Should I Go For Breast Screening
Its important that you have access to enough information about the benefits and harms of breast screening to make the decision.
You can talk to your own doctor or nurse. Or you can contact the Cancer Research UK nurses on freephone 0808 800 4040. The lines are open from 9am to 5pm, Monday to Friday.
What Are The Risk Factors For Developing Breast Cancer
Factors that can increase the risk of developing breast cancer include women with a personal history of, or one or more first-degree relatives diagnosed with, breast or ovarian cancer women who are carriers of gene mutations, such as BRCA1 or BRCA2, or have a first-degree relative with these gene mutations and women who have had chest radiation therapy before age 30 or within the past eight years.
Women with these risk factors are considered high risk and may be encouraged to start screening earlier and more frequently.
Increasingly, breast density is being recognized as a significant risk factor. Dense breast tissue refers to how it appears on the mammogram based on the mix of fatty and fibrous tissue. Women with very dense breasts may require a more personalized screening approach than what is recommended for the general population. This may include both mammography and ultrasound exams.
While the recommendations differ and can be confusing, the ultimate decision rests with women. Understanding the risks and benefits of regular mammogram screening and speaking with your doctor about your medical history, is an important first step to decide whats right for you.
Mayfair Diagnostics has 11 locations which offer mammography exams, including Mahogany Village, Market Mall, Mayfair Place, and Southcentre locations which have the new Pristina mammography system which helps provide a more comfortable mammogram. Visit our breast imaging page for more information.
REFERENCES
Breast Cancer Risk Factors
Everyone wants to know what they can do to lower their risk of breast cancer. Some of the factors associated with breast cancer being a woman, your age, and your genetics, for example can’t be changed. Other factors being overweight, lack of exercise, smoking cigarettes, and eating unhealthy food can be changed by making choices. By choosing the healthiest lifestyle options possible, you can empower yourself and make sure your breast cancer risk is as low as possible.
The known risk factors for breast cancer are listed below. Click on each link to learn more about the risk factor and ways you can minimize it in your own life. If a factor can’t be changed , you can learn about protective steps you can take that can help keep your risk as low as possible.
Just being a woman is the biggest risk factor for developing breast cancer. There are about 266,120 new cases of invasive breast cancer and 63,960 cases of non-invasive breast cancer this year in American women.
As with many other diseases, your risk of breast cancer goes up as you get older. About two out of three invasive breast cancers are found in women 55 or older.
Women with close relatives who’ve been diagnosed with breast cancer have a higher risk of developing the disease. If you’ve had one first-degree female relative diagnosed with breast cancer, your risk is doubled.
About 5% to 10% of breast cancers are thought to be hereditary, caused by abnormal genes passed from parent to child.
Also Check: Stage Three Breast Cancer Prognosis
If You Have A Normal Result
You will receive a letter to let you know your mammogram does not show any signs of cancer. Your next screening appointment will be in 3 years time. Do contact your GP or local screening unit if you havent received an appointment and think you are due one.
It is important to see your GP If you notice any symptoms between your screening mammograms.
Breast Changes Of Concern

Some breast changes can be felt by a woman or her health care provider, but most can be detected only during an imaging procedure such as a mammogram, MRI, or ultrasound. Whether a breast change was found by your doctor or you noticed a change, its important to follow up with your doctor to have the change checked and properly diagnosed.
Check with your health care provider if your breast looks or feels different, or if you notice one of these symptoms:
- Lump or firm feeling in your breast or under your arm. Lumps come in different shapes and sizes. Normal breast tissue can sometimes feel lumpy. Doing breast self-exams can help you learn how your breasts normally feel and make it easier to notice and find any changes, but breast self-exams are not a substitute for mammograms.
- Nipple changes or discharge. Nipple discharge may be different colors or textures. It can be caused by birth control pills, some medicines, and infections. But because it can also be a sign of cancer, it should always be checked.
- Skin that is itchy, red, scaled, dimpled or puckered
Also Check: Can Getting Hit In The Breast Cause Cancer
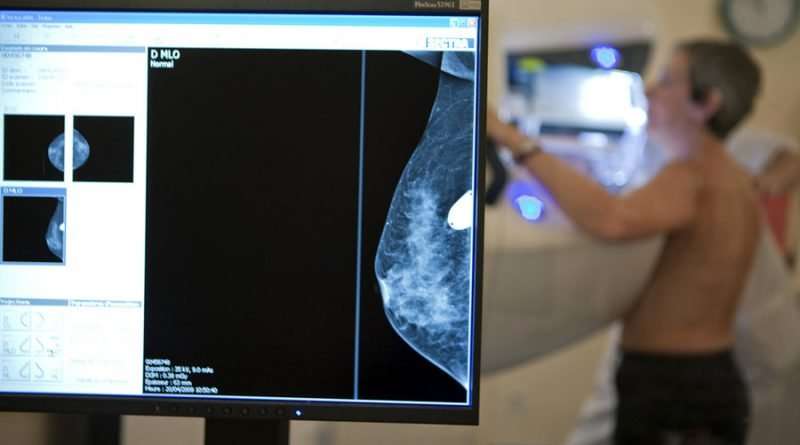
Why Do I Need A Mammogram
Mammograms are done as part of a regular physical exam to provide a baseline reference or to check any unusual changes in the breast. Itâs the best screening test for lowering the risk of dying from breast cancer.
A mammogram can help your health care provider decide if a lump, growth, or change in your breast needs more testing. The mammogram also looks for lumps that are too small to feel during a physical exam.
Myth #: I Dont Have Any Symptoms Of Breast Cancer Or A Family History So I Dont Need To Worry About Having An Annual Mammogram
Fact: The American College of Radiology recommends annual screening mammograms for all women over 40, regardless of symptoms or family history. Early detection is critical, says Dr. Sarah Zeb. If you wait to have a mammogram until you have symptoms of breast cancer, such as a lump or discharge, at that point the cancer may be more advanced . According to the American Cancer Society, early-stage breast cancer has a five-year survival rate of 99 percent. Later-stage cancer has a survival rates of 27 percent.
More than 75 percent of women who have breast cancer have no family history.
You May Like: Stage 3 Lymph Node Cancer
What Does A Suspicious Area Look Like On A Mammogram
- A lump or mass with a smooth, well-defined border usually isnât cancerous. An ultrasound can look inside the lump. If itâs filled with fluid, itâs called a cyst, and itâs usually not cancer, but your doctor might recommend a biopsy.
- A lump that has an irregular border or a starburst appearance raises more concern. A biopsy is usually recommended.
- Deposits of calcium can be large or small, and they might or might not be cancerous. If the deposits are very small, you may need more tests and a biopsy.
Having A Family History Of Breast Cancer
Its important to note that most women who get breast cancer do not have a family history of the disease. But women who have close blood relatives with breast cancer have a higher risk:
- Having a first-degree relative with breast cancer almost doubles a womans risk. Having 2 first-degree relatives increases her risk by about 3-fold.
- Women with a father or brother who has had breast cancer also have a higher risk of breast cancer.
Don’t Miss: Malignant Neoplasm Of Breast Definition
Can A Mole On Your Breast Or Nipple Turn Into Cancer
Moles anywhere on your body can become malignant. That includes moles on your breasts and nipples.
Cancerous moles are a symptom of melanoma, the most common type of skin cancer. In most cases, melanomas can be removed safely, noninvasively, and before the cancer cells have spread.
Having a melanoma on your breast is not the same as having breast cancer, which typically involves a lump or tumor. Follow-up for melanoma removal rarely involves chemotherapy, radiation, or biologic drugs that are usually part of a breast cancer treatment plan.
How Often Should Women Ages 50
The American Cancer Society recommends mammography every year for women ages 50-54 and every 1-2 years for women ages 55 and older .
The NCCN recommends women 50-69 have mammograms every year .
The U.S. Preventive Services Task Force recommends mammography every 2 years for women 50-69 . The Task Force reviewed the scientific evidence and concluded mammography every 2 years gives almost as much benefit as mammography every year while reducing risks . These risks include
You May Like: Stage 3 Ductal Carcinoma Prognosis
Role Of The Funding Source
This research was funded by Agency for Healthcare Research and Quality under a contract to support the work of the United States Preventive Services Task Force and by the National Cancer Institute. Investigators worked with USPSTF members and AHRQ staff to develop the scope, analytic framework, and key questions. The funding source had no role in study selection, quality assessment, or data synthesis. AHRQ staff provided project oversight and reviewed the report to ensure that the analysis met methodological standards. The investigators are solely responsible for the content and the decision to submit the manuscript for publication.
Inheriting Certain Gene Changes
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene changes passed on from a parent.
BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of these genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has up to a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer.
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts.
- Women with one of these gene changes also have a higher risk of developing ovarian cancer and some other cancers.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi origin than in other racial and ethnic groups, but anyone can have them.
Other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
Inherited mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Recommended Reading: Breast Cancer Nodes
Risks Of Screening Mammograms
For most women aged over 50 the benefits of regular mammograms outweigh any risks.
The risks of a mammogram are:
- exposure to a low dose of radiation from x-rays
- a result suggesting a possible cancer that is found to be wrong by follow-up testing . False positive mammograms can be caused by scar tissue, cysts or dense breast tissue
- a false negative result that is, breast cancer was present but not found
- a breast cancer is found and treated that may not have become life threatening. It is not possible to be sure which breast cancers may become life-threatening and which breast cancers may not
Radiation Exposure Simulation Model
Full details including approach, data sources, and assumptions are available in the Supplemental Content. Briefly, for each of the eight screening strategies, we simulated woman-level factors and screening-related events for 100,000 women.
Woman-level factors
Each woman was assigned a compressed breast thickness from the DMIST distribution . Women with a compressed breast thickness of 7.5 cm or larger were assumed to have large breasts requiring extra views for complete examination. Based on distributions observed in the BCSC, each woman was assigned a baseline Breast Imaging-Reporting and Data System density at the start of screening, which could potentially decrease by one category at ages 50 and 65 years .
Evaluation of a positive screening exam
Screening mammography process. Short interval follow-up examinations included unilateral, diagnostic views on the recalled breast at 6 months after the initial SIFU recommendation, and both unilateral, diagnostic views on the recalled breast plus bilateral routine screening views at 12 and 24 months after the initial SIFU recommendation for annual screeners and 24 months after the initial SIFU recommendation for biennial screeners. The routine screening views could result in recall for additional imaging to work up a new finding, followed by a recommendation for another SIFU examination, or tissue biopsy.
Radiation dose
Recommended Reading: Is Weight Gain A Symptom Of Breast Cancer
How Well Do Mammograms Work
These imaging tests help doctors diagnose about 75% to 85% of breast cancers. Detection rates get better as a woman ages, because breasts become less dense with age. This makes tissue easier to see through on mammograms.
Advancing technology raises detection rates. One study showed that using 3D mammography along with digital mammograms improved detection rates and lowered the number of women who had to return for more tests because of a suspicious finding.
So Mammograms Work But Theyre Not Perfect What Exactly Is The Problem
There are a couple of them, actually.
Mammography works, but itâs a blunt tool â and itâs also a little fickle. Sometimes it doesnât work well enough â it may miss tumors hidden within dense breast tissue . Other times, it works too well: identifying âcancersâ that may never come to fruition.
âYes, if you go into screening, thereâs a chance that youâll have a low-risk cancer diagnosed,â said Fred Hutchâs Dr. Ruth Etzioni, a biostatistician and national expert on cancer screening who helped created the ACSâs recent breast screening guidelines. âThat is a possibility. But if you have a low-risk cancer diagnosed, a cancer that doesnât need to be treated, that doesnât mean screening doesnât work for someone else. We know thereâs such a thing as overdiagnosis, but it doesnât mean screening doesnât work.
âTheyâre different sides of the coin,â she said. âItâs a flaw, but itâs not a flaw in mammography. Itâs a flaw in the endeavor to detect cancer early.â
Rahbar summoned the classic baby-with-the-bathwater analogy.
âJust because itâs clear we have overdiagnosis doesnât mean we should throw out an effective tool that decreases breast cancer-related deaths,â he said.
Also Check: Third Stage Breast Cancer
The Effect Of Screening On Total Mortality
Breast cancer mortality is the wrong outcome. Not only because it is biased in favour of screening but also because the treatment of overdiagnosed, healthy women increases their risk of dying. Radiotherapy, for example, may cause deaths from heart disease, lung cancer and other cancers, and these iatrogenic deaths are not counted as breast cancer deaths.
Figure 3 shows the effect of invitations to screening under three overly optimistic and partly erroneous assumptions: screening reduces breast cancer mortality by 20% screening does not increase mortality from other causes and assessment of cause of death is not biased.20 The effect of screening on total mortality is barely visible.
Cumulative risk of dying according to age for women invited to screening from age 50 years and for women who are not invited assuming screening reduces breast cancer mortality by 20% and does not increase deaths from other causes. Based on data for England and Wales for 2009 from Office for National Statistics. Reproduced with permission from Paul Pharoah.
Spot Compression Spot Compression May Be Used To Get A Closer View Of One Area Of The Breast During Diagnostic Mammography
To get a clearer image, a small compression plate separates the breast tissue in an area and pushes normal breast tissue out of the way. The images may be enlarged to make it easier to see small suspicious areas.
These close-up views can show tiny deposits of calcium that look like small white spots on a mammogram. The radiologist looks at the size, shape and pattern of calcifications and reports these as part of the results of the mammography.
Most are not related to cancer. However, certain characteristics of calcifications, such as irregular shapes or certain groupings, can be a concern.
Recommended Reading: Estrogen Positive Breast Cancer Survival
Reproductive History Estrogen Is The Main Hormone Associated With Breast Cancer Estrogen Affects The Growth Of Breast Cells Experts Believe That It Plays An Important Role In The Growth Of Breast Cancer Cells As Well The Type Of Exposure And How Long Cells Are Exposed To Estrogen Affects The Chances That Breast Cancer Will Develop
Early menarche
The start of menstruation is called menarche. Early menarche is when menstruation starts at an early age . Starting your period early means that your cells are exposed to estrogen and other hormones for a greater amount of time. This increases the risk of breast cancer.
Late menopause
Menopause occurs as the ovaries stop making hormones and the level of hormones in the body drops. This causes a woman to stop menstruating. If you enter menopause at a later age , it means that your cells are exposed to estrogen and other hormones for a greater amount of time. This increases the risk for breast cancer. Likewise, menopause at a younger age decreases the length of time breast tissue is exposed to estrogen and other hormones. Early menopause is linked with a lower risk of breast cancer.
Late pregnancy or no pregnancies
Pregnancy interrupts the exposure of breast cells to circulating estrogen. It also lowers the total number of menstrual cycles a woman has in her lifetime.
Women who have their first full-term pregnancy after the age of 30 have a slightly higher risk of breast cancer than women who have at least one full-term pregnancy at an earlier age. Becoming pregnant at an early age reduces breast cancer risk.
The more children a woman has, the greater the protection against breast cancer. Not becoming pregnant at all increases the risk for breast cancer.