Breast Pain After Menopause Can Come In Many Forms
Menopause has come and gone. Why do I still have breast pain?
In most cases, breast pain is a by-product of reproductive life: Like breast swelling, it waxes and wanes during the menstrual cycle, and it’s one of the first symptoms of pregnancy. Many women expect breast pain to go away after menopause. When it doesn’t, they may fear they have breast cancer. Fortunately, breast pain is rarely a symptom of cancer, regardless of age. Still, that possibility should be considered, along with a number of noncancerous conditions that affect the breasts.
Your Race And Ethnicity
White and Black women have the highest risk of developing breast cancer in their lifetime. Asian/Pacific Islander and Hispanic/Latina womens breast cancer rates fall in between two major groupings while American Indian and Alaska Native women are on the lowest end of risk.
While white women are more likely to develop breast cancer than Black women overall, they tend to be diagnosed at an older age . Black women have the highest breast cancer rates among women under age 40. Black women make up a higher percentage of triple-negative breast cancer cases.
What to do: If your race or ethnicity places you at higher risk, make sure you follow all screening recommendations to improve your chances of catching cancer early.
Implications For Clinicians And Policymakers
This study delivers more generalisable estimates of the different risks of breast cancer associated with specific progestogen components of HRT, while confirming no increased risks from short term use of oestrogen only, estradiol-dydrogesterone, and tibolone. Increasing duration of use was generally associated with increased risk, with tibolone and estradiol-dydrogesterone showing the smallest risks. The frequency of prescribing for treatments including dydrogesterone was, however, much lower than for those including norethisterone, medroxyprogesterone, or levonorgestrel.
Recommended Reading: What Does Pt1c Mean In Breast Cancer
Menopausal Hormone Therapy And Cancer Risk
For decades, women have used hormone therapy to ease symptoms of menopause, such as hot flashes and sweating. This is called;menopausal hormone therapy, and you may see it abbreviated as HT or MHT. You may also hear it described as;hormone replacement therapy;,;postmenopausal hormone therapy;, or;postmenopausal hormones;.
In the past, many doctors and their patients believed that MHT didnt just help with hot flashes and other symptoms it had important health benefits. But well-conducted studies have led many doctors to conclude that the risks of MHT often outweigh the benefits.
This information covers only how MHT can affect a womans risk of getting certain cancers. It does not cover other possible risks of MHT such as heart disease or stroke.
You can use this information when you talk to your doctor about whether MHT is right for you.
Age At Menarche Is More Influential Than Age At Menopause On Breast Cancer Risk

The observation that lengthening the reproductive life of a woman, either by an earlier menarche or later menopause, increases the risk of breast cancer would suggest that the overall duration of the exposure to estrogen is underlying the risk. However, a recent meta-analysis of reproductive events and breast cancer risk has found that age at menarche may be more of a deciding factor on the risk than age at menopause .
These findings contradict earlier theories that the influence of age at menarche and menopause on breast cancer risk was simply due to the duration of exposure to cycling ovarian hormones. Instead, it seems that the timing of the first exposure of the mammary gland to cyclic hormones sets up a developmental program that has consequences for breast cancer risk later in life.
Read Also: When Can Breast Cancer Occur
What Are The Treatments For Noncyclic Breast Pain
Its more difficult to figure out the best treatment for noncyclic breast pain. Thats because its hard to know exactly where the pain is coming from. In addition, the pain is not hormonal. Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
Your healthcare provider will do a physical exam and may order a mammogram. In some cases, a biopsy of the area is also needed. If it is found that the pain is caused by a cyst, then the cyst will be aspirated. This means that a small needle will be used to remove the liquid contents of the cyst. Depending on where the pain starts, treatment may include pain relievers, anti-inflammatory medicines, and compresses.
What Causes Breast Cysts
Breasts are made up of lobules and ducts . The milk glands are surrounded by fibrous support tissue and fat, known as breast tissue. This tissue gives breasts their size and shape. Sometimes, the milk glands can fill up with fluid; these are breast cysts.
Cysts may appear naturally as the breast alters with age, due to normal changes in the oestrogen hormone levels. During the menstrual cycle oestrogen causes fluid to be produced. Although you can develop breast cysts at any age, theyre most common in women over 35.
After the menopause , as oestrogen levels fall, cysts usually stop forming. Women who have hormone replacement therapy may still get cysts.
Also Check: How To Tell If Breast Cancer Has Metastasized
Previous Breast Cancer Or Lump
If you have previously had breast cancer or early non-invasive cancer cell changes in breast ducts, you have a higher risk of developing it again, either in your other breast or in the same breast.
A;benign breast lump does not mean;you have breast cancer, but certain types of breast lumps may slightly increase your risk of developing cancer.
Some benign changes in your breast tissue, such as;cells growing abnormally in ducts;, or;abnormal cells inside your breast lobes , can make getting breast cancer more likely.
Breast Cancer And Hormone Replacement Therapy
Menopause can trigger unpleasant side effects such as hot flushes and vaginal dryness. Hormone replacement therapy eases the symptoms by boosting sex hormone levels. It also reduces the risk of osteoporosis and heart disease.;
Since some breast cancers depend on oestrogen, women taking HRT for a long time have a 0.3-fold increased risk. Women who undergo HRT for shorter periods have the same risk of breast cancer as women who have not used HRT. The health benefits of HRT in women in early post-menopause may outweigh the risks in many cases.
Read Also: Are Breast Cancer Tumors Hard Or Soft
The Role Of Estriol In Breast Cancer Prevention
Estriol, the weakest of the three estrogens is thought to protect against breast cancer by softening the effects of its more potent sisters. A revisiting of the literature finds that estriol is vitally important, precisely because it is a weak estrogen. And a number of studies, published over four decades, have demonstrated that estriols unique and perhaps most important role, may be to oppose the growth of cancers, including breast cancer. When lower-strength estriol is used topically, it does not raise the risk of breast cancer as stronger and/or synthetic estrogens do.
Estriols protective action is linked to its ability to bind loosely to hormone receptors on the cell walls of breast tissue, thus blocking more potent estrogens from occupying the sites and stimulating breast cells to grow. Unlike these more excitatory estrogens, estriol does not stimulate growth nearly as much. Some of the best research on the inherent strengths of this weakest of estrogens has been done in Europe where estriol has been more readily available and studied for years:
Women in Balance suggests talking to your physician about bioidentical hormone treatments containing estriol.
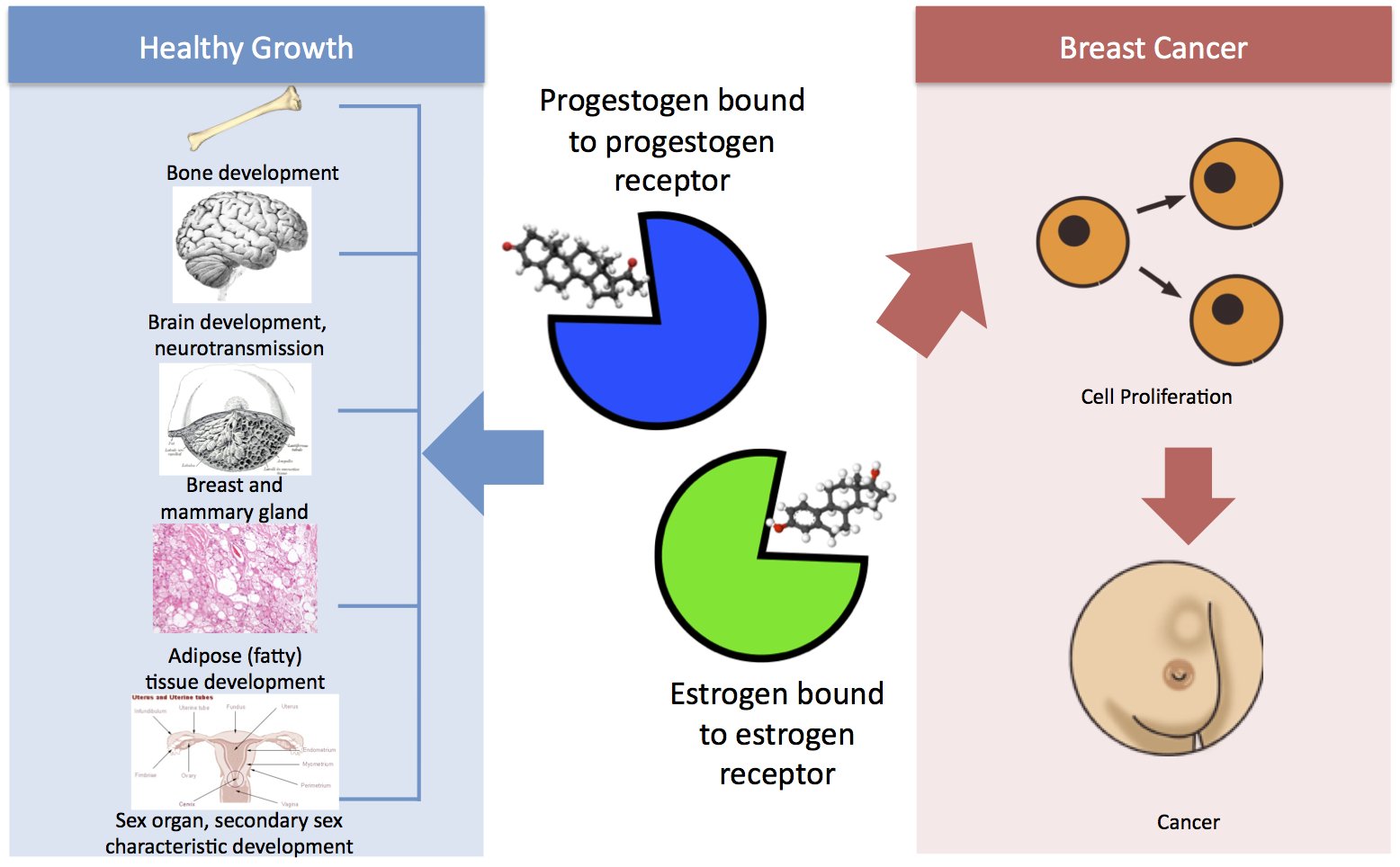
The Proliferative Effects Of Oestrogen
Oestrogens have a marked proliferative effect on breast epithelial tissue in model systems . Both endogenous and exogenous oestrogens stimulate breast epithelial cell mitosis, increasing the number of cell divisions and thus the opportunity for random genetic errors . Oestrogen concentrations may be important at all stages in the development of breast neoplasms because the hormonal stimulus to cell division continues all along the progression pathway . The proliferative effects of oestrogens are brought about on entering target cells, where they bind with a receptor protein, which then binds to hormone response elements on the nuclear DNA, activating or suppressing specific sequences in the regulatory regions of genes responsive to oestrogen that control cell growth and differentiation .
It has also been suggested that oestrogens might have an important influence on risk for developing breast cancer through effects before the initiation of the disease . Raised oestrogen levels during fetal life have been shown to influence morphology of the mammary gland , and increased levels are also thought to be responsible for the persistence of epithelial structures that are known to be sites of malignant transformation . Furthermore, results from animal models and indirect human evidence indicate that exposure to elevated oestrogen levels in utero may increase the risk for developing breast cancer in adulthood .
Also Check: What Do Nipples Look Like When You Have Breast Cancer
How Your Diet May Affect Your Risk Of Breast Cancer
Eating right is one important way you may be able to lower your risk of breast cancer. The American Cancer Society recommends eating mostly vegetables, fruits, and whole grains, and less red meat , less processed meat , and fewer sweets. A healthy diet can help reduce the risk of heart disease, diabetes, stroke, and certain cancer types.
A healthy diet can also help you get to and stay at a healthy weight. Overweight and obesity increase the risk for getting breast cancer. Whats less clear is the link between breast cancer risk and any one food type. Many studies about foods and breast cancer risk have had different results, but no clear-cut answers. Here is what the evidence tells us about fat, vitamin supplements, soy, dairy, and sugar.
Breast Cancer Risk From Using Hrt Is Twice What Was Thought
Study prompts medicines regulator to advise all women using HRT to remain vigilant
The risk of breast cancer from using hormone replacement therapy is double what was previously thought, according to a major piece of research, which confirms that HRT is a direct cause of the cancer.
The findings of the definitive study will cause concern among the 1 million women in the UK and millions more around the world who are using HRT. It finds that the longer women take it, the greater their risk, with the possibility that just one year is risk-free. It also finds that the risk does not go away as soon as women stop taking it, as had been previously assumed.
The UKs drug licensing body suggested women who have used HRT in the past or use it now should be vigilant for signs of breast cancer in the light of the findings, while the Royal College of GPs urged them not to panic but to consult their doctor if they are concerned.
The research, , says one in 50 women of average weight taking the most common form combined daily oestrogen and progestogen for five years will get breast cancer as a result.
That risk is twice what was thought, because it continues at some level for 10 or more years after women stop taking HRT. There are about 1 million women in the UK on HRT, 5 million in the rest of Europe and 6 million in the US.
Read Also: Can Breast Cancer Cause Shortness Of Breath
Estrogen Does Not Cause Breast Cancer: Debunking Common Myths About The Hormone
It is very popular to vilify estrogen these days. The most obvious reason is the result of several sensationalized interpretations of the famous WHI “Prempro” data first out in 2002. While the attempt to objectify the effects of post-menopausal hormone replacement therapy is highly admirable, confusion and inappropriate interpretations have resulted in unprecedented fear of “all things estrogen.” This has created huge challenges for those of us who are interested in the wellness and education of women.
MYTH: “Estrogen causes breast cancer.”
REALITY: The best data indicates that not only does estrogen not cause breast cancer; estrogen supplementation after menopause might have a slight protective effect.
Estrogen induces breast development in our species, so of course there is a strong relationship with breast disease and the hormone that regulates breast growth– but balance is the key. Persistently high levels of estrogen, such as in the obese woman can promote growth of abnormal cells that might otherwise have been plucked out by the immune system. This is not causation, but facilitation after the fact. Stating that estrogen causes breast cancer is like saying fertilizer causes weeds. In a garden even weeds need some soil nutrients, and if these are completely removed, the weeds can’t grow…but neither can the desired plants. The fact is the positive metabolic effects of ideal amounts of estrogen may help the body defend itself from breast cancer before it starts.
Hrt And Breast Cancer
So far there have been more than 60 analytical studies investigating the relationship between menopausal HRT and breast cancer risk. Data from these studies were brought together in a pooled analysis , which found that current users of HRT, or those who ceased use 14 years previously, had a 2.3% excess risk of being diagnosed with breast cancer for each year of use, an increase in risk that is comparable with the effect of delaying menopause for a year . The excess risk of breast cancer among women who had used HRT for 5 years or longer was 35%. This effect was reduced after ceasing use of HRT and had largely, if not wholly, disappeared after about 5 years. These results did not vary significantly by type of HRT, although the collaborative study had relatively little power to assess relationships with combined oestrogenprogestin therapy. More recent studies have reported that the long-term use of preparations containing progestins is more detrimental than the use of oestrogen alone . Recent data from three randomised controlled trials have confirmed that exposure to oestrogens plus progestins for 5 years is associated with an approximate 2630% increase in risk for breast cancer .
Also Check: How Many People Survive Breast Cancer
Metabolism And Thyroid Hormone Balance
The Colorado Thyroid Disease Prevalence Study in 2000 found the rate of hypothyroidism in the general population to be approximately 10%, with an estimated 13 million undiagnosed cases of low thyroid among American adults. Interestingly, women have an approximately seven times greater risk for developing thyroid problems than do men. Thyroid hormone regulates metabolic rate, so low levels tend to cause unwanted weight gain, depression, low energy and cold intolerance. High thyroid levels cause hyper energy levels, a feeling of being too warm all the time, and persistent weight loss. But it is hypothyroidism, or low thyroid, that is most common in women during the perimenopausal and postmenopausal years; in fact, some 26% of women in or near menopause are diagnosed with hypothyroidismand this is the period when breast cancer begins to rise sharply!
Binding Proteins And The Bioavailability Of Oestrogens
The availability of oestrogen in tissues is determined not only by the production of the hormone and concentrations in circulation but also by the extent to which it is bound to a binding protein, sex-hormone-binding globulin . Thus, high concentrations of SHBG decrease the proportion of oestradiol that is able to leave the circulation and enter the cells. SHBG might partly mediate the effects of obesity in postmenopausal women because obesity is associated with lower levels of SHBG and an inverse association has been observed between concentrations of SHBG and breast cancer risk in postmenopausal women . So far, however, the few studies that have investigated the relationship between SHBG and breast cancer risk in premenopausal women have failed to find an association .
Don’t Miss: Who Is At High Risk For Breast Cancer
Effects On Other Target Organs
Tamoxifen and raloxifene have effects on other target sites that may affect the balance of clinical benefits and risks.
Bone
Tamoxifen has an agonist effect on bone and promotes a gain in bone density at least in post-menopausal women . Raloxifene also has estrogen agonistic activity in bone and increases bone mineral density . Raloxifene also decreases the risk of vertebral fractures in post-menopausal women with osteoporosis .
Cardiovascular system
Both tamoxifen and raloxifene have estrogen agonist effects on serum lipids with an increase in high density lipoprotein and a decrease in low density lipoprotein cholesterol and total cholesterol. Raloxifene decreased cardiovascular events by 40% in the MORE trial . Tamoxifen has been associated with a reduction in coronary artery disease in some but not all adjuvant or prevention trials . It is of interest that estrogen also increases high density lipoprotein cholesterol concentration, but does not decrease coronary artery disease events .
Endometrium
Tamoxifen has agonist effects on uterine endothelium and is associated with an increased risk of endometrial cancer in adjuvant trials . In contrast, raloxifene appears to have neutral actions on uterine endothelium and is not associated with an increased risk of endometrial cancer.
Central nervous system
Breast cancer prevention
Not Taking Hormonal Therapy As Prescribed Leads To More Recurrence
After surgery, women diagnosed with hormone-receptor-positive breast cancer usually take hormonal therapy medicine to reduce the risk of the cancer coming back . Hormonal therapy medicines work in two ways:
There are several types of hormonal therapy medicines. Tamoxifen, a selective estrogen receptor modulator , is one of the most well-known. Tamoxifen can be used to treat both premenopausal and postmenopausal women. In the early 2000s, the aromatase inhibitors:
- Arimidex
- Aromasin
- Femara
were shown to be more effective at reducing recurrence risk in postmenopausal women and are now used more often than tamoxifen to treat women whove gone through menopause. Aromatase inhibitors arent commonly used to reduce recurrence risk in premenopausal women.
Most women take hormonal therapy for 5 to 10 years after breast cancer surgery.
Both tamoxifen and aromatase inhibitors can cause side effects. Tamoxifen may cause hot flashes and increase the risk of blood clots and stroke. Aromatase inhibitors may cause muscle and joint aches and pains. Less common but more severe side effects of aromatase inhibitors are heart problems, osteoporosis, and broken bones. Research has shown that about 25% of women who are prescribed hormonal therapy to reduce the risk of recurrence after surgery either dont start taking the medicine or stop taking it early, in many cases because of side effects.
for postmenopausal women diagnosed with hormone-receptor-positive disease.
Don’t Miss: What To Say To Breast Cancer Patient