What’s Your Breast Cancer Risk: Tools That Includes Breast Density As Part Of Risk Calculation
Risk Assessment tools that include a patient’s dense tissue – an critical risk factor for breast cancer.
Having dense tissue is an independent risk factor for breast cancer. Calculating this risk, along with other risk factors, is designed to better predict a women’s risk of breast cancer. A three-tiered scale is used to determine lifetime risk – High , Intermediate and Average
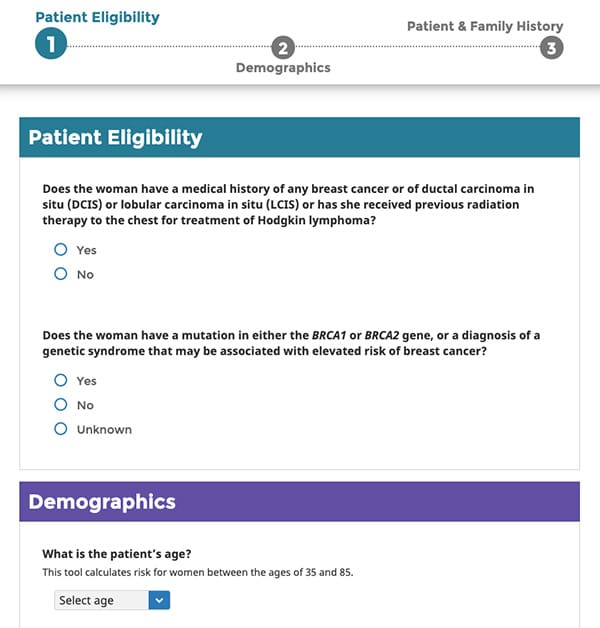
Breast Cancer Surveillance Consortium Risk Calculator
The Breast Cancer Surveillance Consortium Risk Calculator was developed and validated in 1.1 million women undergoing mammography across the United States, among whom 15,000 were diagnosed with invasive breast cancer. The BCSC Risk Calculator is an interactive tool designed by scientists that participate in the Breast Cancer Surveillance Consortium to estimate a woman’s five-year risk of developing invasive breast cancer. The tool includes as assessment of a patient’s breast tissue composition.
Risk Assessment Tool here
Tyrer-Cuzick Risk Assessment
The new version of the Tyrer-Cuzick Risk Assessment includes a patient’s breast tissue composition as part of the assessment. There are three inputs of breast density included in the risk assessment – the ACR 4th edition BI-RADS, the visual analogue scale and Volpara Density, an objective computer-based measure of breast density.
Link to the tool here.
| Back to Resources |
Younger Age At Menarche
Breast cancer risk increases by 5% for each year younger at menarche , a meta-analysis has shown. The association is stronger for oestrogen receptor -positive and progesterone receptor -positive tumours than for ER- and PR-negative tumours. Breast cancer risk may be higher in women whose breast development started at a younger age, a cohort study indicates.
Among BRCA1 mutation carriers too, breast cancer risk may be higher in those who are younger at menarche, a meta-analysis showed among BRCA2 carriers, breast cancer risk is not associated with age at menarche.
Who Is At High Risk For Early
According to the American Cancer Society , women who are at high risk for early-onset breast cancer include those who
- Have a known BRCA1 or BRCA2 gene mutation.
- Have a first-degree relative* , second-degree relative , or third-degree relative, which includes first cousins, with a BRCA1 or BRCA2 gene mutation.
- Have a lifetime risk of breast cancer of about 20% to 25% or greater, according to risk assessment tools that are based mainly on family history.
- Had radiation therapy to the chest between the ages of 10 and 30 years.
- Have Li-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome, or have first-degree relatives with one of these syndromes.
*Risk is higher with more than one affected first-degree relative and if the affected relative was diagnosed at a young age.
You May Like: What Does Breast Cancer Look Like On An Ultrasound
Benefits Of Mammographic Screening
The ACS systematic review also examined the effect of screening mammography on life expectancy. Although the review concluded that there was high-quality evidence that mammographic screening increases life expectancy by decreasing breast cancer mortality, the authors were not able to estimate the size of the increase 23.
Breast Cancer Risk Calculator Types
You can find several risk assessment calculators online there are at least seven or eight, according to Dr. Vincoff.
The one that we use in breast imaging is the one called Tyrer-Cusick Model Breast Cancer Risk Assessment, Dr. Vincoff says. And the reason why we use that one is that it goes back two generations of family history, whereas many just go back one generation. And it also includes enough factors like dense breast tissue, so that we can identify the patients that would most benefit from MRI.
Dr. Vincoff added that some risk calculators are meant to identify women who would benefit from genetic testing.
And that’s important, too. So, depending on who’s doing your risk calculation, you might be using a calculator that’s more geared towards genetic testing, or it could be geared toward women who have the type of breast where to catch cancer early, there needs to be something more than mammography starting at age 40.”
For some women, an MRI could be more effective in spotting cancer in its infancy, she says.
Also Check: What Are Some Warning Signs Of Breast Cancer
Clinical And Genetic Data
First-degree relatives with breast cancer **
Has the patient ever had a benign breast biopsy?
If so, has the patient been diagnosed with atypical hyperplasia?
Smoke
* If the patient did not have any children, complete with 0
** Include only mother, sisters and daughters
About this calculator
This calculator is based on a statistical model known as the Gail model, one of the oldest and well validated risk estimation models. The calculator estimates the 5-year risk of developing breast cancer, as well as the lifetime risk, assuming a life expectancy of 90 years.
The calculator has been validated in large populations of Caucasian women, as well as in populations of Black/African American, Hispanic, Asian and Pacific Islander women. Risk estimation in non-Caucasian women may be less accurate due to more limited data in these populations.
The calculator is only indicated for women with no history of breast cancer, lobular carcinoma in situ or ductal carcinoma in situ. In women with a personal history of breast cancer or known mutations in genes associated with hereditary breast cancer syndromes, other tools may be more appropriate.
About Gail Model Creator
Disclaimer
References
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Shairer C, Mulvihill JJ: Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 81:1879-86, 1989.
How To Measure Your Risk Of Breast Cancer
Every woman has some risk of breast cancer. In the U.S., 1 in 8 women will be diagnosed with invasive breast cancer over the course of her lifetime. This means the average womans breast cancer risk is 12-13%. A mans lifetime risk, by comparison, is much lower at 1 in 833 far less than 1%.
Just as there are factors that INCREASE the risk of breast cancer, there are ways to REDUCE your risk.
The starting point can be assessing YOUR PERSONAL RISK of breast cancer. Thankfully, there is a survey tool that can calculate a womans risk of developing breast cancer in her lifetime.
There are two breast cancer risk assessment tools that doctors use to calculate a womans risk of breast cancer:
- breast ultrasound
You May Like: What Does Metastatic Breast Cancer Look Like
Older Age At First Giving Birth
Breast cancer risk increases by 3% for each year older a woman is when she first gives birth, a meta-analysis showed. The association may be limited to ER/PR-positive tumours. ER/PR-positive breast cancer risk is 15% higher in women who first gave birth at an older age, compared with those who did so at a younger age, a meta-analysis showed. HER2-positive and triple-negative breast cancers are not associated with age at first birth.
Conversely among BRCA1 mutation carriers, breast cancer risk may be lower in those who are older at first birth, meta-analyses have shown among BRCA2 carriers, breast cancer risk is not associated with age at first birth.
Identifying Young Women With Increased Risk Of Hereditary Breast And Ovarian Cancer
Health care providers can play a critical role in helping to reduce the incidence of hereditary breast and ovarian cancer by identifying patients with elevated risk. The following guidelines can help identify young women who may have a higher risk for hereditary breast and ovarian cancer and detect early-onset breast cancer among these women.
Read Also: Who Is Considered High Risk For Breast Cancer
What Are The Breast Cancer Risk Factors That Impact Younger Women
There are traits that can elevate risk in younger women. We are learning that there are certain racial or ethnic groups that are definitely at higher risk, Dr. Vincoff says. We’ve come to understand over the course of the past few years that Black women in particular tend to develop breast cancer younger and that cancer is more aggressive. And they die younger of breast cancer, and more often from breast cancer. We’re trying to get that information out to Black women. Black women are a good example of where current, confusing guidelines arent serving them.
The other group in our community that we worry a lot about, are women of Ashkenazi Jewish heritage. And they’re also at increased risk for the very aggressive kinds of cancers, and for carrying the BRCA gene, Dr. Vincoff says.
Experts have also learned that having dense breasts can also raise risk.
Everybody’s breast tissue is very particular to them Dr. Vincoff explains. It’s like a fingerprint, and they have all different kinds of compositions. So, some people’s breasts are almost entirely fatty tissue, and some people’s breasts are what we call dense.”
Q8 I Am In The High Risk Category Does This Mean I Will Definitely Develop Breast Cancer
No, being high risk just means that when statistically compared to other women, your chances are higher, sometimes only slightly higher. It is completely understandable to be concerned about your high risk status, but early detection is our best tool against breast cancer. By identifying your risk, your doctors can provide you with a personalized screening plan and/or risk reduction options.
You May Like: How To Do Self Breast Examination For Cancer
Gail Model For Breast Cancer Risk
IMPORTANT
This calculator includes inputs based on race, which may or may not provide better estimates this calculator can be run with Race as Unknown, but users should know this defaults to the White option. Our evidence section reviews some of the issues with Race in this model. See here for more on our approach to addressing race and bias on MDCalc.
INSTRUCTIONS
The Gail Model is for use in women with no history of breast cancer, DCIS or LCIS. Other tools may be more appropriate for women with known mutations in BRCA1, BRCA2, or other hereditary syndromes associated with breast cancer. See the Evidence section for more information.
The Gail Model is one of several risk assessment models that can help determine the absolute 5 year risk and lifetime risk of developing breast cancer.
- Other models include the Tyrer-Cuzick model, the Claus model, BRCAPro, and BOADICEA .
It helps determine which risk-reduction optionsmedical , surgical or lifestyle changes onlyare most appropriate for individual patients by weighing risks and benefits of intervention versus likelihood of developing cancer.
Assessing The Risk Of Breast Cancer
In the United States, 279,100 new breast cancer cases were expected in 2020, making it the most prominent cancer risk followed by lung cancer and prostate cancer.
There are many factors to consider when assessing your lifetime risk of developing breast cancer, whether its in situ ductal carcinoma or invasive breast cancer.
A family history of breast cancer, especially among first-degree relatives , is one risk indicator. Usually, if you have a family history of breast cancer, its because of mutations in the BRCA1 and BRCA2 genes. These genes make proteins to help repair damaged DNA.
When variations called mutations occur in these genes, breast cancer is more likely to develop. If your parents have a mutation in either of these genes, youre also more likely to develop cancer at a younger age.
Surprisingly, men can also develop breast cancer, although it is not as common as it is for women. In men, BRCA1 and two mutations are also linked to prostate cancer.
While cancer isnt preventable, you can improve your chances for a positive outcome through early detectionan essential tool in fighting cancer.
Recommended Reading: What Is Grade 2 In Breast Cancer
What Are Screening Tests
Screening refers to tests and exams used to find a disease in people who dont have any symptoms. The goal of screening tests for breast cancer is to find it early, before it causes symptoms . Early detection means finding and diagnosing a disease earlier than if youd waited for symptoms to start.
Breast cancers found during screening exams are more likely to be smaller and less likely to have spread outside the breast. The size of a breast cancer and how far it has spread are some of the most important factors in predicting the prognosis of a woman with this disease.
Breast Cancer Screenings: Covered By Insurance
Many women and patients in general resist preventive care, such as routine medical screenings because of insurance costs. But Dr. Vincoff explains that in New York, a mammogram is paid for by most private insurers.
New York is a great place for breast cancer advocacy, and this is a significant advantage to being here, Dr. Vincoff says.
She says insurance covers mammograms annually starting at age 40, and that a baseline mammogram is covered in a womans 30s.
Even better, if you have dense breast tissue, New York requires a dense breast notification, says Dr. Vincoff. So, when you get your mammogram results, that letter that you get will tell you whether or not you have dense breasts. And if you do, you can have an ultrasound that will be paid for by your insurance, she says, adding that if you’re in that higher than 20 percent lifetime risk for developing breast cancer, your insurance will likely pay for you to have an MRI.
Read Also: Stage Four Metastatic Breast Cancer
Q9 I Am In The High Risk Category Is There Anything I Can Do To Reduce My Risk Of Being Diagnosed With Breast Cancer
You should speak with your doctor about your specific circumstances to determine if there is anything you can do to lower your risk. In some cases, your doctor may recommend lifestyle changes, and in higher risk cases, there are risk lowering drugs and interventional surgery options. It is important, however, that your doctor make the appropriate recommendations.
American Cancer Society Screening Recommendations For Women At Average Breast Cancer Risk
The COVID-19 pandemic initially resulted in most elective procedures being put on hold, leading to many people not getting screened for cancer. Learn how you can talk to your doctor and what steps you can take to plan, schedule, and get your regular cancer screenings in Cancer Screening & COVID-19.
These guidelines are for women at average risk for breast cancer. For screening purposes, a woman is considered to be at average risk if she doesnt have a personal history of breast cancer, a strong family history of breast cancer, or a genetic mutation known to increase risk of breast cancer , and has not had chest radiation therapy before the age of 30.
- Women between 40 and 44 have the option to start screening with a mammogram every year.
- Women 45 to 54 should get mammograms every year.
- Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
- All women should understand what to expect when getting a mammogram for breast cancer screening what the test can and cannot do.
Clinical breast exams are not recommended for breast cancer screening among average-risk women at any age.
Also Check: Why Do Women Get Breast Cancer
Factors That Affect Your Risk Of Breast Cancer
The following factors can affect your personal risk of breast cancer. Your physician will ask about these factors in helping you gauge your risk.
- Your age and family history of cancer
- Your personal history of breast cancer
- Prior radiation to chest or face
- Certain breast changes
- If and when you were pregnant and how many children you had
- Breastfeeding history
- Menstrual history, starting age and menopause age
- Using hormone replacements
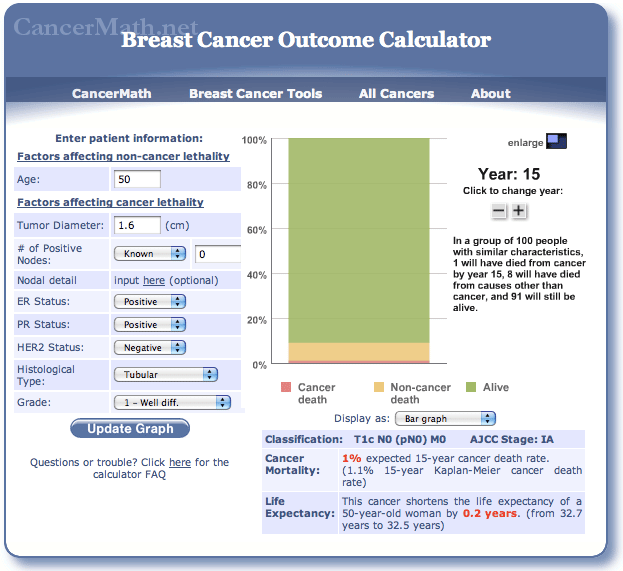
Prediction Models For Breast Cancer Risk
At Simmons Comprehensive Cancer Center, we use a variety of assessment tools designed to predict an individuals lifetime risk of developing breast cancer. Not all tools can be appropriately applied to all patients. Each tool is most effective when the patients characteristics and family history are similar to those of the study population on which the tool was based. Two such tools available at Simmons Cancer Center, which are widely used in research studies and clinical counseling, are known as the Gail model and the Claus model. Both have limitations, and the risk estimates derived from the two tools may differ for an individual patient.
The Gail Model
Designed by researchers at the National Cancer Institute and the National Surgical Adjuvant Breast and Bowel Project, the Gail model is primarily focused on personal risk factors for breast cancer and estimates the patients five-year and lifetime risk of breast cancer. The five-year risk can be used for chemoprevention recommendations if the risk is greater than 1.67 percent. The Gail model considers the following factors:
- Age at which patient has her first menstrual period
- Age at which patient delivers her first live birth
- Patients number of biopsies
- Patients history of atypical hyperplasia
- The number of first-degree female relatives with breast cancer
The Claus Model
Recommended Reading: Why Does Dense Breast Tissue Increase Cancer Risk
Other Risk Assessment Tools
Other risk assessment tools are more appropriate for women who have a history of certain medical conditions. Below is a list of alternative resources for women with a medical history of:
Breast Cancer or Lobular Carcinoma in Situ or Ductal Carcinoma in Situ
- Women with a history of breast cancer have risks of recurrence that depend on the type of breast cancer, its stage at diagnosis, and treatment. A cancer doctor can provide guidance on future risks for breast cancer survivors.
- Women with a history of DCIS have risk of invasive breast cancer that depends on type of treatment for DCIS a cancer doctor can provide information on this risk.
- Women with a history of LCIS can use the IBIS Breast Cancer Risk Evaluation Tool to estimate the risk of invasive breast cancer or DCIS. A cancer doctor can also provide information on the risk.
Treatment with Radiation to the Chest
- Women who received radiation for the treatment of Hodgkin lymphoma have higher than average risk of breast cancer. These risks are discussed in the scientific manuscript Travis, L.B et al. .
A Known Mutation in Either the BRCA1 or BRCA2 Gene
- Women with a known mutation in either the BRCA1 or BRCA2 gene can use the BOADICEA model to estimate their breast cancer risk.
Other Rare Breast Cancer-Causing Syndromes, such as Li-Fraumeni Syndrome
- Women with a known or suspected inherited breast cancer-causing syndrome should consult a specialist in medical genetics.