Prognosis Of Late Vs Early Cancer Recurrence
Late recurrence is associated with a better prognosis than early recurrence in estrogen receptor-positive breast cancer. A 2018 study in Clinical Breast Cancer found that survival after recurrence was significantly longer in people with a late versus early recurrence . In this study, the lungs were the most common site of late distant recurrence.
What Are The Signs Of Breast Cancer Recurrence
If you have a local recurrence or new primary breast cancer, you may find symptoms similar to an initial breast cancer. This includes:
- A new lump in the breast, armpit area or around the collarbone
- A change in breast size or shape
- Changes to the nipple, such as sores or crusting, an ulcer or inverted nipple
- Clear or bloody nipple discharge
- Changes to the skin including redness, puckering or dimpling
- Breast tenderness or pain
If your breast cancer has spread to other parts to the body, known as distant recurrence, there are a number of possible symptoms, including:
- Unexpected weight loss or change in appetite
- Severe or ongoing headaches
However, symptoms will vary depending on where the secondary cancer presents, and some primary and secondary cancers may not present any obvious symptoms. Sometimes recurrence is identified on a scan or blood test that was done for a reason other than breast cancer.
If you have any health concerns or symptoms that are new or persistent, speak with you GP or treating physician.
Microsurgery Can Help Reduce The Risk Of Lymphedema After Breast Cancer Surgery
Developing lymphedema painful swelling in the arm, underarm, hand, chest, abdomen, or back after breast cancer has traditionally been viewed as a risk worth taking to undergo breast cancer surgery.
Even in skilled surgical hands, about 30% of patients develop lymphedema after lymph node dissection, in which 5-30 lymph nodes are removed during cancer surgery and analyzed for signs that the cancer has spread beyond the breast.
Lymphedema can change how a patient looks and feels about their body on top of the physical and emotional challenges of breast cancer treatment. But an advanced procedure called immediate lymphatic reconstruction can reduce the risk of developing lymphedema by 20% or more.
ILR is a microsurgery performed by a plastic surgeon right after mastectomy is complete. Using a microscope and fluorescein a dye that illuminates the 0.5mm-wide lymphatic vessels we can differentiate between the vessels that drain the breast and those that drain the underarm and reroute the flow of lymphatic fluid to be filtered out of the body.
Research has shown that fewer than 10% of patients develop lymphedema within five years after ILR. Working together with UT Southwesterns Breast Cancer team, the Plastic Surgery team offers this advanced and effective procedure to treat lymphedema and reduce the risk of its recurrence.
You May Like: Are There Signs Of Breast Cancer
What Women Can Do Themselves
There are some things women can do themselves to lower their risk of late recurrence:
- Regular exercise is associated with a lower risk of death from breast cancer as well as death from all causes.
- It’s important for everyone to have their vitamin D level tested, although the role of vitamin D is still uncertain. Vitamin D deficiency is associated with bone loss, a concern for most people who have coped with breast cancer.
- Losing weight if you are overweight, or maintaining a healthy weight is important as well.
Can Tamoxifen Reduce Recurrence Risk

Recurrence risk factors. The recurrence risk can be lowered during therapy with tamoxifen or aromatase inhibitors and also by simple lifestyle changes such as a balanced and healthy diet, regular exercise, no smoking or excessive drinking. Breast cancer survivors are recommended regular mammograms, if possible by 3D in addition to
Don’t Miss: What Types Of Breast Cancer Are There
Lisa Fought Breast Cancer For 8 Years Heres Her Story
In contrast to the common belief that surviving for five years after cancer treatment is equivalent to a cure, with hormone-sensitive breast tumors there is a steady rate of recurrence risk for at least 20 years after the original diagnosis, even with very small node-negative tumors.
Overall, the chance that an estrogen receptor-positive tumor will recur between five years and 20 years after diagnosis ranges from 10% to over 41%, and people with these tumors remain at risk for the remainder of their lives.
An awareness of the risk of late recurrence is important for a number of reasons. People are often shocked to learn that their breast cancer has come back after say, 15 years, and loved ones who don’t understand this risk are often less likely to be supportive as you cope with the fear of recurrence.
While chemotherapy has little effect on the risk of late recurrence hormonal therapy does, and estimating this risk may help determine who should receive extended hormonal therapy . Finally, late recurrences can differ from early relapse with regard to sites of metastases and survival.
Factors such as initial tumor size, number of nodes involved, and receptor status play into the risk of late recurrence, but tumor biology appears to have the greatest effect, and research is actively looking for ways to look at gene expression and copy number to predict risk.
Protect Against Potential Breast Cancer Recurrences
If youve had breast cancer before, there is a small chance you can get it again. However, you can put some preventative measures in place.
Practice holistic health care by eating well, exercising, getting plenty of sleep, and caring for your emotional well-being, including practices to help manage your fear and pervasive worry about relapse.
You can assess your risk of cancer or cancer recurrence by taking ezras know-your-risk quiz, which evaluates questions about your lifestyle and medical history.
Your score will highlight areas where you can improve your own health care and lifestyle.
Most importantly, see your oncologist for regular checkups, self-examine your breasts carefully and consistently, schedule an annual MRI screening, and have a yearly mammogram.
To learn more about mammograms, please check out:
Recommended Reading: What Are Symptoms Of Breast Cancer Other Than Lumps
What This Means For You
If youve been diagnosed with early-stage breast cancer, your doctor may recommend treatments after surgery to reduce your risk of recurrence.
If you were diagnosed with hormone receptor-positive, early-stage breast cancer, its likely that your doctor will recommend you take some type of hormonal therapy medicine either tamoxifen or an aromatase inhibitor depending on your menopausal status for five to 10 years after surgery.
Chemotherapy after surgery is usually completed in three to six months. If youre also receiving a targeted therapy, such as Herceptin , with chemotherapy, you may continue to receive the targeted therapy for up to a year after completing chemotherapy.
Radiation therapy after surgery can be completed in one to seven weeks.
So, hormonal therapy after surgery takes the longest to complete. Hormonal therapy medicines also can cause troubling side effects, such as hot flashes, night sweats, and joint pain. Less common but more severe side effects include heart problems and blood clots.
Research has shown that about 25% of women who are prescribed hormonal therapy to reduce the risk of recurrence after surgery either dont start taking the medicine or stop taking it early, in many cases because of side effects.
Learn more about Staying on Track With Treatment. You can read about why its so important to stick to your treatment plan, as well as ways to manage side effects after radiation, chemotherapy, and hormonal therapy.
Who Is At Risk Of Breast Cancer Recurrence
Everyone who has received a breast cancer diagnosis is at risk of recurrence, however the risk differs markedly depending on a number of factors listed below. Some breast cancers, when diagnosed very early when small and without lymph node involvement, have an excellent prognosis and are very unlikely to recur. On the contrary, larger cancers, with lymph node involvement or with a more invasive behaviour, are unfortunately at a higher risk of recurrence.
Don’t Miss: Stage 4 Breast Cancer Symptoms
Local Breast Cancer Recurrence
Breast cancer can return to the same area where it first appeared, Lange says. In this case, your doctor will base a treatment approach on how the first cancer was addressed.
If the original tumor was treated with lumpectomy and radiation, many patients may then need a bigger surgery, such as mastectomy, for the purpose of local control, she explains. If the original tumor was treated with mastectomy, then local resection of the recurrence should be considered. This is often followed by radiation therapy to the resection site.
Lange says an oncologist will evaluate a patient with recurrent breast cancer. Based on characteristics of the cancer cells and how they are behaving, the oncologist might recommend chemotherapy, hormonal therapy or a combination of treatments. For some patients, clinical trials of new therapies may be available.
Can Hormone Receptor Positive Breast Cancer Come Back
If youve been diagnosed with hormone-receptor-positive breast cancer and will be taking hormonal therapy after surgery and other treatments, its very important that you take the medicine for as long as its prescribed and at the dose at which it is prescribed. Hormone-receptor-positive breast cancer can come back, and hormonal therapy after surgery reduces that risk you must remember that.
Also Check: Where Can You Get Breast Cancer Lumps
If All The Cancer Was Removed With Surgery Why Do I Need Any Additional Treatment
It has long been recognized that breast cancer is not always cured by locoregional treatment alone.
The goal of treating early breast cancer is to remove the cancer and keep it from coming back . Most people diagnosed with breast cancer will never have a breast cancer recurrence. However, everyone who has had breast cancer is at potential risk of recurrence, and that is why in most cases, there is a recommendation for treatment in addition to surgery, which is known as adjuvant therapy. The risk of recurrence can never be entirely eliminated, but the aim of adjuvant therapy is to reduce recurrence risk to the absolute minimum.
How Long Does It Take For Breast Cancer To Recur

If doctors knew the specific risk of distant recurrence of a breast cancer after 5 years of hormonal therapy, it could help decide whether to extend hormonal therapy to 10 years. A study suggests that after 5 years of hormonal therapy, the risk of distant recurrence is still sizable, even 20 years after the initial diagnosis.
Recommended Reading: What Is De Novo Metastatic Breast Cancer
Maintain A Healthy Body Weight
Maintaining a healthy weight appears to lower the risk of breast cancer recurrence. If you’ve been frustrated in attempts to lose weight in the past, it may be encouraging to know that some other practices on this list are associated with weight loss, not just exercise, but intermittent fasting, and even upping the fiber in your diet to improve the diversity of the bacteria in your gut.
Risk Of Late Recurrence Is Underestimated
A survey led by the Canadian Breast Cancer Network found that women often underestimate their risk of late recurrence. In the survey, only 10% were aware of the risk of recurrence after five years of tamoxifen therapy, and 40% felt that they were cured after hitting the five-year mark.
Many breast cancer survivors underestimate their risk of late recurrence.
Recommended Reading: What Percentage Of Breast Cancer Is Metastatic
How Does Distant Recurrence Occur
Many patients find it hard to understand how they can be apparently cancer free one day and be diagnosed with recurrent cancer the next. If surgery got all of the cancer out and chemotherapy and radiation were supposed to have mopped up the rest, how can recurrence even happen?
In most cases, even the smallest breast cancer detected has been growing for some time before it was caught. During this period of growth, the cancer cells multiplied and divided over and over again, and some cancer cells may splinter off from the main tumour and escaped into the surrounding blood and lymphatic vessels. Cells that spread to lymph nodes can certainly be trapped in those lymph nodes and removed at the time of surgery, but cells can also go into the circulatory system. Even early-stage cancers that originally had no lymph node involvement can recur and develop metastatic disease.
While its less common, cancer cells can bypass lymphatics and lymph nodes and travel via surrounding blood vessels. Cancer cells can continue to circulate and go anywhere the blood vessels will take them, or they can home in on other organs in the body, where they take up residence and continue to grow and divide in that one particular spot.
If and when cancer comes back, the cancer cells that escaped the breast are to blame. Obviously if your recurrence is ten years after your diagnosis, we assume that the cells have been dormant all that time and missed the treatments aimed at dividing cells.
Treatments And Recurrence: Early And Late
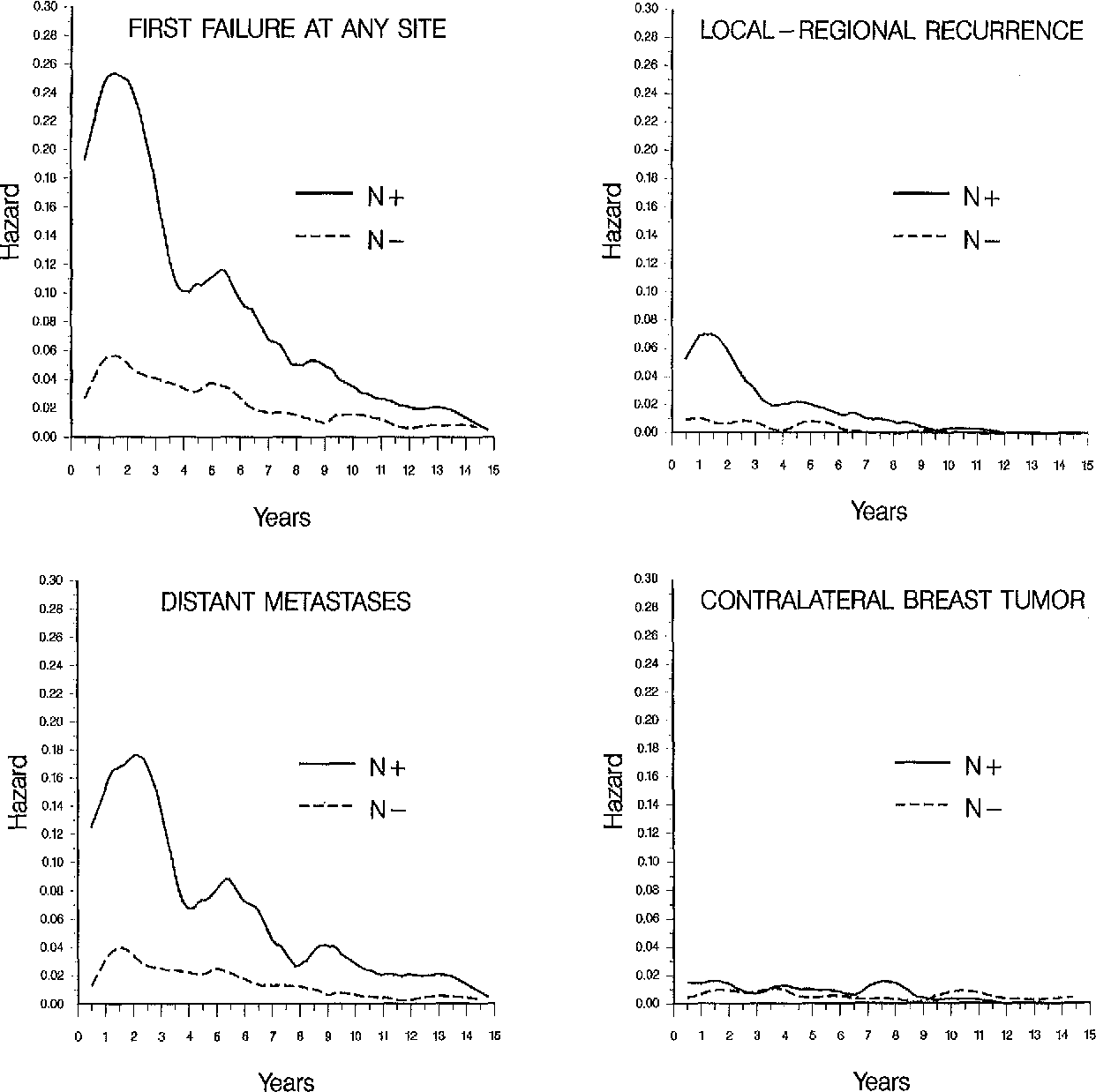
Treatments also play a role in both early and late recurrences. While chemotherapy can significantly reduce the risk of recurrence in the first five years, it has much less influence on the risk of late recurrence.
Hormonal therapy reduces the risk of recurrence in the first five years , but can also reduce the risk of late recurrences. It is this reduction in risk that has led to recommendations to extend hormonal therapy for people at high risk beyond five years.
Extending hormonal therapy from five years to 10 years has been shown to reduce the risk of late recurrence, but the risk of recurrence needs to be weighed against the side effects of continued therapy.
A 2019 study found that people with luminal A tumors continued to have significant benefit from tamoxifen therapy for 15 years post-diagnosis.
The addition of bisphosphonates to an aromatase inhibitor in post-menopausal women with early-stage breast cancer may improve survival, but it’s too early to determine the effect on late recurrences. Bisphosphonates reduce the risk of bone metastases, but the most common sites of distant late recurrence are the brain, liver, and lungs.
Also Check: Best Gifts For Breast Cancer Patients
Check On Whether You Need Medications
After you complete your cancer treatment, if you have a high chance of your cancer returning, your doctor may prescribe you certain drugs to reduce your risk.
Tamoxifen and raloxifene are two such drugs. These drugs are approved for use in the U.S. and doctors usually prescribe them to lower the chances of estrogen-related breast cancer. Both drugs block estrogen hormone in breast cells. Studies show that they reduce your chances of getting breast cancer again by about 40%.
Tamoxifen. You take this once a day by mouth as a pill or liquid. It may make it less likely for you to get cancer in parts of your breast that werenât affected earlier. You may have side effects like hot flashes, vaginal discharge, irregular periods, loss of sexual interest, memory loss, fatigue, and joint pain.
Raloxifene. Itâs a pill you take once a day. Itâs usually given to women who are post-menopausal — those who stopped having their periods. It may also help you avoid or treat osteoporosis, when your bone density thins, putting you at risk of fractures.
While rare, these drugs can also cause blood clots in your leg veins or lungs. This can be a serious side effect that may need immediate medical attention. Contact your doctor as soon as possible if you think you have a blood clot.
Side effects can include vaginal discharge, muscle and joint pain, hot flashes, and night sweats. These drugs may also speed up osteoporosis and may raise your cholesterol.
If Cancer Comes Back In The Same Breast
If the breast cancer comes back in the same breast it’s called local recurrence. The cancer might be picked up at one of your follow up scans or appointments. Or you might notice your breast or scar looks or feels different.
Symptoms of local recurrence can include:
- a small pink or red lump called a nodule on the breast or scar
- change in shape or size of the breast
- a swelling in your arm or hand on the side of your breast surgery
- changes in the shape or position of the nipple
- redness or a rash on the skin on or around the breast area
- a lump or thickening in the breast
Let your doctor know as soon as you can if you notice any changes. You usually have tests to check if the cancer has come back.
Recommended Reading: What To Say To Breast Cancer Patient
What Is The Risk For Breast Cancer Recurrence
The risk of recurrence depends on the type of breast cancer and its stage. Timing matters, too: The highest risk of recurrence for breast cancer patients is during the first few years after treatment.
At the Johns Hopkins Breast Center, our team of breast cancer specialists monitors patients who are at risk of recurrence, Lange explains. The follow-up schedule depends on the stage of cancer, what kind of treatment has been received and prognostic factors. The risk of recurrence decreases as time goes on, but never gets down to zero.
Eat A Wide Variety Of Healthy Foods
According to a 2017 review of studies to date, people with breast cancer who eat a diet rich in vegetables, fruits, whole grains, fish, and poultry have better survival rates. There are many phytonutrients in the foods we eat, several of which have anti-cancer properties. That said, it’s likely that the combination of nutrients found in these foods that’s key, rather than any particular food.
To understand this, it helps to realize that cancer cells are “smart.” Unlike the popular conception of cancer, tumors are not unchanging clones of cells, but continually develop new mutations. Some of these mutations help a tumor grow. Some help a tumor avoid death . Others help a tumor spread, or suppress the body’s attempt to eliminate the cells . Just as tumor cells have many ways to continue their growth , a combination of healthy nutrients gives us the best opportunity to stay as healthy as possible.
Don’t Miss: Life Expectancy For Metastatic Breast Cancer