What Can Men Do To Reduce The Risks Of Breast Cancer
From the things that you eat to the chemicals you expose yourself to, all of these can help determine whether you are at a higher or lower risk of the disease. All men can lower their risk of developing breast cancer by keeping a healthy weight and exercising regularly. Although there is no single ideal weight for all individuals, Body Mass Index is a common tool that measures a persons weight in relation to their height. Age is not a factor in BMI for adults. BMI can offer a rough idea of whether or not a person is at a moderate weight.
To calculate BMI kg the metric formula is your weight in kilograms divided by your height in metres squared. For example, if you are 175cm in height and 75kg in weight, you can calculate your BMI as follows: 75kg / = 24.49kg/m².
A BMI calculation provides a single number, which falls into the following categories:
- A BMI of less than 18.5 means a person is underweight.
- A BMI of between 18.5 and 24.9 is ideal.
- A BMI of between 25 and 29.9 is overweight.
- A BMI over 30 indicates obesity.
Avoid or limit alcohol Alcohol use increases the risk of breast cancer in both women and men. Even low levels of alcohol intake have been linked with an increase in risk. Alcohol use is linked with several cancers and is the third most important preventable risk factor for cancer. It is best not to drink alcohol. For men who do drink, they should have no more than two alcoholic drinks a day.
How Often To Screen
Once a woman has decided to begin screening, the next decision is how often to undergo screening. No clinical trials compared annual mammography with a longer interval in women of any age. In the randomized trials that demonstrated the effectiveness of mammography in reducing breast cancer deaths in women aged 40 to 74 years, screening intervals ranged from 12 to 33 months.2, 3 There was no clear trend for greater benefit in trials of annual mammography, but other differences between the trials preclude certainty that no difference in benefit exists. Available observational evidence evaluating the effects of varying mammography intervals found no difference in the number of breast cancer deaths between women aged 50 years or older who were screened biennially versus annually.2, 3
Regardless of the starting age for screening, the models consistently predict a small incremental increase in the number of breast cancer deaths averted when moving from biennial to annual mammography, but also a large increase in the number of harms .7, 8 The USPSTF concludes that for most women, biennial mammography screening provides the best overall balance of benefit and harms.
How Do You Check Your Breasts For Lumps
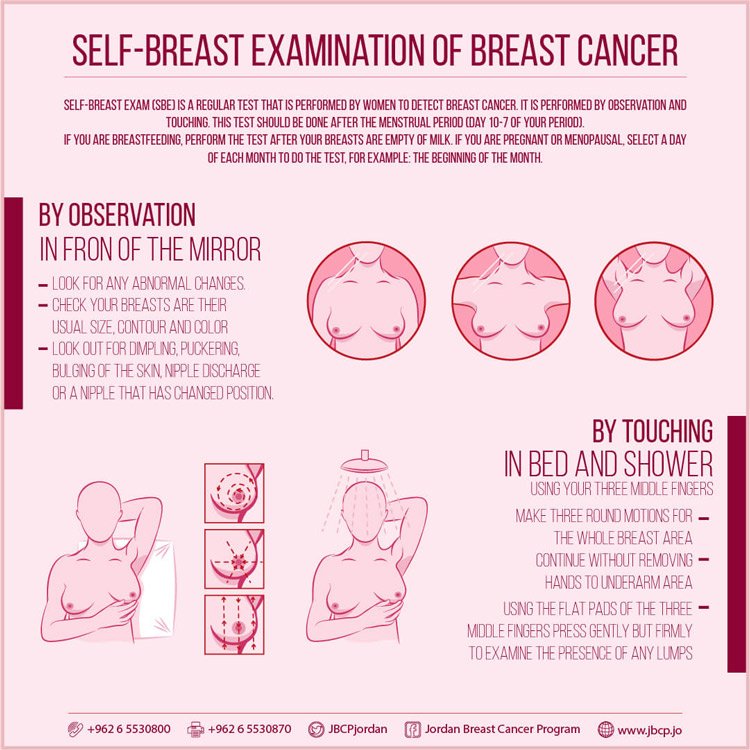
Follow the below steps to help you check how to check breast cancer at home:-
- Stand in front of the mirror with your shoulders straight and your arms on your hips, looking at your breasts. Skin that is dimpling, puckering or bulging.
- Raise your arms and look for the same changes as before.
- Examine your nipples in the mirror for any symptoms of fluid leaking from one or both of them .
- Keep your fingers flat and together while applying a firm, smooth touch to the first few finger pads of your hand. Make a quarter-sized circular motion with your hands.
- From your collarbone to the top of your abdomen, and from your armpit to your cleavage, cover the entire breast from top to bottom, side to side.
You May Like: Where Does Triple Negative Breast Cancer Metastasis To
How Is Breast Cancer Detected And Diagnosed
An accurate and thorough diagnosis is important so that your breast cancer team can develop the best treatment plan for you. At City of Hope, your care team will utilize the most state-of-the art breast imaging technologies and laboratory techniques to guide your personalized treatment.
If you notice changes in your breast, experiencing breast pain, or as part of a routine breast screening, your doctor may use tests to look for breast cancer. An integral part of diagnosing breast cancer begins with your doctor asking questions about your health history, your symptoms, risk factors, and family history of disease.
Inspection While Lying Down
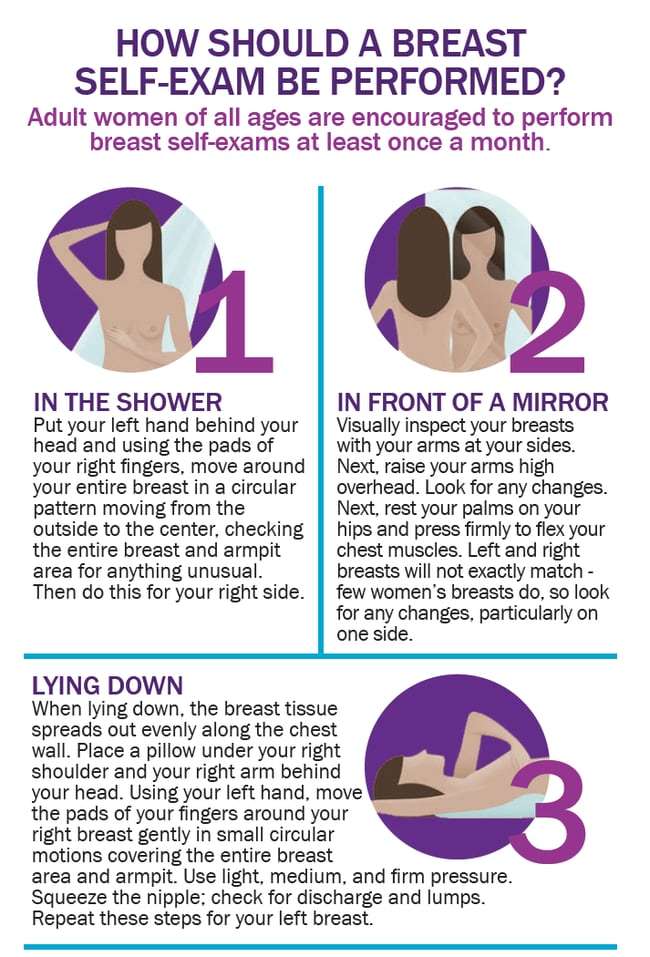
As you lay down the tissues of your breast spread off evenly. So one can feel the changes especially if one has heavy breasts. You need to lie down and then put a pillow under your right shoulder. Place the right arm behind your head. Again, by applying the pads of your fingers press the different parts of the tissue and under your arm. Next put the pillow on the other side and check the armpit and breast.
You May Like: Breast Cancer How To Check
Genetic Testing For Hereditary Breast And Ovarian Cancer
Genetic testing is available for hereditary breast and ovarian cancer. Most breast and ovarian cancer is not caused by inherited mutations, so genetic testing will not help most women with a family health history of breast and ovarian cancer. Genetic testing will not identify the cause for some hereditary breast and ovarian cancers, because the genes affected in these cancers are not yet known.
Genetic counseling before genetic testing for hereditary breast and ovarian cancer is important to determine whether you and your family are likely enough to have a mutation that it is worth getting tested. Usually, genetic testing is recommended if you have:
- A strong family health history of breast and ovarian cancer
- A moderate family health history of breast and ovarian cancer and are of Ashkenazi Jewish or Eastern European ancestry
- A personal history of breast cancer and meet certain criteria
- A personal history of ovarian, fallopian tube, or primary peritoneal cancer
- A known BRCA1, BRCA2, or other inherited mutation in your family
The BRCA1 and BRCA2 genes
Genetic counseling after genetic testing is important to help you understand your test results and decide the next steps for you and your family:
What Does Receptor Status Mean In Breast Cancer
Your breast cancer may be classified as hormone receptor positive or negative, depending on whether it has particular protein receptors on its surface or not. This is known as the hormone receptor status. Breast cancer cells with hormone receptors may be stimulated by your own natural hormones, or by the pill or hormone replacement therapy.
The hormone receptor status you receive may include:
- ER+ breast cancer has receptors for oestrogen
- PR+ breast cancer has receptors for progesterone
- ER- and PR- breast cancer has neither oestrogen or progesterone receptors
If your breast cancer is classified as hormone receptor positive, it may respond to treatments that adjust or block the hormones in the body. This is known as hormone or endocrine therapy.
If your breast cancer is classified as hormone receptor negative, hormone treatment will not be effective.
Also Check: How Do You Feel If You Have Breast Cancer
Treatment For Breast Cancer
While there are many different types of breast cancer, its important to know that there are a wide range of treatments available. Your doctor will help you to understand what type of breast cancer you have and discuss your treatment options with you. These will depend on the subtype and stage of your breast cancer as well as your own health and personal situation.
Breast cancer treatment includes local treatment to the breast and lymph node regions. If your breast cancer can be removed with a clear margin, a lumpectomy and radiation therapy is as effective as a mastectomy. Breast cancer treatment also commonly includes drug therapy, such as hormone therapy and chemotherapy.
Do You Need Tests For Later
Imaging tests. If your cancer is stage IIIB or IV, you should get an imaging test to look for cancer in other parts of your body. Treatment can depend on how much and where the cancer has spread.
Tumor marker tests. If you have later-stage breast cancer, your doctor may also use blood tests to look at tumor markers. These tests should be done only when it is known that you have advanced cancer.
This report is for you to use when talking with your healthcare provider. It is not a substitute for medical advice and treatment. Use of this report is at your own risk.
09/2012
Also Check: Why Do I Need Chemo And Radiation For Breast Cancer
How Much Do Anastrozole And Exemestane Lower The Risk Of Breast Cancer
Studies have shown that both anastrozole and exemestane can lower the risk of breast cancer in postmenopausal women who are at increased risk of the disease.
In one large study, taking anastrozole for five years lowered the risk of developing estrogen receptor-positive breast cancer by 53 percent. In another study, taking exemestane for three years lowered the risk of developing estrogen receptor-positive breast cancer by 65 percent.
The most common side effects seen with anastrazole and exemestane are joint pains, decreased bone density, and symptoms of menopause .
Last reviewed by a Cleveland Clinic medical professional on 12/31/2018.
References
Why Are Self Exams Important
Not many people go to the doctor often to check their breasts, as they usually seem fine. Even if you do, not all early tests can discover underlying issues. By combining regular doctor visits with self-exams, you ensure that any potential cancer is caught early.
When cancer is discovered early its more easily treatable, and more options and solutions can be discussed with your doctor.
Recommended Reading: Is Breast Cancer Only Genetic
What Are The Signs And Symptoms Of Breast Cancer In Men
Most men dont realise that they need to be chest aware. However, it is important to check yourself regularly, as 70% of breast cancer cases in men are primarily detected by self-examination. This is how you can do a male breast self-examination:
Regular breast self-examinations can help you know how your breasts normally look and feel. Most breast lumps or changes are not cancer, but you should always have them checked by your GP.
Symptoms of breast cancer in men may include:
- A lump or swelling in the chest area or armpit.
- Discharge from the nipple, which may be blood stained.
- An inverted nipple.
- Ulcers or sores on the chest or around the nipple.
- A rash on or around the nipple.
- Changes in the shape or size of the breast.
Sometimes breast cancer can spread to lymph nodes under the arm or around the collar bone and cause a lump or swelling there, even before the original tumour in the breast is large enough to be felt. Should you notice anything unusual or are worried, make an appointment to see your GP as soon as possible. A lump in your breast may be a sign of breast cancer however, more commonly, a lump may be a sign of a condition that can be treated, such as a hormone problem.
Who Can Get Breast Implant Associated Cancer
All reported cases of breast implant associated cancer in Australia involve patients who have had a textured implant at some point in their life. Based on current evidence, experts do not think breast implant associated cancer is related to either the contents or shape of the implant.
Breast implant associated cancer is rare. The recent review by the TGA has found between one in 2,500 and one in 25,000 people with breast implants are diagnosed with the condition in Australia based on confirmed cases of BIA-ALCL where only one brand of implant had been used. The risk of developing BIA-ALCL increases with increasing texturing of the implant. Implants which have a smooth surfaced have not been associated with BIA-ALCL. Breast implant associated cancer can occur after either reconstruction or augmentation surgery, with 95% of cases occurring between three and 14 years after the insertion of an implant.
Recommended Reading: Do You Feel Ill If You Have Breast Cancer
Clinical Considerations And Recommendations
How should individual breast cancer risk be assessed?
Health care providers periodically should assess breast cancer risk by reviewing the patients history. Breast cancer risk assessment is based on a combination of the various factors that can affect risk Box 1610111213. Initial assessment should elicit information about reproductive risk factors, results of prior biopsies, ionizing radiation exposure, and family history of cancer. Health care providers should identify cases of breast, ovarian, colon, prostate, pancreatic, and other types of germline mutation-associated cancer in first-degree, second-degree, and possibly third-degree relatives as well as the age of diagnosis. Women with a potentially increased risk of breast cancer based on initial history should have further risk assessment. Assessments can be conducted with one of the validated assessment tools available online, such as the Gail, BRCAPRO, Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm, International Breast Cancer Intervention Studies , or the Claus model 34.
Is screening breast self-examination recommended in women at average risk of breast cancer, and what should women do if they notice a change in one of their breasts?
Should practitioners perform routine screening clinical breast examinations in average-risk women?
When should screening mammography begin in average-risk women?
How frequently should screening mammography be performed in average-risk women?
What Is Breast Cancer
Cells in the body normally divide only when new cells are needed. Sometimes, cells in a part of the body grow and divide out of control, which creates a mass of tissue called a tumor. If the cells that are growing out of control are normal cells, the tumor is called benign. If, however, the cells that are growing out of control are abnormal and dont function like the bodys normal cells, the tumor is called malignant .
Cancers are named after the part of the body from which they originate. Breast cancer originates in the breast tissue. Like other cancers, breast cancer can invade and grow into the tissue surrounding the breast. It can also travel to other parts of the body and form new tumors, a process called metastasis.
Recommended Reading: Can Ca125 Detect Breast Cancer
General Considerations For Screening
The goal of screening for cancer is to detect preclinical disease in healthy, asymptomatic patients to prevent adverse outcomes, improve survival, and avoid the need for more intensive treatments. Screening tests have both benefits and adverse consequences .
Breast self-examination, breast self-awareness, clinical breast examination, and mammography all have been used alone or in combination to screen for breast cancer. In general, more intensive screening detects more disease. Screening intensity can be increased by combining multiple screening methods, extending screening over a wider age range, or repeating the screening test more frequently. However, more frequent use of the same screening test typically is associated with diminishing returns and an increased rate of screening-related harms. Determining the appropriate combination of screening methods, the age to start screening, the age to stop screening, and how frequently to repeat the screening tests require finding the appropriate balance of benefits and harms. Determining this balance can be difficult because some issues, particularly the importance of harms, are subjective and valued differently from patient to patient. This balance can depend on other factors, particularly the characteristics of the screening tests in different populations and at different ages.
Msks Screening Guidelines For Breast Cancer
These are MSKs latest guidelines for breast cancer. They may be different from those of other groups of experts. We use an approach that saves the most lives. The type of screening you have and your screening schedule are based on your personal risk for breast cancer.
- Starting at age 20, become familiar with how your breasts look and feel. Knowing your breasts will help you notice changes.
- Get a breast exam from your healthcare provider every year starting at age 25.
- Starting at age 40, have a mammogram or tomosynthesis every year. First, talk with your healthcare provider about the possible reasons for and against getting screened. If your mammogram shows you have dense breasts, they may recommend additional screening tests. These can include an ultrasound or a mammogram with contrast. Contrast is a special dye used in imaging scans that makes it easier to see differences in your breasts.
- Starting at age 20, become familiar with how your breasts look and feel. Knowing your breasts will help you notice changes.
- Starting at age 25, get a breast exam by your healthcare provider every 6 months.
- If you have or had atypical hyperplasia or lobular neoplasia, start getting screened at age 30. If you were diagnosed at age 30 or older, start getting screened at the time of diagnosis.
- Get a mammogram or tomosynthesis every year.
- Your healthcare provider may recommend more imaging, such as an ultrasound, contrast mammography, or an MRI especially if you have dense breasts.
You May Like: Type Of Breast Cancer Surgery
Stay Ahead Of The Trend In Fashion And Beyond With Our Free Weekly Lifestyle Edit Newsletter
Television presenter Sarah Beeny has been diagnosed with breast cancer.
The 50-year-old was diagnosed with cancer three weeks ago after finding a lump in her breast. While an initial mammogram didnt show any signs of the disease, a biopsy confirmed it was cancer.
The nurse was so sweet and they were really nice to me but I thought, You dont understand. I have waited 40 years to hear those words. I knew I was going to hear it one day, Beeny explained.
Beenys mother was diagnosed with breast cancer when Beeny was a child. It spread to her brain and she died when Beeny was just 10 years old.
Beeny is currently awaiting a test to see if the disease is hereditary as her grandmother also had breast cancer. She also urged women to check their breasts regularly and to trust their instincts.