Autosomal Dominant Inheritance Of Breast And Gynecologic Cancer Predisposition
Autosomal dominant inheritance of breast and gynecologic cancers is characterized by transmission ofcancer predisposition from generation to generation, through either the mothers or the fathersside of the family, with the following characteristics:
- Inheritance risk of 50%. When a parent carries an autosomal dominant genetic predisposition, each child has a 50:50 chance of inheriting the predisposition. Although the risk of inheriting the predisposition is 50%, not everyone with the predisposition will develop cancer because of incomplete penetrance and/or gender-restricted or gender-related expression.
- Both males and females can inherit and transmit an autosomal dominant cancer predisposition. A male who inherits a cancer predisposition can stillpass the altered gene on to his sons and daughters.
Germline pathogenic variants in the genes responsible for these autosomal dominant cancer syndromes produce different clinical phenotypes of characteristic malignancies and, in some instances, associated nonmalignant abnormalities.
The family characteristics that suggest hereditary cancer predisposition include the following:
Figure 1 and Figure 2 depict some of the classic inheritance features of a BRCA1 and BRCA2 pathogenic variant, respectively. Figure 3 depicts a classic family with Lynch syndrome.
| % risk of carrying MLH1, MSH2, MSH6 pathogenic variant |
Brca1 And Brca2 Genetic Mutations
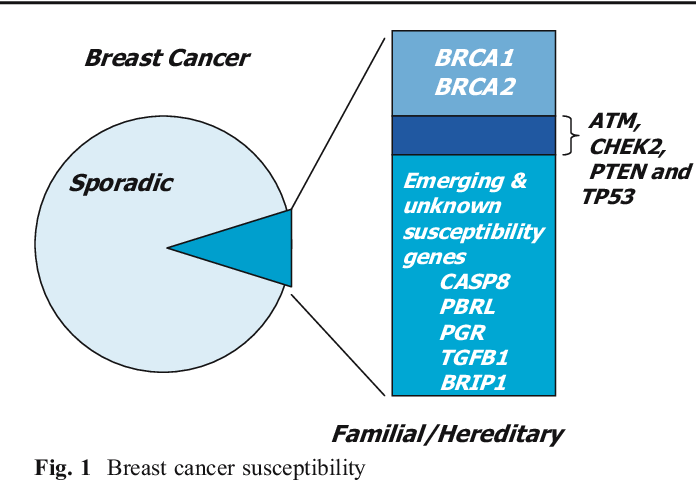
Most inherited cases of breast cancer are associated with mutations in two genes: BRCA1 and BRCA2 .
Everyone has BRCA1 and BRCA2 genes. The function of the BRCA genes is to repair cell damage and keep breast, ovarian, and other cells growing normally. But when these genes contain mutations that are passed from generation to generation, the genes don’t function normally and breast, ovarian, and other cancer risk increases. BRCA1 and BRCA2 mutations may account for up to 10% of all breast cancers, or 1 out of every 10 cases.
Having a BRCA1 or BRCA2 mutation doesn’t mean you will be diagnosed with breast cancer. Researchers are learning that other mutations in pieces of chromosomes called SNPs may be linked to higher breast cancer risk in women with a BRCA1 mutation as well as women who didn’t inherit a breast cancer gene mutation.
Women who are diagnosed with breast cancer and have a BRCA1 or BRCA2 mutation often have a family history of breast cancer, ovarian cancer, and other cancers. Still, most people who develop breast cancer did not inherit a genetic mutation linked to breast cancer and have no family history of the disease.
You are substantially more likely to have a genetic mutation linked to breast cancer if:
If one family member has a genetic mutation linked to breast cancer, it does not mean that all family members will have it.
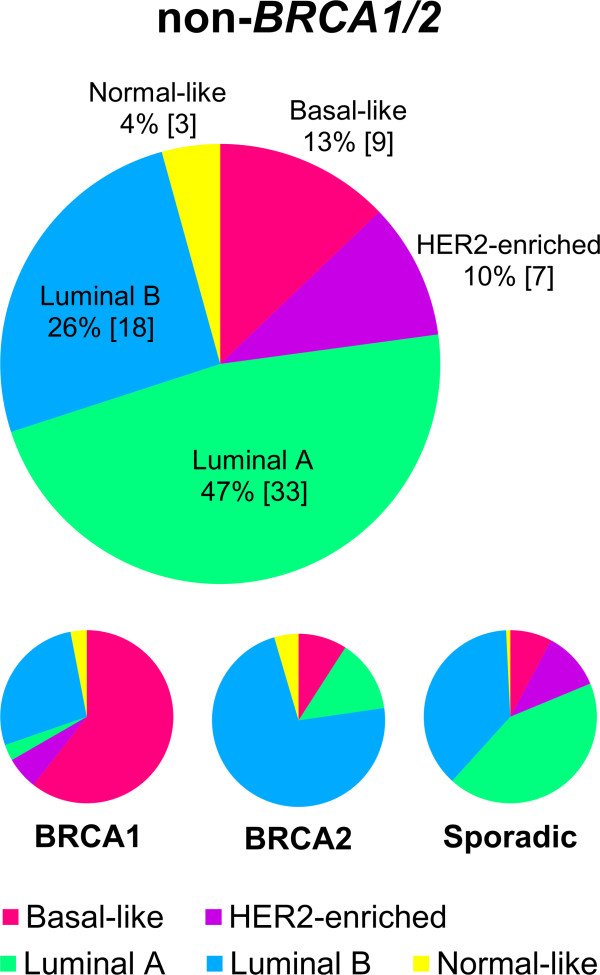
The Genetic Basis Of Breast Cancer Subphenotypes
Triple-negative breast cancers are associated with poor prognosis due to aggressive tumor behavior and poor response to chemotherapy. After screening 2301 triple-negative cases and 3949 controls, Antoniou et al identified five SNPs on 19p13 that modify risk in BRCA1 mutation carriers and are specifically associated with triple-negative breast cancer. Additional phenotypic subtypes which are currently being interrogated genetically include differences in susceptibility variants between racial groups and in response to treatment and prognosis.
Also Check: Can Little Girls Get Breast Cancer
Ovarian Cancer And Other Cancers
BRCA1 and BRCA2 mutations increase a womans risk of ovarian cancer, pancreatic cancer and melanoma .
BRCA1/2 mutations may also increase the risk of other cancers . However, data are limited and these topics are still under study.
|
For a summary of research studies on BRCA1 and BRCA2 mutations and cancer,;visit the Breast Cancer Research Studies section. |
Low Penetrant Breast Cancer Loci
A number of common breast cancer susceptibility loci have been associated with a slightly increased or decreased risk of breast cancer. These can follow the polygenic model, or can act synergistically with environmental factors or lifestyle, to account for a small fraction of familial breast cancer cases.
Most of these low-susceptibility loci have been highlighted through genome wide association studies and initially included a number of loci. In the final breast cancer assessment risk, six SNPs showed statistically significant association: MAP3K1, FGFR2, LSP1, TNRC19, and H19 .
Moreover, a particular SNP in CASP8 was identified to confer a slightly increased susceptibility in a candidate-gene study .
Although the actual contribution of low power, common susceptibility loci in hereditary breast cancer is debatable, the identification of such alleles can explain a subset of breast cancer cases.
Recommended Reading: Does Pain In Your Breast Mean Cancer
Breast Cancer And Genetic Testing
At the current time, testing is available for BRCA gene mutations, as well as mutations ATM, CDH1, CHEK2, MRE11A, MSH6, NBN, PALB2, PMS2, PTEN, RAD50, RAD51C, SEC23B, and TP53, with this area expected to expand dramatically in the near future.
Having these tests available, however, raises many questions. For example, who might have hereditary breast cancer and who should be tested? What should you do if you test positive for one of these genes?
Ideally, any testing should be done only with the guidance and help of a genetic counselor. There are two reasons for this.
One is that it can be devastating to learn that you carry a mutation that may increase your risk, and the guidance of someone who is aware of recommended management and screening is invaluable.
As noted earlier, some mutations confer a high risk and others a much lower risk. Some mutations might be of more concern earlier in life , whereas others might not require early screening. A genetic counselor can help you learn about what is currently recommended with regard to screening for your particular mutation while taking into account any other risk factors you might have.
The other reason genetic counseling is so important is that you may have a significant risk of developing breast cancer even if your tests are negative. There is much yet to learn, and a genetic counselor can help you look at your family history to see if you may carry a high risk despite negative testing, and plan screening accordingly.
Breast Cancer: Risk Factors And Prevention
Have questions about breast cancer? Ask here.
ON THIS PAGE: You will find out more about the factors that increase the chance of developing breast cancer. Use the menu to see other pages.
A risk factor is anything that increases a persons chance of developing cancer. Although risk factors often influence the development of cancer, most do not directly cause cancer. Some people with several risk factors never develop cancer, while others with no known risk factors do. Knowing your risk factors and talking about them with your doctor may help you make more informed lifestyle and health care choices.
Most breast cancers are sporadic, meaning they develop from damage to a persons genes that occurs by chance after they are born. There is no risk of the person passing this gene on to their children, as the underlying cause of sporadic breast cancer is environmental factors.
Inherited breast cancers are less common, making up 5% to 10% of cancers. Inherited breast cancer occurs when gene changes called mutations are passed down within a family from parent to child. Many of those mutations are in tumor suppressor genes, such as BRCA1, BRCA2, and PALB2. These genes normally keep cells from growing out of control and turning into cancer. But when these cells have a mutation, it can cause them to grow out of control.
The following factors may raise a womans risk of developing breast cancer:
You May Like: What Age Do Women Get Breast Cancer
Talking About Family Health History With Your Health Care Provider
Your family history of breast cancer and other health conditions is important to discuss with your health care provider. This information helps them understand your risk of breast cancer.
|
Susan G. Komen®s My Family Health History Tool |
|
My Family Health History tool is a web-based tool that makes it easy for you to record and organize your family health history. It can help you gather information thats useful as you talk with;your doctor or genetic counselor. |
Your Race And Ethnicity
Overall, white women are slightly more likely to develop breast cancer than African American women, although the gap between them has been closing in recent years. In women under age 45, breast cancer is more common in African American women. African American women are also more likely to die from breast cancer at any age. Asian, Hispanic, and Native American women have a lower risk of developing and dying from breast cancer.
Risk in different groups also varies by type of breast cancer. For example, African American women are more likely to have the less common triple-negative breast cancer.
Don’t Miss: Can Cancer Spread To The Breast
Inheriting Certain Gene Changes
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene changes passed on from a parent.
BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of these genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has up to a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer. ;
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts.
- Women with one of these gene changes also have a higher risk of developing ovarian cancer and some other cancers.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi origin than in other racial and ethnic groups, but anyone can have them.
Other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
Mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Clinical Management Of Carriers Of Brca Pathogenic Variants
Increasing data are available on the outcomes of interventions to reduce risk in people with agenetic susceptibility to breast cancer or ovarian cancer. As outlined in other sections of this summary, uncertainty is oftenconsiderable regarding the level of cancer risk associated with a positivefamily history or genetic test. In this setting, personal preferences arelikely to be an important factor in patients decisions about risk reductionstrategies.
You May Like: What Are The Symptoms Of Stage 1 Breast Cancer
Brca1 And Brca2 Inherited Gene Mutations
Like other inherited gene mutations, BRCA1 and BRCA2 gene mutations are rare in the general population. In the U.S., about 1 in 400 people have a BRCA1/2 mutation .
Prevalence varies by ethnic group. Among Ashkenazi Jewish men and women, about 1 in 40 have a BRCA1/2 mutation .
Learn more about BRCA1/2 mutations.
Risk Factors For Endometrial Cancer
Refer to the PDQ summary on Endometrial Cancer Prevention for information about risk factors for endometrial cancer in the general population.
Age
Age is an important risk factor for endometrial cancer. Most women with endometrial cancer are diagnosed after menopause. Only 15% of women are diagnosed with endometrial cancer before age 50 years, and fewer than 5% are diagnosed before age 40 years. Women with Lynch syndrome tend to develop endometrial cancer at an earlier age, with the median age at diagnosis of 48 years.
Family history including inherited cancer genes
Although the hyperestrogenic state is the most common predisposing factor for endometrial cancer, family history also plays a significant role in a womans risk for disease. Approximately 3% to 5% of uterine cancer cases are attributable to a hereditary cause, with the main hereditary endometrial cancer syndrome being Lynch syndrome, an autosomal dominant genetic condition with a population prevalence of 1 in 300 to 1 in 1,000 individuals.
Reproductive history
Reproductive factors such as multiparity, late menarche, and early menopause decrease the risk of endometrial cancer because of the lower cumulative exposure to estrogen and the higher relative exposure to progesterone.
Hormones
Recommended Reading: Can Estroven Cause Breast Cancer
Genes Associated With Hereditary Prostate Cancer
Recent research indicates specific mutations are responsible for hereditary prostate cancer and men who have these gene mutations are at increased risk for the condition. BRCA1 or BRCA2 inherited gene mutations can increase the risk of prostate cancer in some men. BRCA 1 or; 2 mutation increases the risk of developing a more severe form of prostate cancer.;;
A condition known as Lynch syndrome or HNPCC is also linked to inherited gene changes and increase the risk of prostate cancer among other cancers.
Other genes linked to an increased risk of prostate cancer include ATM, CHEK2, NBN, PALB2.
Uptake Of Genetic Counseling And Genetic Testing
Degree of uptake of genetic counseling and genetic testing
Comparison of uptake rates among studies in which counseling and testing were offered is challenging because of differences in methodologies, including the sampling strategy used, the recruitment setting, and testing through a research protocol with high-risk cohorts or kindreds. In a systematic review of 40 studies conducted before 2002 that had assessed genetic testing utilization, uptake rates varied widely and ranged from 25% to 96%, with an average uptake rate of 59%. Results of multivariate analysis found that BRCA1/BRCA2 genetic testing uptake was associated with having a personal or family history of breast or ovarian cancer, and with methodological features of the studies, including sampling strategies, recruitment settings, and how studies defined actual uptake versus the intention to have testing.
Other factors have been positively correlated with uptake of BRCA1/BRCA2 genetic testing, although these findings are not consistent across all studies. Psychological factors that have been positively correlated with testing uptake include greater cancer-specific distress and greater perceived risk of developing breast or ovarian cancer. Having more cancer-affected relatives also has been correlated with greater testing uptake.
Table 14 summarizes the uptake of genetic testing in clinical and research cohorts in the United States.
| Study Citation |
|---|
You May Like: How To Help Breast Cancer Awareness
Is There A Test For Hereditary Breast Cancer
Hereditary breast cancer is suspected when there is a strong family history of breast cancer: occurrences of the disease in at least three first or second-degree relatives . Currently the only tests available are DNA tests to determine whether an individual in such a high-risk family has a genetic mutation in the BRCA1 or BRCA2 genes.
When someone with a family history of breast cancer has been tested and found to have an altered BRCA1 or BRCA2 gene, the family is said to have a “known mutation.” Positive test results only provide information about the risk of developing breast cancer. The test cannot tell a person whether or when cancer might develop. Many, but not all, women and some men who inherit an altered gene will develop breast cancer. Both men and women who inherit an altered gene, whether or not they develop cancer themselves, can pass the alteration on to their sons and daughters.
But even if the test is negative, the individual may still have a predisposition to hereditary breast cancer. Currently available technique can’t identify all cancer-predisposing mutations in the BRCA1 and BRCA2 genes. Or, an individual may have inherited a mutation caused by other genes. And, because most cases of breast cancer are not hereditary, individuals may develop breast cancer whether or not a genetic mutation is present.
Screening And Prevention Strategies
| Addressed in general terms and other guidelines referenced | Addressed in general terms and other guidelines referenced |
| Genetic Counseling: Addressed |
References
Don’t Miss: Is Stage 2 Breast Cancer Bad
Is Breast Cancer Hereditary
Breast cancer is the second most common cancer in women in the United States, and with one in every eight women developing some form of invasive breast cancer in their lifetime,1 many people know at least one woman that has been diagnosed with the disease.
Genetic research has revealed that adverse mutations in a handful of different genes can greatly increase an individuals risk of developing breast cancer, and importantly, these hereditary forms of breast cancer can be passed from an affected parent to their child. ;Here, in recognition of Breast Cancer Awareness Month this October, we highlight the prevalence of hereditary breast cancer and how individuals can better assess their own hereditary cancer risk.
There are many different types of invasive breast cancer, or breast cancer that has spread beyond the site where it originally developed. The types of breast cancer differ in where the cancer originates, the appearance of and the presence or absence of hormone receptors on the cancer cells, and whether or not the cancer cells have too many copies of the HER2 gene. The types of invasive breast cancer and the percentage of diagnoses attributed to each type are listed below:
- Invasive ductal carcinoma – 70-80%