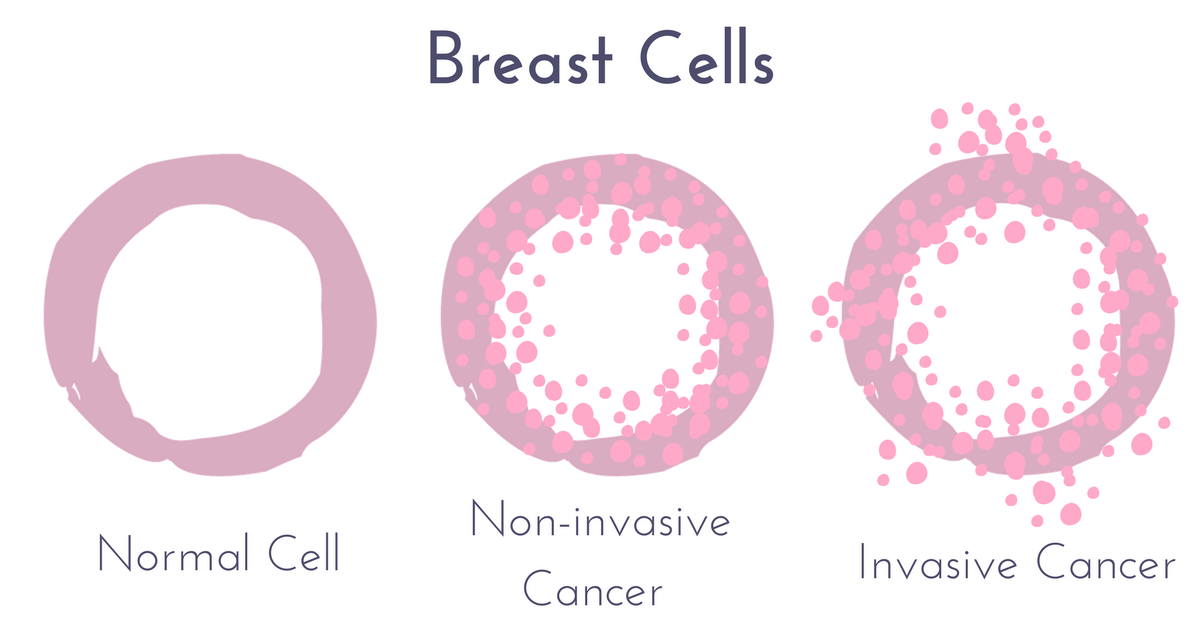
Ductal Carcinoma In Situ
DCIS is the most common type of noninvasive breast cancer, with about 60,000 new cases diagnosed in the United States each year. About one in every five new breast cancer cases is ductal carcinoma in situ.
Also called intraductal carcinoma or stage 0 breast cancer, its considered a noninvasive breast cancer. With DCIS, abnormal and cancerous cells havent spread from the ducts into nearby breast tissue nor anywhere else, such as the lymph nodes.
DCIS is divided into several subtypes, mainly according to the appearance of the tumor. These subtypes include micropapillary, papillary, solid, cribriform and comedo.
Patients with ductal carcinoma in situ are typically at higher risk for seeing their cancer return after treatment, although the chance of a recurrence is less than 30 percent. Most recurrences occur within five to 10 years after the initial diagnosis and may be invasive or noninvasive. DCIS also carries a heightened risk for developing a new breast cancer in the other breast. A recurrence of ductal carcinoma in situ would require additional treatment.
The type of therapy selected may affect the likelihood of recurrence. Treating DCIS with a lumpectomy , and without radiation therapy, carries a 25 percent to 35 percent chance of recurrence. Adding radiation therapy to the treatment decreases this risk to about 15 percent. Currently, the long-term survival rate for women with ductal carcinoma in situ is nearly 100 percent.
Recommended Reading: Estrogen Positive Metastatic Breast Cancer
How Is Noninvasive Breast Cancer Treated
The standard treatment for DCIS is surgery. In most cases, women can opt for lumpectomy, which is breast-conserving surgery. It only removes the area with the cancer and some healthy tissue surrounding it. Radiation therapy is usually necessary after to decrease the risk of the cancer returning. Sometimes, doctors recommend mastectomy, which removes the entire breast. This may be the best choice if the DCIS is large or there are multiple spots within the breast.
Your preference also plays a role in the extent of surgery. A second opinion can help you make this decision. The process can give you another point of view or verify what you have already heard. In either case, you will be making an informed decision, which can increase your confidence.
Hormone therapy will be a treatment option for hormone receptor-positive tumors. Your pathology report will tell your doctor whether or not this treatment is appropriate.
LCIS does not require treatment, but it does increase your risk of breast cancer in the future. Your doctor may recommend additional screening exams, estrogen blocking, or preventive mastectomy.
Types Of Invasive Breast Cancer
Two types account for about 90% of invasive breast cancer.
- Invasive ductal carcinoma . This is the most common type, making up about 80%. With IDC, cancer cells start in a milk duct, break through the walls, and invade breast tissue. It can remain localized, which means it stays near the site where the tumor started. Or cancer cells may spread anywhere in the body.
- Invasive lobular carcinoma . This type accounts for about 10% of invasive breast cancers. ILC starts in the lobules or milk glands and then spreads. With ILC, most women feel a thickening instead of a lump in their breast.
Some women may have a combination of both or a different type of invasive breast cancer.
Recommended Reading: Does Stage 2 Breast Cancer Require Chemotherapy
How Long Does It Take For Stage 1 Breast Cancer To Develop Into Stage 2
It is not possible to determine exactly how long it will take for newly diagnosed breast cancer to progress from stage 1 to stage 2. It can happen within months if it is an aggressive high-grade tumor, or it can take longer. It’s important to know that stage 1 breast cancer could have already been present for a while before being detected, so it may progress quickly.
The Overall Survival Rate For Micro
In terms of management and follow up, it is felt that microinvasive breast carcinoma behaves in a manner more like DCIS than invasive ductal carcinoma. The rate of local recurrence is generally 17% or less, and distant metastasis is extremely rare. The overall 5 year survival rate for women with microinvasive carcinoma of the breast can be estimated at around 95% or higher.
You May Like: Is Weight Loss A Symptom Of Breast Cancer
Diagnosis Of Invasive Ductal Carcinoma
Diagnosing invasive breast cancer usually involves many steps. The first is a physical exam and medical history. Doctors can often feel the lump in your breast. They’ll check your armpits and surrounding areas for changes, too.
A mammogram is the next step. This is an x-ray of your breast tissue. It allows doctors to see any tumors or lumps of abnormal tissue. This is the same screening done in healthy women to detect breast cancer early. Ultrasounds and MRIs provide additional images if needed. The biopsy comes last. Doctors remove the lump during surgery. Then, they test the tumor to diagnose cancer.
What Is Tumor Grading
After surgery to remove the tumor, a doctor will check it and assign a grade to it. The grade depends on how closely the cancer cells resemble normal cells when viewed under a microscope. Low-grade cancer cells are similar to normal breast cells. Higher grade breast cancer cells look more different. They show the cancer is more aggressive.
The doctor will also test for estrogen receptors and progesterone receptors. This test will show whether the female hormones — estrogen and progesterone — influence the cancer cells. If the test is positive, it means hormones cause the cancer cells to grow. In that case, therapies to suppress or block hormones may help treat the cancer.
The cancer will also be tested for a gene called HER2. If itâs found, additional drugs like trastuzumab can be used.
Other tests will see if the cancer has spread from the breast to other areas of the body.
Don’t Miss: Stage 3 Breast Cancer Treatment
What Are Lymph Nodes
You have hundreds of lymph nodes throughout your body. Your lymph nodes are part of your lymphatic system, which, in turn, is part of your immune system.
Lymph nodes are little bean-shaped structures that contain immune cells that help fight infection. Theyre connected by a system of lymph vessels that carry fluid throughout your body. As fluid passes through your lymph nodes, they filter out harmful substances.
Cancer spreads when cancer cells break away from the primary tumor. In breast cancer, these cells are most likely to reach the lymph nodes closest to the affected breast.
Usually, these lymph nodes are under the arm, but there are also clusters of lymph nodes near the collarbone and breastbone.
The ones that are closest to your breast are called sentinel lymph nodes. The nodes under your armpit are called axillary lymph nodes.
Even if cancer has reached nearby lymph nodes, it doesnt mean it has spread to other areas. But cancer that reaches the lymph system or bloodstream has a greater potential to travel to other parts of the body.
Breast cancer that has spread to lymph nodes may be treated more aggressively than if it hadnt reached these nodes.
The 5-year survival rate for breast cancer that hasnt reached nearby lymph nodes is 99 percent versus 86 percent when it has.
Who Is More Likely To Develop Lobular Breast Cancer
Risk factors for developing lobular breast cancer are the same as those for developing breast cancer in general. These include:
- Older age. The risk of breast cancer increases with age. Most breast cancers are diagnosed after age 50.
- Being diagnosed with lobular carcinoma in situ. This means you have abnormal cells confined within the lobules of your breast. Although this is not considered cancer, it does increase your risk of developing breast cancer.
- Family history of breast cancer. Having a mother, sister, or daughter who has had breast cancer.
- Early puberty/late menopause. Starting your period at an early age or experiencing late menopause .
- Not having children/later childbirth. Not having children or having your first child after the age of 35.
- Postmenopausal hormone use. Using the female hormones estrogen and progesterone for more than 5 years to manage menopause symptoms.
- Exposure to radiation. Receiving radiation to the breast or chest to treat cancer before the age of 30.
- Having genetic mutations for certain types of breast cancer. Being a carrier of the familial breast cancer genes, BRCA1 and BRCA2.
- Being overweight.
- Drinking alcohol. Compared with nondrinkers, women who consume one alcoholic drink a day have a 10% increase in risk. The risk increases the more you drink.
Don’t Miss: How Long Does Breast Cancer Treatment Take
Less Common Types Of Invasive Breast Cancer
There are some special types of breast cancer that are sub-types of invasive carcinoma. They are less common than the breast cancers named above and each typically make up fewer than 5% of all breast cancers. These are often named after features of the cancer cells, like the ways the cells are arranged.
Some of these may have a better prognosis than the more common IDC. These include:
- Adenoid cystic carcinoma
- Low-grade adenosquamous carcinoma
- Medullary carcinoma
Some sub-types have the same or maybe worse prognoses than IDC. These include:
- Metaplastic carcinoma
- Micropapillary carcinoma
- Mixed carcinoma
In general, all of these sub-types are still treated like IDC.
Morphological Characteristics Of Lobular Neoplasia And Invasive Lobular Carcinoma
Diagnostic criteria for lobular neoplasia and ILC are now well established and described and so are only briefly outlined below. The term lobular neoplasia was introduced to encompass a spectrum of in situ neoplastic proliferations including atypical lobular hyperplasia and lobular carcinoma in situ , which describe different levels of involvement of individual lobular units. The descriptions ALH and LCIS are widely used to classify these lesions since they confer different relative risks for the patient to subsequently develop invasive cancer compared with the general population . By definition, neoplastic cells of LN remain confined to the terminal duct-lobular unit, but they may exhibit pagetoid spread in which cells can migrate along the ductal system between the basement membrane and normal epithelial cell population .
Figure 1
You May Like: Mayo Clinic Breast Cancer Symptoms
Hormonal Therapy For Idc
If the cancer tested positive for hormone receptors, your doctor likely will recommend some form of hormonal therapy. Hormonal therapy, also called anti-estrogen therapy or endocrine therapy, works by lowering the amount of estrogen in the body or blocking the estrogen from signaling breast cancer cells to grow. Because hormonal therapy affects your whole body, its sometimes called a systemic treatment.
In some cases of advanced-stage IDC, hormonal therapy can be given before surgery to help shrink the cancer . Still, its more common for hormonal therapy to start after other treatments, such as chemotherapy or radiation therapy, unless these treatments arent needed.
Hormone receptors are special proteins found on the surface of certain cells throughout the body, including breast cells. These receptor proteins are the eyes and ears of the cells, receiving messages from the hormones in the bloodstream and then telling the cells what to do. In other words, the receptors act like an on-off switch for a particular activity in the cell. If the right substance comes along that fits into the receptor like a key fitting into a lock the switch is turned on and a particular activity in the cell begins.
You and your doctor will work together to decide which form of hormonal therapy is best in your situation. Two types of hormonal therapy are most frequently used:
Also Check: Stage 4 Carcinoma
What If My Report Mentions Her2/neu Or Her2
Some breast cancers have too much of a growth-promoting protein called HER2/neu . The HER2/neu gene instructs the cells to make this protein. Tumors with increased levels of HER2/neu are referred to as HER2-positive.
The cells in HER2-positive breast cancers have too many copies of the HER2/neu gene, resulting in greater than normal amounts of the HER2 protein. These cancers tend to grow and spread more quickly than other breast cancers.
All newly diagnosed breast cancers should be tested for HER2, because women with HER2-positive cancers are much more likely to benefit from treatment with drugs that target the HER2 protein, such as trastuzumab , lapatinib , pertuzumab , and T-DM1 .
Testing of the biopsy or surgery sample is usually done in 1 of 2 ways:
- Immunohistochemistry : In this test, special antibodies that will stick to the HER2 protein are applied to the sample, which cause cells to change color if many copies are present. This color change can be seen under a microscope. The test results are reported as 0, 1+, 2+, or 3+.
- Fluorescent in situ hybridization : This test uses fluorescent pieces of DNA that specifically stick to copies of the HER2/neu gene in cells, which can then be counted under a special microscope.
Many breast cancer specialists think that the FISH test is more accurate than IHC. However, it is more expensive and takes longer to get the results. Often the IHC test is used first:
Read Also: Etiology Of Basal Cell Carcinoma
Don’t Miss: Stage 3 B Breast Cancer
What Is Ductal Carcinoma In Situ
Ductal carcinoma in situ is a very early form of breast cancer thats confined to the milk ducts, which is why its called ductal. Carcinoma is the name for any cancer that begins in cells that line the inner or outer surfaces of tissues, such as the breast ducts. In situ is a Latin term meaning in its original place. DCIS is the most common form of noninvasive breast cancer.
DCIS is classified as low, intermediate, or high grade. Grades are based on what the cells look like under a microscope. The lower the grade, the more closely DCIS resembles normal breast cells. The higher the grade, the more different it is from normal cells. DCIS can sometimes involve the nipple, causing it to look red and scaly. This is a rare form of cancer known as Pagets disease of the breast .
In some women, DCIS may not progress to invasive cancer in their lifetime. This has fueled debate about DCIS about whether women with low-risk disease need any treatment, or if they could be safely checked with annual mammograms and breast exams to see if the cancer is progressing. Currently, the standard treatment for DCIS includes surgery, often a lumpectomy.
Breast Cancer Survival Rates Are Affected By Tumor Grade
Breast cancer grade refers to the size and shape of the malignant breast cancer cells. If the breast cancer cells look very different than normal breast tissue cells, and somewhat random in appearance, they are called poorly differentiated and described as high grade.
There are three main breast cancer grades and these are as follows:-
- Grade 1: The cancer cells are well differentiated and look the most like normal cells. These type of cancers tend to be slow-growing.
- Grade 2: These cancer cells are moderately differentiated. This means that the cells look less like normal cells and tend to grow faster.
- Grade 3: Poorly differentiated cells do not appear like normal cells at all and tend to be very fast growing. Hence, the affect on prognosis.
Microscopic Images of Ductal cell carcinoma in Situ Grades 1, 2 and 3
Higher grade breast cancers tend to have a poorer prognosis.
You will be able to find the Grade of your tumor on your pathology report.
Don’t Miss: Stage-three Cancer
What Is Invasive Ductal Carcinoma
Breast ducts are the passageways where milk from the milk glands flows to the nipple.
Invasive ductal carcinoma is cancer that happens when abnormal cells growing in the lining of the milk ducts change and invade breast tissue beyond the walls of the duct.
Once that happens, the cancer cells can spread. They can break into the lymph nodes or bloodstream, where they can travel to other organs and areas in the body, resulting in metastatic breast cancer.
Myoepithelial Cells As Regulators Of Tissue Polarity
Reversal of inside-out acini by addition of myoepithelial cells. Luminal cells make inside-out acini in collagen. Luminal epithelial cells were double-stained for MUC1 and ESA . In the presence of myoepithelial the acinar polarity is rescued as evidenced by apical expression of MUC1 and ESA . Bar, 25 μm. ).
You May Like: Stage 3 Lymph Node Cancer
How Do You Prevent Invasive Ductal Carcinoma
There is no single way to prevent all cases of breast cancer but people can take steps to lower the risk.
- Lose weight or maintain a healthy weight
- Breastfeed for at least several months
- Use non-hormonal options to treat menopausal symptoms
- For women at increased risk of breast cancer :
- Genetic counseling and testing for breast cancer risk
- Close observation to look for early signs of breast cancer
- More frequent doctor visits for breast exams and ongoing risk assessment
- Start breast cancer screening with yearly mammograms at an earlier age
- Other screening tests, such as breast MRI