What Are The Risk Factors For Breast Cancer
Being a woman and getting older are the main risk factors for breast cancer.
Studies have shown that your risk for breast cancer is due to a combination of factors. The main factors that influence your risk include being a woman and getting older. Most breast cancers are found in women who are 50 years old or older.
Some women will get breast cancer even without any other risk factors that they know of. Having a risk factor does not mean you will get the disease, and not all risk factors have the same effect. Most women have some risk factors, but most women do not get breast cancer. If you have breast cancer risk factors, talk with your doctor about ways you can lower your risk and about screening for breast cancer.
Environmental And Lifestyle Risk Factors
- Lack of Physical Activity:; A sedentary lifestyle with little physical activity can increase your risk for breast cancer.
- Poor Diet:; A diet high in saturated fat and lacking fruits and vegetables can increase your risk for breast cancer. ;
- Being Overweight or Obese:; Being overweight or obese can increase your risk for breast cancer. Your risk is increased if you have already gone through menopause. ;
- Drinking Alcohol:; Frequent consumption of alcohol can increase your risk for breast cancer. The more alcohol you consume, the greater the risk.
- Radiation to the Chest:;;Having radiation therapy to the chest before the age of 30 can increase your risk for breast cancer. ;
- Combined Hormone Replacement Therapy :; Taking combined hormone replacement therapy, as prescribed for menopause, can increase your risk for breast cancer and increases the risk that the cancer will be detected at a more advanced stage.
Benefits Of Mammographic Screening
The ACS systematic review also examined the effect of screening mammography on life expectancy. Although the review concluded that there was high-quality evidence that mammographic screening increases life expectancy by decreasing breast cancer mortality, the authors were not able to estimate the size of the increase 23.
You May Like: Does Pain In Your Breast Mean Cancer
Determining Your Risk Of Breast Cancer
While knowing your risk is important, experts say, having an increased risk may not necessarily translate to being high risk.
“Not all women who have risk factors that place them at increased risk for breast cancer have a risk that’s high enough to warrant a recommendation for aggressive screening or risk-reduction measures,”;Peshkin says.
To find out your risk level, consider reviewing your personal and family history with a healthcare provider, Peshkin advises.
Another option is to use an online risk assessment instrument such as the National Cancer Institute’s Breast Cancer Risk Assessment Tool, which gauges your risk, Garber suggests.
If you suspect you have a hereditary risk, then consider seeking genetic counseling with a credentialed provider who can review testing options in detail, Peshkin says.
General Considerations For Screening

The goal of screening for cancer is to detect preclinical disease in healthy, asymptomatic patients to prevent adverse outcomes, improve survival, and avoid the need for more intensive treatments. Screening tests have both benefits and adverse consequences .
Breast self-examination, breast self-awareness, clinical breast examination, and mammography all have been used alone or in combination to screen for breast cancer. In general, more intensive screening detects more disease. Screening intensity can be increased by combining multiple screening methods, extending screening over a wider age range, or repeating the screening test more frequently. However, more frequent use of the same screening test typically is associated with diminishing returns and an increased rate of screening-related harms. Determining the appropriate combination of screening methods, the age to start screening, the age to stop screening, and how frequently to repeat the screening tests require finding the appropriate balance of benefits and harms. Determining this balance can be difficult because some issues, particularly the importance of harms, are subjective and valued differently from patient to patient. This balance can depend on other factors, particularly the characteristics of the screening tests in different populations and at different ages.
Don’t Miss: Why Is Left Breast Cancer More Common
Key Points To Remember
- If you have a personal or family history of breast cancer, you need to talk to your doctor to find out how high your risk really is.
- A woman who has inherited a BRCA gene change is very likely to get breast cancer.
- Taking medicines like anastrozole, raloxifene, and tamoxifen may help prevent breast cancer in women who are at high risk.
- Surgery to remove the breasts and/or ovaries greatly lowers the risk of breast cancer in high-risk women.
- Taking medicines and having surgery both have side effects and risks.
- None of the choices can prevent all breast cancer.
- Finding out that you are at high risk for breast cancer is not an emergency. There is plenty of time to carefully think about options.
Breast Cancer And Your Risk
For readers interested in the PDF version, the document is available for downloading or viewing:
This brochure identifies biological as well as lifestyle factors associated with breast cancer. It offers information and advice to help you better understand and address them. It also identifies common misconceptions about breast cancer and includes helpful tips and useful website addresses to help you stay informed.
It is intended for women who:
- are 18 years of age or over; and
- do not have breast cancer or any breast problems. You should report any changes in your breasts or concern you might have about your breasts to your doctor.
Importance Of Risk Assessment
Breast cancer remains a major global problem. Despite a steady reduction in the mortality rates from breast cancer in many Western countries, with the exception of the United States , the incidence of breast cancer continues to increase . Although this increase in incidence is likely to be related predominantly to changes in dietary and reproductive patterns, evidence from genetic studies has also shown an increase in incidence in patients with BRCA1 and BRCA2 mutations .
Flowchart of the management of women who are referred to family history clinics. *High risk usually defined as more than 10% risk of harboring mutation, and low risk usually defined as 10% or lower risk. High risk usually defined as a 5-year risk of developing breast cancer more than 1.67%, and low risk usually defined as a 5-year risk of developing breast cancer 1.67% or lower.
Additional High Risk Breast Screenings
A mammogram is the most important screening exam for early breast cancer detection. However, for some individuals who have an increased lifetime risk of breast cancer, there are additional screenings that your provider may recommend.; Your lifetime breast cancer risk is calculated based on a Cancer Risk Assessment done at time of your mammogram.
The Care Program For Women At High Risk Of Breast Cancer
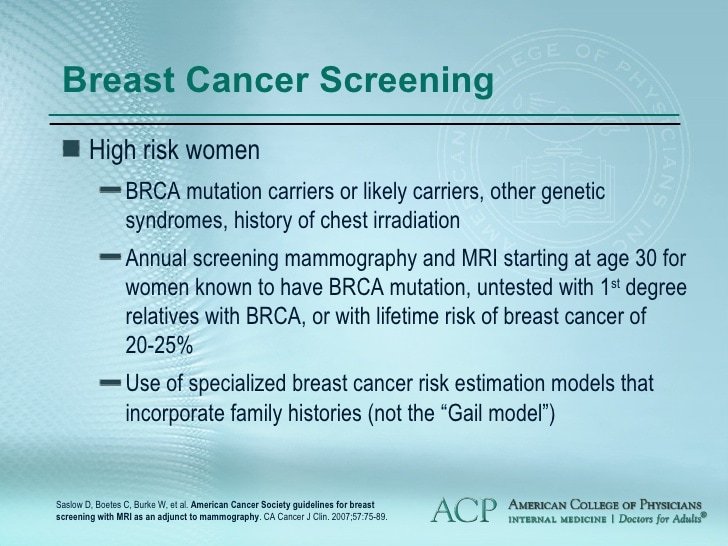
The Division of Breast Surgerys Breast Cancer Assessment and Risk Evaluation program provides assessment, surveillance, and management for patients who have a higher risk of developing breast cancer due to:
- Breast disorders such as atypical ductal hyperplasia , atypical lobular hyperplasia , or lobular carcinoma in situ
- BRCA1 or BRCA2 genetic mutations
- Li-Fraumeni, Peutz-Jeghers, and Cowden syndromes
- Strong family history of premenopausal breast cancer in first-degree relatives
- History of radiation to the chest before age 30
We will tailor a screening and prevention program that meets your needs. We offer:
Watch: Am I At Increased Risk
It’s important to empower yourself with knowledge of your own risk factors for breast cancer.
Depending on your level of risk, your physician could refer you to the high-risk breast cancer prevention program. This program is a diverse team of care providers that includes:
- Genetic counselors
- Lifestyle counselors
What Else Do You Need To Make Your Decision
Check the facts
- Sorry, that’s not right. Sometimes women think that their risk is higher than it really is. That’s why it’s important to talk to your doctor before you consider having any treatment to prevent breast cancer.
- You’re right. Sometimes women think that their risk is higher than it really is. That’s why it’s important to talk to your doctor before you consider having any treatment to prevent breast cancer.
- It may help to go back and read “Get the Facts.” It depends on what kind of family history you have. Sometimes women think that their risk is higher than it really is. Talk to your doctor.
- No, there’s no reason to hurry. For example, some women decide to have extra checkups and testing now and think about surgery later, after they have had children and have finished breastfeeding.
- That’s correct. There’s no reason to hurry. Some women will decide to choose extra checkups and testing now and think about surgery later, after they have had children and have finished breastfeeding.
- It may help to go back and read “Compare Your Options.” There’s no reason to make this decision in a hurry.
- Yes, you’re right. A woman who has inherited a BRCA gene change is very likely to get breast cancer.
- Sorry, that’s wrong. A woman who has inherited a BRCA gene change is very likely to get breast cancer.
- It may help to go back and read “Get the Facts.” A woman who has inherited a BRCA gene change is very likely to get breast cancer.
Being Overweight Or Obese
Women who are overweight after their menopause have a higher risk of breast cancer than women who are not overweight. Men also have an increased risk of breast cancer if they are overweight or obese. For both men and women, the risk increases as more weight is gained.;
Body mass index is a measure that uses your height and weight to work out whether you are a healthy weight. For most adults, an ideal is between 18.5 to 24.9. Being overweight means having a BMI of between 25 and 30. Obesity means being very overweight with a BMI of 30 or higher.
Try to keep a healthy weight by being physically active and eating a healthy, balanced diet.
Drinking alcohol increases the risk of breast cancer in women. The risk increases with each extra unit of alcohol per day. The number of units in a drink depends on the size of the drink, and the volume of alcohol.
The latest UK government guidelines advise drinking no more than 14 units of alcohol a week.
Risk Factors You Can’t Change Or Control
Reproductive history – menstruation, menopause, pregnancy and breastfeeding
Hormones, especially estrogen, can encourage the growth of some types of breast cancers. Estrogen levels increase in woman when they go through puberty and start menstruating, change during pregnancy, and drop when breastfeeding and after menopause . As a result, the lifetime exposure to estrogen is lower in women who:
Different studies have used different ages to look at the relationship between age of menstruation and the risk of breast cancer. As well, there is some evidence that the typical age of menstruation may be changing in North America. As a rule, though, starting to menstruate at a younger age than most of your peers or going through menopause much later in life is associated with a greater relative risk of breast cancer. Less lifetime exposure to estrogen may help to keep down a womans risk of some types of breast cancer.
When women are pregnant, changes occur in the cells of the breast to prepare for breastfeeding. These changes can make the cells more resistant to cancer later in life. The earlier in life a woman experiences these changes, the greater protection she has against breast cancer. As a result, women are at lower risk of breast cancer if they:
- have children, particularly if they:
- have their children at an earlier age or
- have several children.
- Learn about the Indigenous Cancer Strategy II.
Common Risks For Breast Cancer
According to the National Cancer Institute below are the factors that increase a womens risk of getting breast cancer:
The strongest risk factor;for breast cancer is age. A womans risk of developing this disease increases as she gets older. The risk of breast cancer, however, is not the same for all women in a given age group. Research has shown that women with the following risk factors have an increased chance of developing breast cancer.
Genetic alterations : Inherited changes in certain genes increase the risk of breast cancer. These changes are estimated to account for no more than about 10 percent of all breast cancers. However, women who carry changes in these genes have a much higher risk of breast cancer than women who do not carry these changes.
Family history: A womans chance of developing breast cancer increases if her mother, sister, and/or daughter have been diagnosed with the disease, especially if they were diagnosed before age 50. Having a close male blood relative with breast cancer also increases a womans risk of developing the disease.
Personal history;of breast cancer: Women who have had breast cancer are more likely to develop a second breast cancer.
Alcohol: Studies indicate that the more alcohol a woman drinks, the greater her risk of breast cancer.
Long-term use of;menopausal hormone therapy: Women who used combined estrogen and progestin menopausal hormone therapy for more than 5 years have an increased chance of developing breast cancer.
Documented Risk Factors For Breast Cancer
Documented risk factors for breast cancer are shown in , arranged roughly in order of relative risk. Relative risk denotes the risk for an individual who is positive for a factor versus the risk for an individual who is negative for a factor. A relative risk of 1 indicates that there is no increased risk, whereas a relative risk of 10 indicates that there is a 10-fold increase in risk.
Table 1. RISK FACTORS FOR BREAST CANCER
* There is controversy over whether pathologic hyperplasia detected in breast biopsy samples is directly equivalent to cytologic hyperplasia detected in samples obtained through FNA or nipple aspiration.
Begg has suggested that these relative risks are subject to ascertainment bias and may overestimate the true risk associated with germline mutations in BRCA genes.
Age
One of the best-documented risk factors for breast cancer is age. As seen in , the incidence of breast cancer is extremely low before age 30 , after which it increases linearly until the age of 80, reaching a plateau of slightly less than 500 cases per 100,000. If all women less than 65 years of age are compared with women aged 65 or older, the relative risk of breast cancer associated with increased age is 5.8.
Figure 1. Breast cancer incidence as a function of age.
Lifestyle and Environmental Factors
Alcohol Consumption
Body Mass Index
Hormone Replacement Therapy
Radiation Exposure
Reproductive Factors
Prior History of Neoplastic Disease or Hyperplasia in the Breast
Hyperplasia
What Is The Brca Gene Mutation And Could I Carry It Slice
When it is functioning normally, BRCA is a gene that makes proteins to help repair damage to DNA and stop tumor growth. Mutations in BRCA1 and BRCA2 gene are inherited in families and can lead to an increased risk of certain cancers, including breast, ovarian, prostate, and pancreatic cancer, among others.
The gene can be inherited from either a personâs mother or their father. There are certain âred flagsâ in families that might make us worry about a BRCA mutation, including history of multiple different cancers, male breast cancer, ovarian cancer, or cancers diagnosed at a young age.
If indicated, testing for a BRCA mutation typically consists of a blood test. Results can be very important in determining the most appropriate cancer screening and methods to reduce cancer risk.
What Can I Do
Be proactive. Increasing your awareness and knowledge may help reduce your risk of developing breast cancer. Take action on your lifestyle risk factors. Know your body, watch for changes, and contact your health care provider with any questions or concerns about breast health and breast cancer prevention, early detection and screening.
What Are The Most Common Risk Factors For Breast Cancer
The following risk factors have the strongest evidence behind them and are recognized as clearly affecting breast cancer risk, for better or worse.
To see more risk factors, including possible risk factors that are currently under study, visit Susan G. Komens website. There are also lots of things that are rumored to increase breast cancer risk but have been shown by research not to. Susan G. Komen has a list of those factors too.
Who May Wish To Seek Assessment About Breast Cancer Risk
You might want to make an appointment to discuss your breast cancer risk if you:
- Have two first-degree relatives who were diagnosed with breast cancer
- Had an abnormal biopsy
- Have a family history of ovarian cancer or male breast cancer
- Were diagnosed with breast cancer before age 45
- Were diagnosed with two separate breast cancers
- Have a BRCA1 or BRCA2 gene mutation
- Have a blood relative with the BRCA1 or BRCA2 gene
- Are of Ashkenazi Jewish heritage
High Risk Breast Cancer Program

The High Risk Breast Cancer Program at Wake Forest Baptist Health provides breast cancer screening, chemoprevention and genetic risk evaluation for individuals at increased risk of breast cancer due to personal risk factors.
Our multidisciplinary team is comprised of specially trained physicians, genetic counselors and care coordinators who provide:
- Education
- Hereditary cancer risk assessment
- Genetic counseling and education about your risk of developing breast cancer
- Genetic testing to identify any genetic mutation that may lead to cancer or that may affect other members of your family
- Individualized cancer surveillance plan
- Prevention programs for people who are concerned about their personal and family history of breast cancer
Patients with the following risk factors may be referred to the program for genetic testing:
- Breast cancer diagnosis 50 years of age
- Bilateral breast cancer
- Breast cancer diagnosis plus any of the following in patient or close relative:
– Breast cancer in 2 relatives- Ovarian cancer- Ashkenazi Jewish ancestry
Patients with the following risk factors may be referred to the program for preventative services:;
- Positive genetic test result for a mutation associated with an inherited susceptibility to cancer
- Uninformative genetic test result but has a significant family history concerning for inherited susceptibility.
- Abnormal breast biopsy including atypical ductal hyperplasia , atypical lobular hyperplasia and lobular carcinoma