Types Of Surgery For Breast Implants A Breast Implant Is Placed In A Space Under Chest Muscle Doctors Can Use The Following Approaches To Create The Pocket
Tissue expansion
If the skin and tissues in the chest are too tight or flat for the surgeon to place the implant, they will need to make the space larger. This is called tissue expansion.
The surgeon places an expander implant under the skin and muscles on the chest. An expander implant is an empty bag with a small valve, like a balloon. Sometimes the expander implant is placed during surgery to remove part or all of the breast . It can also be placed during a surgery done at a later time.
Once the expander implant is in place, the doctor slowly fills it with saline. The doctor passes a very small needle through the skin and into the valve to inject the saline. This is done every 1 or 2 weeks in the doctors office until the skin is stretched enough to fit a breast implant that is the same size as the opposite breast. This may take up to 3 months.
Once the skin is stretched enough, the surgeon does a second operation to remove the expander implant and place the permanent implant. Sometimes the expander implant is left in place as the final implant.
One-step reconstruction
One-step reconstruction is also called direct-to-implant reconstruction. It is a newer procedure that may be an option for some women. This type of implant uses special donated human skin tissue called acellular dermal matrix . The cells are removed from the donated tissue to prevent rejection.
Can Everyone Have Breast Reconstruction Surgery
Breast reconstruction may not be possible for everyone. For example, breast reconstruction is not recommended if you are a smoker, have a medical condition such as obesity or diabetes or if your cancer is at an advanced stage.
These factors can put you at a greater risk of serious problems after surgery and they will be taken into consideration, along with your preferences and the recommendations of your surgeon, when determining the type of reconstruction that is best for you.
What Are The Different Types Of Breast Reconstruction
There are 2 main types of reconstruction surgery:
-
Expander-implant. This method uses an expander that’s filled over time to slowly stretch the skin to create a breast mound. This may be followed by the placement of a permanent breast implant.
-
Autologous tissue. This method uses your own body tissues to reconstruct a new breast mound. These reconstruction surgeries leave you with 2 surgical wounds: your chest and the site where tissue was removed.
In some cases, you may have a combination of both types of reconstruction. You may also decide to have other procedures to improve how your new breast shape looks. For instance, you might decide to have reconstructive surgery on your other breast so that it matches your new breast shape. Or you may want to have a nipple or areola reconstructed.
Recommended Reading: Is There Pain With Breast Cancer Symptoms
Choosing The Type Of Breast Reconstruction Thats Right For You
Breast reconstruction can be done with:
- Breast implants
- Natural tissue flaps
- A combination of these methods
Theres no one breast reconstruction method that works best for everyone. You may be a good candidate for one reconstruction method, but not another. There are pros and cons to each method.
For example, breast implants require less invasive surgery than procedures using your own body tissues, but the results may look and feel less natural .
Possible Risks During And After Reconstruction Surgery
Any type of surgery has risks, and breast reconstruction may pose certain unique problems for some women. Even though many of these are not common, some of the possible risks and side effects during or soon after surgery include:
- Problems with the anesthesia
Problems that can develop later on include:
- Tissue death of all or part of a tissue flap, skin, or fat
- Loss of or changes in nipple and breast sensation
- Problems at the donor site, such as loss of muscle strength, bulging of the abdominal wall, and dimples in the skin
- The need for more surgery to fix problems that come up
- Changes in the arm on the same side as the reconstructed breast
- Problems with a breast implant, such as movement, leakage, rupture, rippling , or scar tissue formation
- Uneven breasts
You May Like: Do You Lose Your Hair With Chemotherapy For Breast Cancer
How Do I Know What Type Of Breast Reconstruction Surgery To Get
Your provider will recommend the most appropriate technique for you based on:
- Your age, overall health and lifestyle.
- The kind of mastectomy or lumpectomy you had and how much tissue remains.
- Whether you need additional treatments for breast cancer .
- Past surgeries youve had that may make it difficult or impossible to take a flap from your belly. One example is abdominal surgery.
- Your goals and desired appearance.
Recovery From Breast Reconstruction Surgery
You may have some discomfort for the first few days afterward. Youâll get pain medication as needed. Throughout your hospital stay, the staff will closely watch you.
Soon after surgery, youâll be encouraged to move your arms, but not for any forceful activity like pulling yourself up, getting out of bed, or lifting heavy objects. Nurses will help you in and out of bed. The day after surgery, you may be able to sit in a chair beside the bed. On the second day, most patients are walking without help.
Youâll probably get IV fluids for a day or two. You may have a urinary catheter overnight or until you can walk to the bathroom. And where the surgeon made cuts , youâll have drains. If you go home with these drains in place, youâll get instructions on how to care for them.
The length of your hospital stay depends on the type of operation and how your recovery goes. If you got implants, the average hospital stay is 1 to 2 days. Flap procedures may require a stay of 5 to 6 days.
Read Also: How Can Breast Cancer Be Treated
Breast Reconstruction After Mastectomy For Breast Cancer
Copyright and License informationDisclaimerCorrespondence to:Copyrightcited by
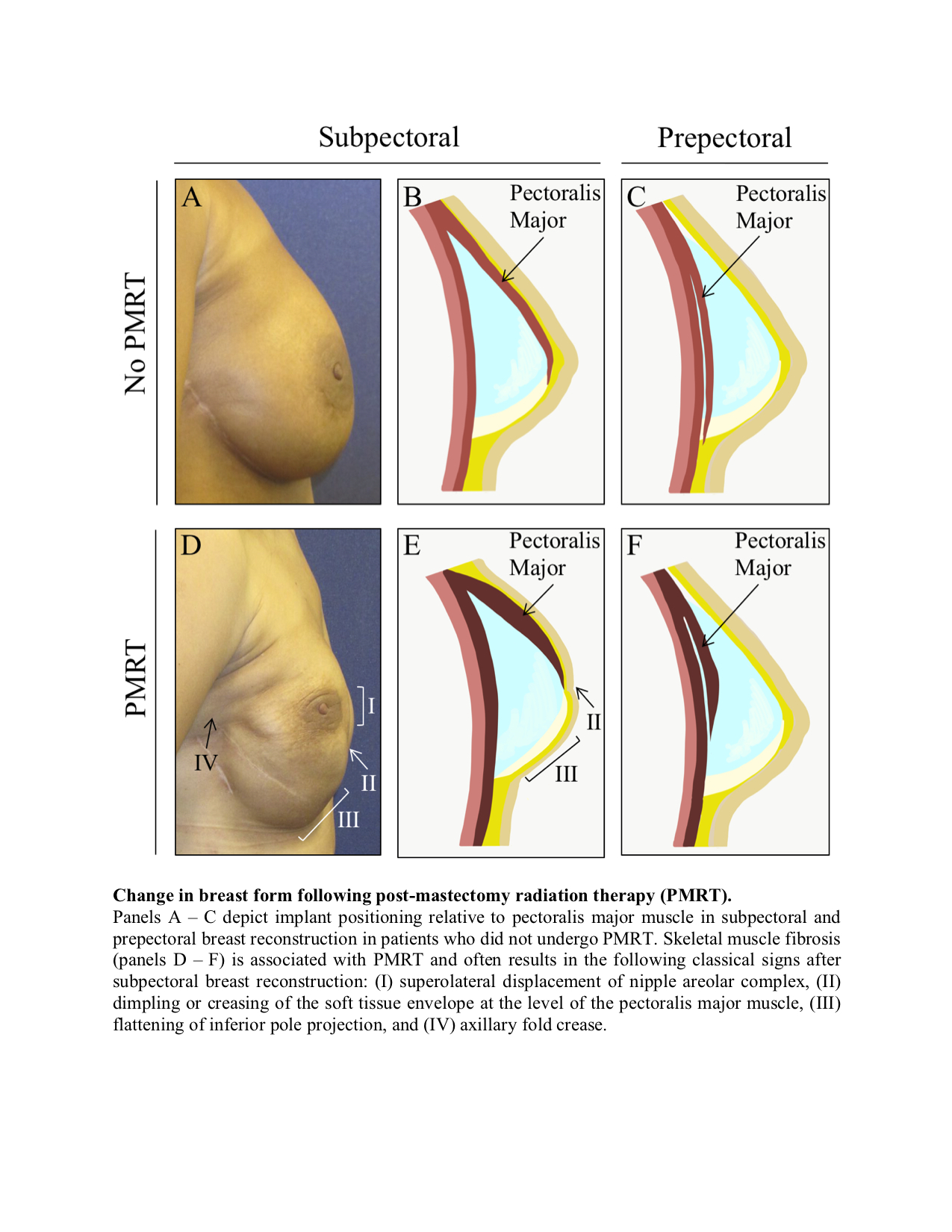
Just as there have been improvements in the early detection and treatment of breast cancer, there have also been improvements in the techniques used for breast reconstruction after mastectomy. There are many reconstructive methods available, using either autologous tissue or implants,1 each with its unique set of indications, contraindications, advantages, disadvantages and complications . Breast reconstruction after mastectomy is oncologically safe7,8 and is associated with high satisfaction and improved psychosocial outcomes.9 Although the rates of major complications after immediate reconstruction are greater than after mastectomy alone, clinically significant delays in the receipt of adjuvant therapy after immediate reconstruction have not been found.10,11 Despite the potential psychological benefits of breast reconstruction, few patients who have had a mastectomy undergo breast reconstruction.12
Body Tissue Reconstruction Surgery
With this operation, your surgeon takes skin, fat, and sometimes muscle from another part of your body and makes it into a breast shape.
Advantages
- Body tissue reconstruction can usually be done in one or two operations, but you may need minor adjustments to the new or opposite breast.
- The reconstructed breast is warm and gives a more natural shape and feel compared to an implant .
- Women with small or large breasts can have this type of surgery.
Disadvantages
- It is a much bigger and longer operation than implant reconstruction.
- The operation leaves you with two wound sites and two sets of scars.
- There is the risk of arm weakness if you have tissue taken from your back .
- There is a risk of tummy weakness if you have tissue taken from your tummy .
The reconstructed breast tends to match the other breast well at first but may droop after some time. So then the breasts may be out of alignment.
You May Like: Where Does Breast Cancer Start
Timing Of Your Reconstruction Surgery
Should you decide to have breast reconstruction surgery, there are basically two options open to you with regards to when it should be done. These are:
Which of the two you end up doing is a decision youll need to make from discussing with your doctors who are trained to guide you into making the right one. The following factors are known to influence that decision.
1. Radiation therapy. This is the most important factor determining the appropriate timing for your reconstruction. The presence of implants could interfere with the delivery of radiation to target areas.
This could affect the efficacy of your treatment but having the reconstruction done before radiation is better as the procedure may be problematic after radiation.
For anyone having natural tissue reconstruction but who must go through radiation, delayed reconstruction is better so the damaged body tissues from the radiation can be replaced by healthy ones during the reconstruction.
In the absence of radiation therapy, flap tissue reconstruction could still be done immediately following mastectomy with great outcomes as a study in the Journal of American society of plastic surgeonsThe journal of American Society of Plastic Surgeons Visit source has revealed.
Choosing the best for your situation is something to discuss with your doctor.
Is Breast Reconstruction Post
While it appears that there are multiple mechanisms in the reconstruction which create a pro-oncogenic environment, their consistent impact has yet to materialize in vivo. Indeed, recent research focuses on the risk-reducing mastectomy as the first line of defense against recurrence . In one study regarding flap surgery, among a list of varied complications , recurrence is not listed as one of them . While delayed wound healing and re-operation rates were higher with implant reconstruction, there is no significant increased risk of recurrence with implant placement compared to mastectomy alone . Recently, it was found that lipofilling to augment the shape of an LD flap resulted in seromas and wound dehiscence. However, the fat grafting brought no recurrence to any patient in the study . These reports are snapshots of a wider sample of work, partly described in the body of this review, which all generally report similar outcomes.
Also Check: What Does Stage 3 Breast Cancer Look Like
First Steps: Meeting With Your Surgeons
Determining whether youre a candidate for breast reconstruction, and if so, which options you qualify for, is often a multi-step process that involves some back-and-forth among you, your breast surgeon, your plastic surgeon and the rest of your cancer care team.
Patients should see a breast cancer surgeon before consulting with a plastic surgeon for reconstruction. The breast surgeon should have a pretty clear recommendation about whether you need a mastectomy or a lumpectomy. This may be a clinical judgement that changes depending on where you go for treatment or which doctor you see.
The type of surgery chosen is often a personal decision for the patient. Sometimes a woman has a very small tumor that could be removed with a lumpectomy, but she doesnt want to deal with radiation and lifelong mammographic surveillance. Or, she may have anxiety about the potential for a cancer recurrence. Genetic mutations, such as BRCA1 and BRCA2 that are known to increase the lifetime risk of breast cancer, are appropriate medical indications for prophylactic mastectomies. A woman with one of these genetic mutations may choose to have a bilateral mastectomy for her own peace of mind.
When To Have Reconstruction

Most women who opt for breast reconstruction have it done at the same time as the initial surgery. This is known as immediate reconstruction. You will be referred to a plastic surgeon or oncoplastic breast surgeon as part of the surgical planning process. However, there are often valid reasons why a delayed reconstruction is recommended:
- There is an urgent need for chemotherapy. If chemotherapy treatment needs to be undertaken first, it’s important to talk with your surgeon about wanting reconstruction once this has been completed.
- Post-mastectomy radiation will be required. Flap reconstruction, using your own tissue, has better outcomes after radiation treatment.
- Factors such as smoking, diabetes and obesity increase the risk of infection, poor wound healing and other complications and reconstruction may have to be delayed until these risks have been lowered.
Some women may prefer to have the cancer removed and treated before making any decision about whether to have breast reconstruction.
Many women have a delayed reconstruction by choice, often some years after the original surgery. Unfortunately, in some areas of New Zealand women might experience a long wait to have this done in a public hospital. If you are considering having a delayed reconstruction and are no longer being seen for follow-up at the breast clinic, ask your GP to refer you to a plastic surgeon to discuss the options available to you.
Recommended Reading: Can I Get Breast Cancer At 15
When Is The Best Time To Have Breast Reconstruction
Talk with your healthcare provider before your mastectomy. You may meet with a plastic surgeon. This is the healthcare provider who does the reconstruction surgery after the mastectomy is done. Your healthcare providers will then talk with you about your options for:
-
Immediate reconstruction. This is reconstruction surgery done at the same time as the mastectomy.
-
Delayed reconstruction. This is a surgery done after you recover from the mastectomy. If radiation therapy is part of your treatment plan, you may be advised to wait until after the radiation is finished.
Here are some things to keep in mind about the best time to schedule your surgery:
-
The overall surgery plan. Breast reconstruction can involve many surgeries over a period of time to complete the reconstruction. Be sure to discuss this with your surgeon so you know what to expect.
Whens The Best Time To Have Breast Reconstruction
The timing is based on what you want to do, your medical conditions, and your cancer treatment. You can have it done during the operation to remove the breast, or you can have it months or years after a mastectomy.
If you’ve started chemotherapy or radiation treatments, reconstruction is usually put off until theyâre finished. Your surgeon can help you decide the best timing for you.
Read Also: Does Smoking Increase Risk Of Breast Cancer
What Should I Ask My Breast Surgeon
Make sure youve got all the facts you need and have received answers to all your questions before making an informed decision. You may find it helpful to write down any questions you want to ask and to take notes during consultations. Taking someone with you can help you to remember what has been discussed and give you extra support.
Here are some questions you may want to ask your surgeon.
- Can I have an ?
- Which reconstruction would be best for me and why?
- What are the benefits, limitations and risks of this type of surgery?
- When would I be able to have my surgery done?
- How long would I have to stay in hospital?
- What is the recovery time for this operation?
- When would I be able to move about, walk and drive?
- How much pain is there likely to be?
- Can you show me where the scars would be and how big/long?
- Would I have scars elsewhere on my body?
- Would I be able to keep my nipple?
- Can reconstruction surgery delay my other cancer treatments, like chemotherapy and radiotherapy?
- When would I be able to exercise again?
- Can you show me any photographs or images of your previous breast reconstructions?
- Can I speak to someone who has had the same type of reconstruction?
- Would I need to wear a special bra after the operation?
Basic Types Of Breast Reconstruction
The table below compares the basic types of breast reconstruction.
Specific types of reconstruction are discussed in more detail below.
|
Risk of complications |
|
|
|
Risk of complete reconstruction failure |
|
|
|
Adapted from selected sources . |
Recommended Reading: Does Breast Cancer Kill You
How To Prepare For The Surgery
1. Youll do well to stop smoking if you smoke as it delays healing and increases risks.
2. Do research and look for a reputable microvascular or plastic surgeon with experience.
3. Write down all the questions you may have and ask all you want to know about your surgery.
4. Join support groups in your locality or online to learn from others experiences.
5. Discuss your hopes for the surgery to help align your expectations with realities.
6. If you are on any medications, bring them to the notice of your surgeons.
7. You may be asked to stop herbal supplements, anti-inflammatory drugs, and blood thinners in due time.
8. Depending on your unique situation, certain medications may be prescribed including tests.
9. Avail yourself of any help offered by family, friends, and people that have been in your situation.
10. Prior to your surgery, find out what youll need at home thatll be helpful in your recovery.