Implications For Genetic Testing
The results presented above on the morphological and immunohistochemical characteristics of hereditary breast cancer illustrate major differences between genotypes. The most important were those between tumors in BRCA1 carriers and all other categories. These histopathological features, in conjunction with clinical data, can be used to predict BRCA1 status and, to a lesser extent, BRCA2 and non-BRCA1/2 status and this could have implications for the process of mutation screening.
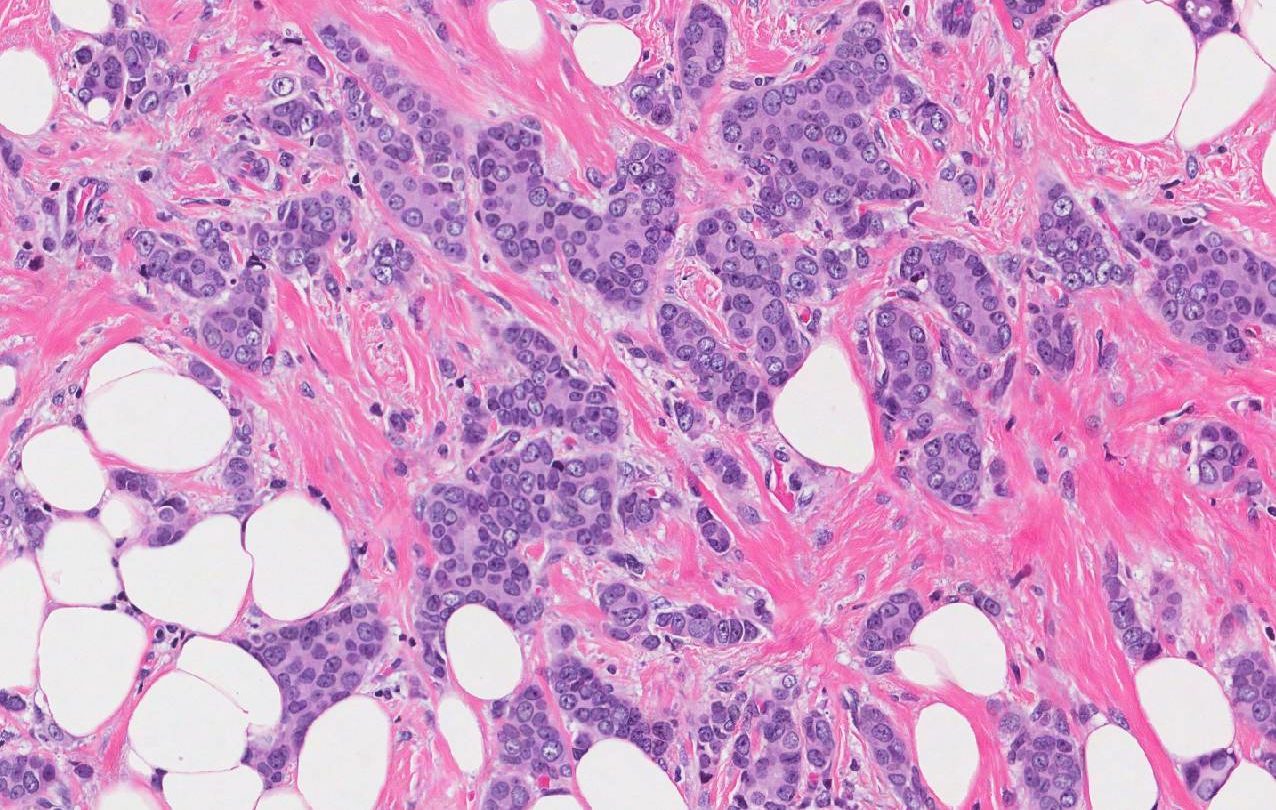
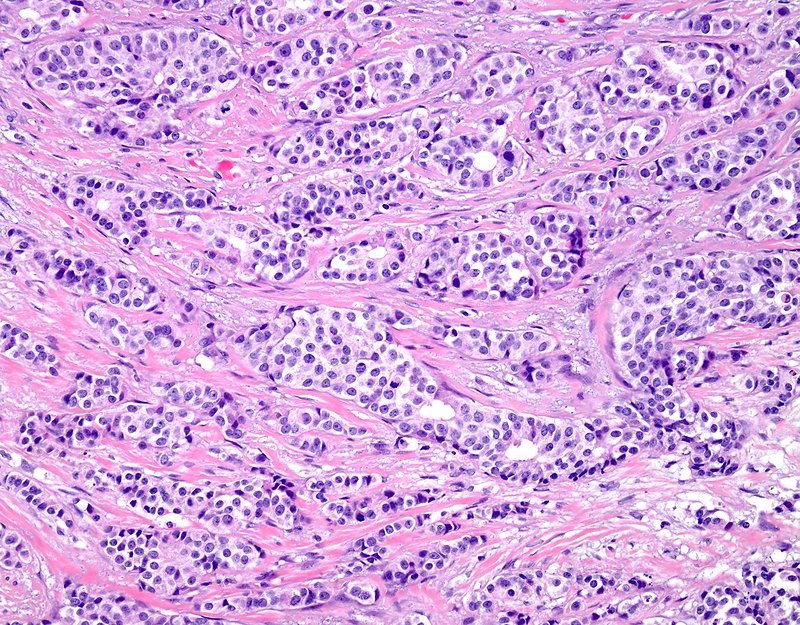
In families with a high incidence of breast and ovarian cancer there is a high probability of finding a BRCA1 or BRCA2 germline mutation. In the absence of other clinical features suggesting the alteration of a specific gene, such as prostate cancer and BRCA2 mutations, histopathological features can be used to indicate which gene should be screened first. Grade 3, estrogen receptor- and progesterone receptor-negative infiltrating ductal carcinomas are more common among BRCA1 patients, specially if they show medullary features. These cases should be also tested for CK5/6 and EGFR expression, since the positive staining of any of these makers further increase the probability of being a BRCA1 mutation carrier. Estrogen receptor- and/or progesterone receptor-positive tumors without evidence of basal differentiation should first be tested for BRCA2 mutations.
How Common Is Hboc
Most breast and ovarian cancers are sporadic, meaning they occur by chance with no known cause. Most women who have breast or ovarian cancer do not have HBOC.
Currently, it is estimated that less than 1% of the general population has a mutation in the BRCA1 or BRCA2 genes, and up to 10% of women and 20% of men diagnosed with breast cancer have a mutation in 1 of these genes. About 10% to 30% of women younger than 60 diagnosed with triple-negative breast cancer, which are cancers that do not have receptors for estrogen, progesterone, and HER2, have a BRCA1 or BRCA2 gene mutation, and others will have mutations in other breast cancer risk genes. Therefore, doctors recommend that women with triple-negative breast cancer receive genetic counseling and genetic testing .
HBOC is most common in families who have had multiple cases of breast cancer and/or ovarian cancer on the same side of the family. In families with 4 or more cases of breast cancer diagnosed before age 60, the chance of HBOC is about 80%. To compare, the chance of finding HBOC when only 1 woman has had breast cancer diagnosed before age 50 is estimated to be 10% or less.
Families with Ashkenazi Jewish ancestry have an increased chance of having HBOC. There are 3 specific gene mutations, known as founder mutations, that are common in these families:
-
185delAG in BRCA1
-
5382insC in BRCA1
-
6174delT in BRCA2
Alterations In Apoptosis Regulation
Dysregulation of apoptosis plays an important role in the pathogenesis and progression of breast cancer, as well as in responses of tumors to therapeutic intervention. Overexpression of BCL2 is commonly observed in estrogen receptor-positive sporadic breast carcinomas and has been associated with a good prognosis. Compared with BCL2, far less is known about the expression of other apoptotic markers in breast tumors in general, and in hereditary cases in particular.
Overexpression of BCL2 in BRCA2 tumors has been reported in several studies, confirming the good correlation between these markers and estrogen receptor status. By contrast, low levels of BCL2 but high levels of caspase 3 were observed in BRCA1 tumors. Caspase 3 is a cytosolic enzyme that is activated only in cells committed to undergoing apoptosis, and is strongly associated with morphological assessment. Thus, previous studies have shown that the apoptotic index obtained by measuring caspase activation was higher in high-grade, estrogen receptor-negative tumors, as has been observed in BRCA1-associated carcinomas. These data are in accordance with an expression study using cDNA microarrays that showed BRCA1-mutation-positive tumors to have increased expression of genes associated with inducing apoptosis , and decreased expression of genes involved in suppressing apoptosis .
You May Like: What Screening Is Used To Test For Breast Cancer
Inheriting Certain Gene Changes
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene changes passed on from a parent.
BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of these genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has up to a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer. ;
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts.
- Women with one of these gene changes also have a higher risk of developing ovarian cancer and some other cancers.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi origin than in other racial and ethnic groups, but anyone can have them.
Other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
Mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Histopathology And Molecular Features Of Familial Non
Very little is known about the genetic basis of non-BRCA1/2 breast cancer. Genetic linkage analysis of families has been performed and several chromosomal regions potentially harboring breast cancer susceptibility genes have been identified, including 8p12p22, 13q21, and 2q31q33. However, these loci have either been shown not to be major predisposing loci, or their status remains to be confirmed, thereby emphasizing genetic heterogeneity and population-specific effects among non-BRCA1/2 families. Non-BRCA1/2 hereditary carcinomas represent 67% of familial breast cancers when families with only female breast cancer and four or five affected members are considered. In the Spanish population, considering families with at least three cases of female breast cancer and one of the affected women being <50 years, 75% of cases were not attributable to BRCA1/2 mutation.
There are three studies that have defined the histological characteristics of these neoplasias., , In the three studies, invasive ductal carcinoma was the most frequent histological type: 77% of the cases according to Lakhani et al, 78% in the series of Palacios et al and 67% in the study of Eerola et al. In two of them,, an excess of lobular carcinomas was found in familial non-BRCA1/2 compared with BRCA1 , BRCA2 , and sporadic cases . The difference was only significant with respect to BRCA1 tumors.
Recommended Reading: How Long Does Someone Live With Stage 4 Breast Cancer
Risks For Breast Cancer
A risk factor is something that increases the risk of developing cancer. It could be a behaviour, substance or condition. Most cancers are the result of many risk factors. But sometimes breast cancer develops in women who dont have any of the risk factors described below.
Most breast cancers occur in women. The main reason women develop breast cancer is because their breast cells are exposed to the female hormones estrogen and progesterone. These hormones, especially estrogen, are linked with breast cancer and encourage the growth of some breast cancers.
Breast cancer is more common in high-income, developed countries such as Canada, the United States and some European countries. The risk of developing breast cancer increases with age. Breast cancer mostly occurs in women between 50 and 69 years of age.
Criteria For Genetic Screening
Clinical criteria for genetic testing were suggested as following: bilateral lobular breast cancer with or without family history of breast cancer, with age at onset <50 years; and unilateral lobular breast cancer with family history of breast cancer, with age at onset <45 years. In this context, it has been estimated that the frequency of E-cadherin germline mutation is a rare event, affecting about 3% of the screened population. However, there are ongoing studies to assess the penetrance and the cancer risk in the hereditary lobular breast cancer syndrome.
Also Check: Do Hormones Cause Breast Cancer
What Is The Prognosis For Invasive Ductal Carcinoma
Based on individual markers and prognostic factors, including the staging of your tumor, your physician will work to give you a prognosis. At Johns Hopkins Medicine, our team of breast cancer specialists is dedicated to developing cutting-edge techniques for surgery, breast reconstruction, chemotherapy, biologic targeted therapy, radiation therapy and other hormonal therapies. Our research allows us to make great strides forward for patients with breast cancer.
How Well Do Different Guidelines Identify Women With Inherited Mutations
The American Society of Breast Cancer Surgeons
ASBrS recommends testing for all women with breast cancer. An XRAY review of the ASBrS recommendations can be found here. Using ASBrS guidelines:
- According to these guidelines, in this study, all participants with mutations would be identified.
Pro: All women with mutations would be identified; none would be missed.
Con:;3,666 women who did not have an inherited mutation were tested, which may have caused unnecessary cost, stress and anxiety.
The National Comprehensive Cancer Network
NCCN;has a complex set of guidelines for genetic testing recommendations . Using current NCCN guidelines:
- 169 of the 3,907 participants had a genetic mutation in one of 9 actionable breast cancer genes and would qualify for genetic testing under NCCN guidelines.
- These 169 women represented 70% of 241 women with an inherited mutation.
Pro: Fewer women without inherited mutations were tested than under ASBrS guidelines and did not unnecessarily face the potential stress and anxiety of genetic testing.
Con: A large portion women with an inherited mutation were not identified, which prevented them from using this information to guide their treatment and surgical decisions.
Expanded NCCN guidelines
Don’t Miss: How Do You Know You Have Breast Cancer
How Is Hboc Identified
Mutations in the BRCA1 or BRCA2 genes can be identified through a blood or saliva test. The usual method of testing, called standard gene sequencing, can find most BRCA mutations. There are other types of mutations called rearrangements, which include deletions or duplications in BRCA1 and BRCA2 that also may cause an increased risk for these cancers. Testing is also available for large rearrangements in BRCA1 and BRCA2.
After initial BRCA1 and BRCA2 genetic testing, additional testing may be recommended if:
- The results were negative, meaning no genetic mutation was detected
- A variant of uncertain significance was detected, which means that there is a genetic change, but it is not known how that change could affect cancer risk
Talk with your health care team and/or a genetic counselor for more information.
Most, but not all, insurance providers, including Medicare and Medicaid, cover the cost of complete BRCA1 and BRCA2 testing. Many genetic specialists offer multigene panels, which may include 6, 20, 40, or more genes depending on your personal and family history. The multigene panel tests may often be done at the same time as BRCA1 and BRCA2 testing. Talk with your genetic counselor for more information on the type of testing you will have and your insurance coverage before testing begins.
Other Cancer Risks For People With Hboc
Anyone with mutations in the BRCA2 gene may be at an increased risk of other types of cancer, including melanoma and pancreatic, stomach, esophageal, and bile duct cancers.Mutations in other genes may be associated with an increased risk of developing breast and other cancers, including the Li-Fraumeni syndrome , Cowden syndrome, and others. The pattern of cancers in the family is often a clue to the specific gene that may explain the hereditary cancer for that family. Multigene panels are available for people with a strong personal and family history of cancer. Multigene panel tests include BRCA1 and BRCA2 and many other genes that increase the risk of breast, ovarian, and other cancers. If your BRCA1 and BRCA2 test was negative, then you may or may not have mutations in other genes. A newer type of testing, called next generation sequencing, massively parallel sequencing, or deep sequencing, has made testing for multiple genes at the same time faster and less expensive. If a genetic mutation is found, this could explain the cancers in a specific family and provide information about who is at risk and the appropriate types of monitoring and prevention/risk reduction methods.
You May Like: What Is Stage 2 Cancer Of The Breast
Guidelines For Elective Surgical Options
Women with BRCA1 or BRCA2 mutations face a significant risk of breast and ovarian cancer. Prophylactic removal of the fallopian tubes and ovaries is recommended by about age 40.; Many women with BRCA1 or BRCA2 mutations will also elect to have their breasts removed. Nipple-sparing mastectomy is an effective option for these women.;
Making the decision to have an elective preventive double mastectomy and removal of the ovaries is personal and should be based on many life factors. You must balance where you are in your childbearing years, what your future choices may be, and whether you would prefer to follow a rigorous screening schedule instead of making such a life-altering choice.
Whatever your decision, we encourage you to make an informed choice. If you do elect to have a preventive double mastectomy, our breast specialists will guide you in the appropriate breast surgery reconstruction to help restore your body image after treatment.
If you are interested in discussing ovary removal surgery , we will refer you to one of our gynecological oncologists.
Show me more…
Guidelines For Breast Cancer Screening
Breast cancer screening guidelines for average risk women have become confusing. One organization recommends that women start getting mammograms every other year at age 50 and another recommends yearly mammograms between age 45 and 55 with every other year mammograms thereafter.;One reason for these differences is disagreement as to whether annual mammography in younger women can reduce the risk of dying of breast cancer. At Johns Hopkins, we continue to recommend annual mammography beginning at age 40 for average risk women,
Extra screening tests are recommended for women with higher than average risk for breast cancer. Current guidelines suggest that if you have more than a 20% risk of developing breast cancer during your lifetime you should consider adding screening breast MRI to your mammogram.;Women who carry mutations in BRCA1, BRCA2, PALB2, or CHEK2 will meet this risk threshold. Other women with family history of breast cancer or a history of a breast biopsy showing high risk changes may meet this criterion as well. You can calculate your breast cancer risk ;online using the Gail model or the BCSC model . Breast specialists in the Johns Hopkins Breast Center have access to additional resources for calculating your breast cancer risk. At Johns Hopkins enhanced surveillance for high risk women consists of a breast exam every 6 months alternating mammograms with MRI scans.
Don’t Miss: What Does Breast Cancer Cause
What Do The Test Results Mean
The results of HER2 testing will guide you and your cancer care team in making the best treatment decisions.
It is not clear if one test is more accurate than the other, but FISH is more expensive and takes longer to get the results.;Often the IHC test is done first.
- If the IHC result is 0 or 1+, the cancer is considered HER2-negative. These cancers do not respond to treatment with drugs that target HER2.
- If the IHC result is 3+, the cancer is HER2-positive. These cancers are usually treated with drugs that target HER2.
- If the IHC result is 2+, the HER2 status of the tumor is not clear and is called “equivocal.” This means that the HER2 status needs to be tested with FISH to clarify the result.
Triple-negative breast tumors dont have too much HER2 and also dont have estrogen or progesterone receptors. They are HER2-, ER-, and PR-negative. Hormone therapy and drugs that target HER2 are not helpful in treating these cancers. See Triple-negative Breast Cancer to learn more.
Triple-positive breast tumorsare HER2-, ER-, and PR-positive. These cancers are treated with hormone drugs as well as drugs that target HER2.
Our team is made up of doctors and;oncology certified nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.
Last Revised: September 20, 2019
Support For People With Inherited Gene Mutations
Some support groups are tailored to people with BRCA1, BRCA2 or other high-risk gene mutations and those with breast cancers related to inherited gene mutations.
Our Support section offers a list of resources to help find local and online support groups. For example, FORCE is an organization that offers online support for people at higher risk of breast, ovarian or other cancers related to family history or inherited gene mutations.
Sharsheret offers online support for Jewish women affected by hereditary breast and/or ovarian cancer.
|
;Susan G. Komen® Support Resources |
|
You May Like: What Age Do Women Get Breast Cancer