Ivana Sestak Phd On Clinical Treatment Score From Tailorx: Predicting Distant Breast Cancer Recurrence
Ivana Sestak, PhD, of Queen Mary University of London and the Centre for Cancer Prevention, discusses study findings that confirm the prognostic ability of the Clinical Treatment Score at 5 years for late distant recurrence, specifically for patients older than 50 years and/or for those deemed to have intermediate- or high-risk hormone receptorpositive, HER2-negative, node-negative breast cancer. The CTS5 is less prognostic in women younger than 50 who received 5 years of endocrine therapy alone .
Experts Navigate The New World Of Her2
OncologyLive
Treatment decisions in the second-line setting for patients with HER2-positive metastatic breast cancer are not as cut-and-dried as deciding between which data have the best outcomes.
Treatment decisions in the second-line setting for patients with HER2-positive metastatic breast cancer are not as cut-and-dried as deciding between which data have the best outcomes.
Nuances in patient populations, toxicity profiles, and sequencing considerations following disease progression in later lines of therapy are playing a larger role as new data mount. Adaptability will be key for oncologists in the coming years. been generated are going to move the sequence, Gradishar said. Its going to be different 1 year from now, and 2 years from now. What we have learned with confidence is that things are going to change. What I am struck by is every time we go to the ASCO or San Antonio , we compare the new data to the time when we started our careers….We fiddled with the handful of chemotherapy drugs we had and maybe the schedule. That was the big question at every meeting, William J. Gradishar, MD, said. Now we have new drugs, we understand more nuance or maybe we dont understand, and we are trying to figure out how to use these drugs optimally, and thats really excitingto juxtapose those 2 time periods.
Study Participants Had Metastatic Or Inoperable Breast Cancer
The clinical trial, called DESTINY-Breast04, enrolled 557 adults who had metastatic or inoperable HER2-low breast cancer and had previously been treated with one or two types of chemotherapy. Nearly 90% of participants had hormone receptorpositive disease, meaning their tumors had receptors for the hormones estrogen and/or progesterone. The trial was funded by the developers of T-DXd, Daiichi Sankyo and AstraZeneca.
Two-thirds of participants were randomly assigned to receive T-DXd and the rest to receive their doctors choice of chemotherapy. T-DXd was given intravenously every 3 weeks and patients were followed for a median of about 18 months.
In the group that received T-DXd, the median time that people lived without their cancer getting worse was about 10 months, compared with 5 months in the chemotherapy group. People who received T-DXd survived for a median of 23.4 months overall, while those in the chemotherapy group survived for a median of 16.8 months.
The numbers were similar when the researchers looked specifically at study participants who had hormone receptorpositive disease.
Don’t Miss: Does Itchy Breast Mean Cancer
Treatment Sequencing Beyond Progression On T
The results of the DESTINY-Breast01 phase II trial yield encouraging results, demonstrating impressive response rates and PFS in an extensively pretreated patient population with advanced HER2 positive breast cancer. Depending on results from future phase III trials, T-DXd may claim an emerging role vying for a position as standard third-line therapy. There were important safety concerns however, and as more patients are receiving trastuzumab, pertuzumab and T-DM1 in the neoadjuvant and adjuvant settings T-DXd may move into earlier lines of therapy and expose even greater numbers of patients to its toxicities. It is important to interpret the results of the DESTINY-Breast01 study in the context of other trials conducted in similar populations of patients, of which the HER2CLIMB, NALA, and SOPHIA trials are the most notable.
Ema Accepts Type Ii Application For Trastuzumab Deruxtecan For Previously Treated Her2
In Partnership With:
The European Medicines Agency has validated a Type II Variation application for trastuzumab deruxtecan as monotherapy for adults with unresectable or metastatic HER2-low breast cancer.
The European Medicines Agency has validated a Type II Variation application for fam-trastuzumab deruxtecan-nxki as monotherapy for adults with unresectable or metastatic HER2-low breast cancer. Daiichi-Sankyo announced the move in a press release June 22, 2022.1
Validation confirms that the application is complete and commences the scientific review process by the EMAs Committee for Medicinal Products for Human Use . A Type II variation represents a major change to a drugs marketing authorization that may have a significant impact on the quality, safety or efficacy of a medicine, but does not involve a change to the active substance, strength, or method of administration. Such a change requires a formal approval.2 The CHMP typically releases an opinion, or requests more information on a Type II application, 60 days after initiating the evaluation.3
The HER2-directed antibody drug conjugate would be available for patients who have received systemic therapy in the metastatic setting or who developed disease recurrence during or within 6 months of completing adjuvant chemotherapy. Those with hormone receptor positive breast cancer must also have received or be ineligible for endocrine therapy.
Read Also: What Are The Main Signs Of Breast Cancer
Data Collection And Outcomes
We collected the following clinicopathological characteristics at baseline: age, ECOG-PS at diagnosis, gender, menopausal status, blood counts, histological subtypes, TNM and histoprognostic factors determined by biopsy. After surgery, assessment of pCR , TNM, and histoprognostic factors determined on the resected specimen were collected, as well as data concerning treatments and follow-up . The primary objective of this study was to evaluate pCR rates according to HER2-low status. Secondary objectives were to assess disease free survival , i.e., the time between the diagnosis to the date of any clinical or radiological relapse, overall survival , i.e., the time between the diagnosis to death from any cause , according to HER2-low status , to explore the prognostic value of the neutrophil to lymphocyte ratio defined as the absolute neutrophil count divided by the absolute lymphocyte count pre-chemotherapy, and to analyze the safety.
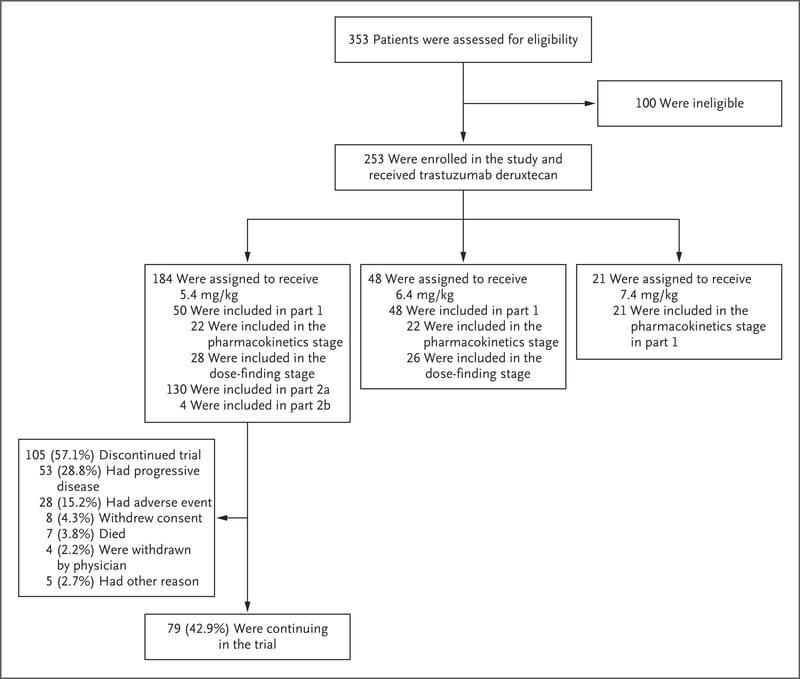
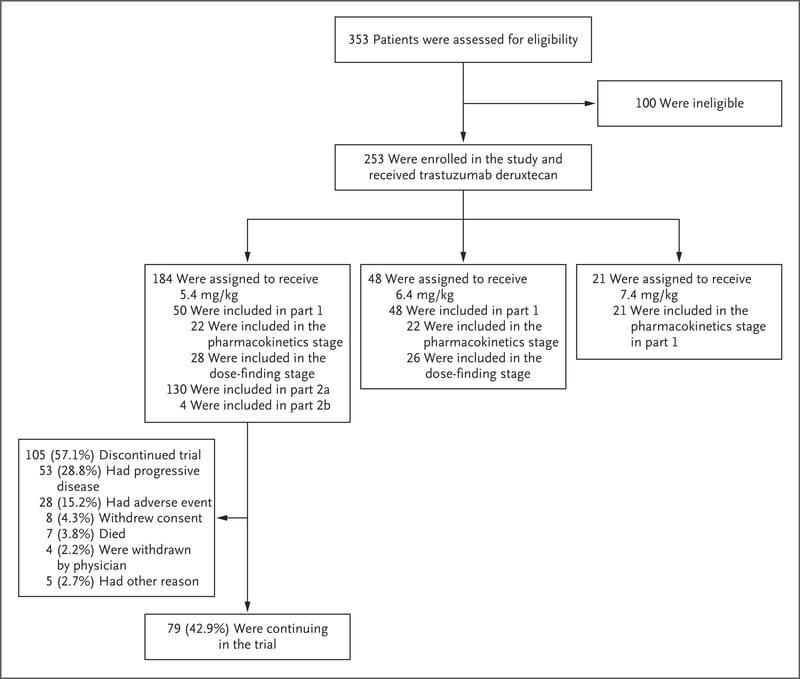
Study Design And Population
We conducted a retrospective bicentric study which enrolled all HER2-low early BC patients treated with NAC at the Comprehensive Cancer Centers François Baclesse and Oscar Lambret . Patients had to meet the following inclusion criteria: age18 years, with histologically proven invasive HER2-low BC, and who received NAC followed by surgery. HER2 expression was classified according to ASCO guidelines . HER2-low status was defined as HER2 IHC score of 1+or 2+without amplification by FISH/ISH testing. We excluded patients with HER2 score 0 and HER2 positive BC , those who received neoadjuvant endocrine therapy, those who did not receive the complete planned chemotherapy regimen and those who did not undergo surgery. HR were assessed by IHC on pretreatment biopsy. Tumors were defined as HR positive if estrogen receptor and/or progesterone receptor nuclear staining was positive in10% of tumor cells.
Recommended Reading: Her 2 Negative Breast Cancer
Trastuzumab Deruxtecan Receives Eu Approval For Previously Treated Unresectable/metastatic Her2+ Breast Cancer
European patients with unresectable or metastatic HER2-positive breast cancer are now able to receive treatment with trastuzumab deruxtecan following 1 or more previous anti-HER2 regimens.
The European Commission has granted approval to fam-trastuzumab deruxtecan-nxki as a treatment for patients with unresectable or metastatic HER2-positive breast cancer after 1 or more prior lines of anti-HER2 therapies, according to a press release from developer AstraZeneca and Daiichi Sankyo.1
The approval was based on findings from the phase 3 DESTINY-Breast03 trial , which reported that the agent yielded a 72% reduction in risk of disease progression or death compared with trastuzumab emtansine .2 At 12 months, the overall survival rates were 94.1% in patients in the trastuzumab deruxtecan arm and 85.9% in those in the T-DM1 arm . Moreover, the overall response rate in either arm was 79.7% vs 34.2%, respectively.
Inclusion And Exclusion Criteria
Inclusion criteria were as follows: 1) clinical trials in any phase using DS-8201a as main strategy 2) patients were with HER2-positive solid tumors 3) the reported results included sufficient information of AEs and survival condition. Exclusion criteria was that studies: 1) in forms of review articles, laboratory articles, meta-analysis, or letters 2) using other curing strategies without using DS-8201a alone 3) without sufficient information about the survival or AEs of patients 4) not in English version. Two authors selected articles independently and a third author with more experience was responsible for resolving divergences.
Read Also: Breast Cancer Walk Pittsburgh 2022
What Does Progress Mean
Graff noted that although the agents have a place, it is not fully transparent. Approved therapies such as trastuzumab deruxtecan and tucatinib keep fighting to move earlier and earlier I am lucky to practice in an environment where I have those agents on trials in those settings and were seeing patients stay on them longer. Graff added that this raises the question about what to do with T-DM1.
If I am moving trastuzumab deruxtecan earlier in my portfolio of treatment, when am I putting T-DM1 back in the sequence? Because of the pattern of visceral metastasis and brain metastasis, is hard to know if patients with HER2-positive disease are going to get fifth, sixth, or seventh line of therapy especially after heavy pretreatment, and long durations of therapy with effective HER2 ADCs. After these agents, Graff added, she would pick among neratinib, lapatinib, and margetuximab-cmkb as her next line of therapy. The answer is somewhere in the data, she said. I am choosing based on the medications we are using in combination and the toxicity profile relative to the patient as well as their risk of AEs.
As for whats next, Traina said, I hopefully will be on a panel in a couple of years reporting out data from new agents, but its tough for the new agents that are being explored because they are designed to treat individuals who have previously seen drugs such as trastuzumab, trastuzumab deruxtecan, or tucatinib. Its going to be a high bar to show benefit there.
Challening The Second Line
Following disease progression, the traditional approach to care was ado-trastuzumab emtansine .2 Findings from the phase 3 EMILIA trial demonstrated that the ADC outperformed capecitabine and lapatinib in patients with HER2positive, metastatic breast cancer who previously received trastuzumab and a taxane. However, after impressive data brought fam-trastuzumab deruxtecan-nxki to the third and later lines of therapy, the natural next step was to test the agents efficacy against the long-standing standard of care in the second line.
T-DM1 was the first drug to take that mantle, Vijayakrishna Gadi, MD, PhD, said. Recently, weve got these exciting data with the trastuzumab deruxtecan in that space, a randomized clinical trial comparing trastuzumab deruxtecan to T-DM1. If you recall, that had 22 zeros in the P value . When was the last time we saw a drug approval trial with 22 zeros? Investigators of DESTINY-Breast03 pitted T-DM1 head-to-head with trastuzumab deruxtecan among 524 randomly assigned patients. The 12-month progression-free survival rate was 75.8% with trastuzumab deruxtecan compared with 34.1% with T-DM1 .3 There were superior PFS data, and a hint of an OS already, although events are still occurring, Gadi said, adding that safety data presented at the 2022 ASCO meeting showed that different analyses reflect another avenue for success with the newcomer.
Read Also: Can You Get Breast Cancer At 22
Trastuzumab Deruxtecan Shows Survival Improvement In Her2
Findings from the phase 2 DESTINY-Breast02 show that trastuzumab deruxtecan improves both progression-free and overall survival in patients with HER2-positive unresectable and/or metastatic breast cancer.
Trastuzumab deruxtecan demonstrated a statistically significant improvement in progression-free survival compared with physicians choice of therapy in patients with HER2-positive unresectable and/or metastatic breast cancer previously treated with trastuzumab emtansine .1
Results show that the phase 2 DESTINY-Breast02 met its primary end point. The key secondary end point of improvement in overall survival was also met, according to an announcement by AstraZeneca. The data builds on the efficacy and trastuzumab deruxtecan in patients with HER2-positive breast cancer.
The top-line results from DESTINY-Breast02 confirm the robust progression-free survival seen in previous trials of Enhertu and enrich our clinical understanding of the benefit this therapy may offer patients with HER2-positive metastatic breast cancer, said Ken Takeshita, Global Head, R& D, Daiichi Sankyo, in a press release. As this is the confirmatory trial for our current breast cancer indication in Europe and several other countries, we look forward to sharing these findings with regulatory authorities to add to the body of data for Enhertu for the treatment of HER2-positive metastatic breast cancer.
REFERENCES:
Response To Neoadjuvant Chemotherapy
The majority of patients received a sequential combination of anthracyclines and taxanes as NAC 114 patients underwent total mastectomy and 115 underwent conservative breast surgery. Sentinel lymph node dissection was performed in 134 patients and axillary lymph node dissection in 89 patients . There were no differences in the treatment approaches between the two centers. Assessment of the pathological response to NAC was available according to the Sataloff classification or RCB score for 224 tumors. pCR was achieved in 38 tumors , of which 24 were HER2 score 1+and 14 were HER2 score 2+.
Table 3 Response to neoadjuvant chemotherapy and survival according to HER2 status
You May Like: Do You Gain Weight With Breast Cancer
Monitoring For Potentially Serious Lung Inflammation
The rates of side effects seen with T-DXd and chemotherapy were similar. The most common severe side effects of T-DXd were reduced levels of white and red blood cells and fatigue.
T-DXd can also cause a potentially serious type of lung inflammation called interstitial lung disease. In DESTINY-Breast04, 45 people in the T-DXd group developed this side effect, and 3 died as a result. By contrast, only one person in the chemotherapy group developed this lung condition and it was mild.
Patients receiving T-DXd must be carefully monitored and promptly treated if they develop signs of lung inflammation, Dr. Modi said.
Because oncologists are already using T-DXd to treat some women with breast cancer, they are now more aware of this possible complication and know so much more about how to diagnose it earlier and how to treat it better, said oncologist Patricia LoRusso, D.O., Ph.D., of Yale Cancer Center, who was not involved with the study.
This knowledge, Dr. LoRusso said, has cut the rate of severe interstitial lung disease seen in people treated with T-Dxd since the drug first came into use a few years ago.
Trastuzumab Deruxtecan In Previously Treated Her2
DESTINY-Breast04 is the first phase III trial of a HER2-directed therapy, trastuzumab deruxtecan, in patients with HER2-low metastatic breast cancer to show a statistically significant and clinically meaningful benefit in PFS and OS compared to standard-of-care treatment, regardless of HR status, with a manageable safety profile.
HER2-low metastatic breast cancer is defined by a score of 1+ on immunohistochemical analysis or as an ICH score of 2+ and negative results on in situ hybridisation. These HER2-low tumours represent a heterogeneous population with a high prevalence of hormone receptor co-expression and without distinct biology. HER2-low mBC is often treated as HER2-negative mBC, with limited options for later lines of treatment. Current HER2-targeted therapies are not effective for patients with tumours that express lower levels of HER2, highlighting the need for more effective drugs. Trastuzumab deruxtecan is a next-generation antibodydrug conjugate consisting of a humanised anti-HER2 monoclonal antibody linked to a topoisomerase I inhibitor payload through a tetrapeptide-based cleavable linker. Results from phase I and phase II studies have shown promising results in heavily pre-treated patients with HER2-low mBC. Therefore, the phase III DESTINY-Breast04 was set up to evaluate the efficacy and safety of T-DXd as compared with the physicians choice of chemotherapy in patients with HER2-low metastatic breast cancer.
Read Also: How Long Does Radiation Treatment Last For Breast Cancer
Case Scenario: Brain Metastases
Approaches to brain metastases, as Gradishar pointed out, are not cut-and-dried and may require a multidisciplinary approach to care.
In a case scenario, Seidman posed: At the time of progression there is suspicion of CNS disease in a patient who has progressed on trastuzumab deruxtecan as her second-line regimen after having had CLEOPATRA therapy in the first line. On an MRI she had 2 subcentimeter lesions and it is not clear if they were causing her symptoms. Youre going to send her for stereotactic radiation. Are you going to try HER2CLIMB and see whether you get a CNS response in the asymptomatic oligometastatic patient? Are you going to give T-DM1?
Gadi noted that if there were disease control below the neck, he would retain the previous agent and target the CNS metastases with stereotactic radiosurgery. If she is progressing below the neck and above the neck, thats frightening because below the neck progression is strongly correlated with additional brain metastases, he said. Maybe target the CNS directly with stereotactic surgery and radiosurgery and then move on to the HER2CLIMB regimen for that patientor, even better, if we have a clinical trial to explore some combinations in that setting, I might do both.
New Methods Of Assessing Her2 Levels Are Needed
With additional HER2-targeted antibodydrug conjugates expected to become available in the coming years, we must also rethink novel, more accurate and sensitive ways of assessing HER2 status, Dr. LoRusso said in formal comments after Dr. Modis presentation of the study findings.
She noted that a recent study found that pathologists did not always agree when it came to distinguishing between HER2-low and HER2-negative breast cancers using immunohistochemistry. Researchers are developing new tests that can detect lower HER2 levels, she said, but these are not yet ready for use in everyday patient care.
We need to reevaluate how we classify the HER2 content of tumors in terms of what treatment to offer patients, Dr. Zimmer said. And its not clear yet what the lower end of the new HER2-low designation will be, she noted.
Other issues for future study include figuring out how T-DXd compares with other targeted drugs used to treat metastatic HER2-low cancers, such as those that block the activity of CDK4 and CDK6 proteins on cancer cells, she said. Ideally, clinical trials are needed to answer which one is best and clarify the order in which they should be offered to patients.
In addition, Dr. LoRusso said, Despite phenomenal and responses to T-DXd, metastatic breast cancer eventually does progress, and its important to understand why tumors stop responding.
Don’t Miss: Can Breast Cancer Lumps Be Itchy