How Common Are Breast Cancer Gene Mutations
Breast cancer gene mutations arent common in the general population, Dr. Eng says, but they are common in people who have breast cancer. About 10% to 15% of people with breast cancer have one of the breast cancer gene mutations.
You can inherit these gene mutations from either of your biological parents, and the cancers theyre linked to can affect both men and women so consider all your relatives when thinking about your family history.
Who Should Be Tested For Hboc
Most breast and ovarian cancers occur by chance with no known cause, so testing for BRCA1 or BRCA2 gene mutations may not be beneficial for the average person. Genetic testing is recommended primarily for people who have a personal and/or family history that suggests HBOC. However, women younger than 60 with triple-negative breast cancer , are at risk of having a BRCA mutation, regardless of family history.
For women with a previous diagnosis of breast cancer or ovarian cancer and/or a family history of breast or ovarian cancer, the National Comprehensive Cancer Network provides recommendations for when genetic counseling and testing may be needed. These recommendations are based on your familys history of cancer and how closely related you are to the person who developed cancer. Here are some important definitions to know:
-
“First-degree relatives” include parents, siblings, and children.
-
“Second-degree relatives” include aunts/uncles, grandparents, grandchildren, and nieces/nephews.
-
“Third-degree relatives” include first cousins, great-grandparents, or great-grandchildren.
Genetic testing should be considered if a person or family meets 1 or more of the criteria listed below:
What Are The Screening Options For Hboc
Screening is the use of different tests to find specific types of cancer before signs and symptoms appear. It is important to talk with your health care team about the following screening options, as each person is different:
Screening for women with a BRCA1 or BRCA2 gene mutation
-
Monthly breast self-examinations, beginning at age 18
-
Clinical breast examinations performed twice a year by a health care team or nurse, beginning at age 25
-
Yearly magnetic resonance imaging scans of both breasts, between ages 25 and 29.
-
Yearly mammogram and breast MRI, between ages 30 and 75.
-
Pelvic examination, trans-vaginal ultrasound, and CA-125 blood test every 6 months, beginning at age 30 to 35. It should be noted, however, that screening is not yet able to find most early ovarian cancers.
-
Consideration of prophylactic salpingo-oophorectomy, between ages 35 and 40, and once a woman is done giving birth to children
Screening for men with a BRCA1 or BRCA2 gene mutation
Screening options may change over time as new methods are developed and more is learned about HBOC. Talk with your health care team about appropriate screening tests for you.
Learn more about what to expect when having common tests, procedures, and scans.
Don’t Miss: Can You Beat Metastatic Breast Cancer
What Other Cancers Are Linked To Harmful Variants In Brca1 And Brca2
Harmful variants in BRCA1 and BRCA2 increase the risk of several additional cancers. In women, these include fallopian tube cancer and primary peritoneal cancer , both of which start in the same cells as the most common type of ovarian cancer. Men with BRCA2 variants, and to a lesser extent BRCA1 variants, are also at increased risk of breast cancer and prostate cancer . Both men and women with harmful BRCA1 or BRCA2 variants are at increased risk of pancreatic cancer, although the risk increase is low .
In addition, certain variants in BRCA1 and BRCA2 can cause subtypes of Fanconi anemia, a rare syndrome that is associated with childhood solid tumors and development of acute myeloid leukemia . The mutations that cause these Fanconi anemia subtypes have a milder effect on protein function than the mutations that cause breast and ovarian cancer. Children who inherit one of these variants from each parent will develop Fanconi anemia.
Should I Have Genetic Screening
You should consider talking to a genetic counselor if your family history includes one or more of the following:
- A diagnosis of triple-negative breast cancer before age 60
- Multiple people in the family with the same cancer or related cancers, such as breast and ovarian or colon and uterine
- Two or more relatives with the same cancer type, such as breast cancer or colorectal cancer, especially if they were diagnosed at younger ages
- A cancer diagnosis at an early age
- More than one primary cancer in an individual
- Occurrence of a rare cancer, such as ovarian cancer or male breast cancer
- Occurrence of a cancer in a person not exposed to a known risk factor, such as lung cancer in a nonsmoker
- A known cancer gene mutation in the family
You May Like: What To Get Someone With Breast Cancer
What A Positive Result Means
If your predictive genetic test result is positive, it means you have a faulty gene that raises your risk of developing cancer.
It does not mean you are guaranteed to get cancer your genes only partly influence your future health risks. Other factors, such as your medical history, lifestyle and your environment, also play a role.
If you have one of the faulty BRCA genes, there is a 50% chance you will pass this on to any children you have and a 50% chance that each of your siblings also has it.
You may want to discuss your results with other members of your family, who may also be affected. Staff at the genetics clinic will discuss with you how a positive or negative result will affect your life and your relationships with your family.
You can read more about BRCA1 and BRCA2 in the beginner’s guide to BRCA1 and BRCA2 produced by The Royal Marsden NHS Foundation Trust.
Insurance companies cannot ask you to disclose the results of predictive genetic tests for the majority of policies, but this may change in the future.
What Is A Gene
Each persons DNA contains the code used to build the human body and keep it functioning. Genes are the small sections of DNA that code for individual traits. For example, someone with naturally red hair has a gene that causes his or her hair to be red.
All inherited traits are passed down through genes. Each person has two copies of every gene: one gene from each parent. Since each parent passes down exactly half of their genes to each child, any of the parents genetic traits has a 50% chance of being passed on to their offspring.
Don’t Miss: Will Breast Cancer Cause Breast To Shrink
Brca1 And Brca2 Inherited Gene Mutations
Like other inherited gene mutations, BRCA1 and BRCA2 gene mutations are rare in the general population. In the U.S., about 1 in 400 people have a BRCA1/2 mutation .
People of all races and ethnicities can have BRCA1/2 inherited gene mutations. However, the proportion of people who have a BRCA1/2 gene mutation varies by ethnic group. Among Ashkenazi Jewish men and women, about 1 in 40 have a BRCA1/2 mutation .
What Are Brca1 And Brca2
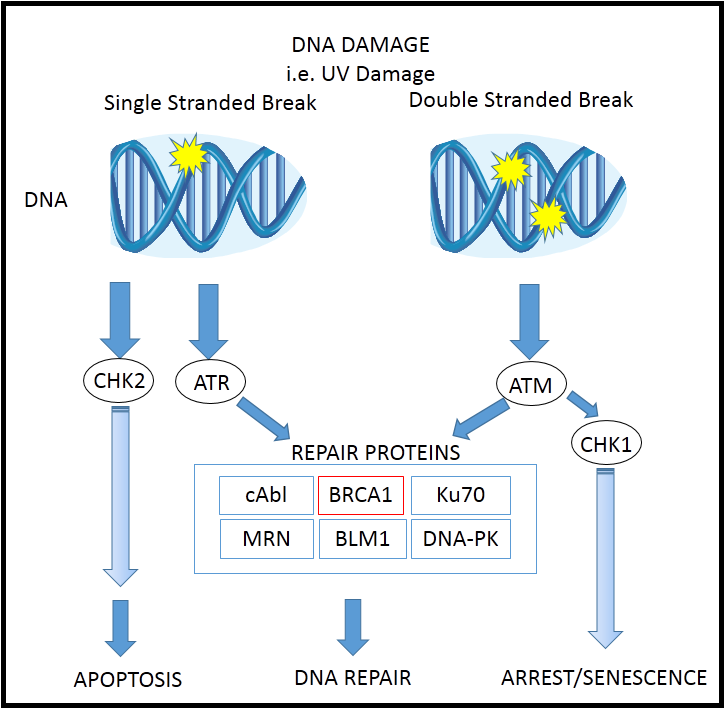
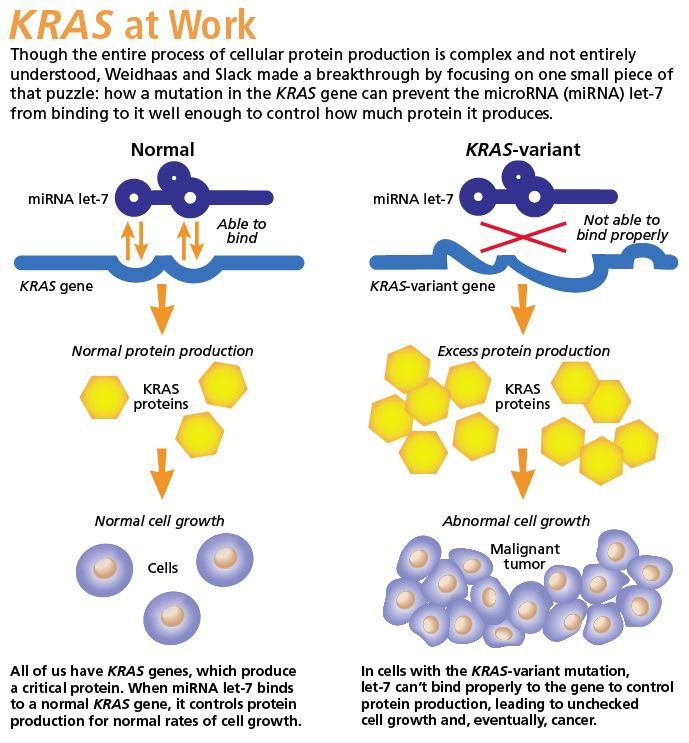
BRCA1 and BRCA2 are genes that produce proteins that help repair damaged DNA. Everyone has two copies of each of these genesone copy inherited from each parent. BRCA1 and BRCA2 are sometimes called tumor suppressor genes because when they have certain changes, called harmful variants , cancer can develop.
People who inherit harmful variants in one of these genes have increased risks of several cancersmost notably breast and ovarian cancer, but also several additional types of cancer. People who have inherited a harmful variant in BRCA1 and BRCA2 also tend to develop cancer at younger ages than people who do not have such a variant.
A harmful variant in BRCA1 or BRCA2 can be inherited from either parent. Each child of a parent who carries any mutation in one of these genes has a 50% chance of inheriting the mutation. Inherited mutationsalso called germline mutations or variantsare present from birth in all cells in the body.
Even if someone has inherited a harmful variant in BRCA1 or BRCA2 from one parent, they would have inherited a normal copy of that gene from the other parent . But the normal copy can be lost or change in some cells in the body during that persons lifetime. Such a change is called a somatic alteration. Cells that dont have any functioning BRCA1 or BRCA2 proteins can grow out of control and become cancer.
Don’t Miss: Can You Get Breast Cancer If You Have Breast Implants
What To Do If You’re Worried
Speak to a GP if cancer runs in your family and you’re worried you may get it too. They may refer you to a local genetics service for an NHS genetic test, which will tell you if you have inherited one of the cancer risk genes.
This type of testing is known as predictive genetic testing. It’s “predictive” because a positive result means you have a greatly increased risk of developing cancer. It does not mean you have cancer or are definitely going to develop it.
You may be eligible for this NHS test if the faulty gene has already been identified in one of your relatives, or if there is a strong family history of cancer in your family.
Having Dense Breast Tissue
Breasts are made up of fatty tissue, fibrous tissue, and glandular tissue. Breasts appear denser on a mammogram when they have more glandular and fibrous tissue and less fatty tissue. Women with dense breasts on mammogram have a higher risk of breast cancer than women with average breast density. Unfortunately, dense breast tissue can also make it harder to see cancers on mammograms.
A number of factors can affect breast density, such as age, menopausal status, the use of certain drugs , pregnancy, and genetics.
To learn more, see our information on breast density and mammograms.
Also Check: Is Painful Lump In Breast Cancer
Detection Of Large Genomic Rearrangement Using Copy Number Variation Analyses
Coverage or read depth has been used to detect CNVs in genome-scale datasets. Multiplex PCR-based enrichment focuses sequencing efforts on a very small fraction of the genome, and the observed read depth for each of the regions can differ due to varying number of PCR amplicons, sequence variation, or PCR enrichment efficiency. For CNV detection in our PCR-enriched amplicon sequencing data of the 20 genes, we used two algorithms, Quandico and ONCOCNV , specifically developed for CNV analysis of amplicon sequencing data. The CNVs detected with these algorithms were then verified experimentally using the multiplex ligation-dependent probe amplification technique. This analysis resulted in the discovery of two carriers of a BRCA1 large genomic rearrangement in the study cohort.
Questions To Ask The Health Care Team
If you are concerned about your risk of cancer, talk with your health care team. It can be helpful to bring someone along to your appointments to take notes. Consider asking your health care team the following questions:
-
What is my risk of developing breast cancer and ovarian cancer?
-
What is my risk for other types of cancer?
-
What can I do to reduce my risk of cancer?
-
What are my options for cancer screening?
If you are concerned about your family history and think your family may have HBOC, consider asking the following questions:
-
Does my family history increase my risk of breast cancer, ovarian cancer, or other types of cancer?
-
Should I meet with a genetic counselor?
-
Should I consider genetic testing?
Don’t Miss: What Is The Prognosis For Breast Cancer
Significance Of Gene Sets
Group CaMP
For each group of genes we determined the total number of mutations observed for the tissue of interest, as well as the number of base pairs that were successfully sequenced. We then computed the P-value as the probability of a group having at least as many mutations as were observed, given the numbers of base pairs sequenced and the background passenger frequencies, using the binomial distribution in R . The background passenger frequencies were conservatively estimated as the total numbers of mutations observed in each tumor type in Sjöblom et al. divided by the total number of base pairs sequenced in the study . The P-values were then corrected for multiple comparisons according to the method described by Benjamini and Hochberg with an FDR of 10%. The Group CaMP score is the negative log of the corrected P-value.
CaMP GSEA
Considerations For Genetic Testing
If you meet any of the criteria that increases your risk of having BRCA1 or BRCA2 mutations, as listed above, you may be considering genetic testing.
Genetic testing for BRCA1 or BRCA1 is usually a simple blood or saliva test. After a conversation and a prescription from a doctor, youll have a sample of your blood or saliva drawn and sent to a lab. The lab looks for the mutations, and the doctor will call you with the results.
You can also pay a direct-to-consumer company to do the test without a referral from your doctor. But these tests only test for BRCA1 and BRCA2 gene mutations. They cant rule out any and all factors that could increase your risk of breast cancer.
If youre curious about other genetic mutations that you may have, youll need to speak with a doctor about getting tested for those mutations, too.
The National Comprehensive Cancer Network offers criteria for who should consider getting a genetic test for BRCA1 and BRCA2 mutations, in addition to other gene mutations including those discussed above. Just know that insurance may not always cover genetic testing.
Currently, these tests arent seen as necessary or recommended for the general public. Genetic testing is only recommended if you have a family history of breast cancer or ovarian cancer.
Children under age 18 are
Don’t Miss: Do Bras Cause Breast Cancer
Finding The Other Mutations
The researchers measured DNA at over 10 million sites across the genome, said professor Peter Kraft of Harvard T.H. Chan School of Public Health, a study author.
At each of these sites, we asked whether the DNA sequence in women with breast cancer was different than that in women without, said Kraft. Because our study was so large, we could detect subtle differences between these two groups of women and be sure these differences were not due to chance.
According to Jacques Simard, a study author and professor and researcher at Université Laval, Quebec City, the newly discovered mutations only slightly by anywhere from 5% to 10% increase a womans risk of developing breast cancer.
But even though, individually, these mutations dont have as big as an effect as BRCA1 and BRCA2 defects, there are many of them, so their overall contribution is larger, said Easton. An individual woman, then, may have two or more of these common smaller risk gene mutations, and so her risk for developing breast cancer increases due to their combined effects.
Kraft noted that taken together, these risk variants may identify a small proportion of women who are at 3-times increased risk of breast cancer. Women found to have a number of these smaller risk genetic mutations, then, would likely benefit from earlier mammography screening.
Risk Factors For Hereditary Breast Cancer
Knowing your potential risk for HBOC can help you and your healthcare professional make better, more informed decisions about your health, before the onset of cancer or before a second cancer has had a chance to develop. Genetic testing for hereditary breast and ovarian cancer with the Myriad Genetics MyRisk Hereditary Cancer panel should be considered if:*
You:
- Have had breast cancer at age 50 or younger
- Have had triple negative breast cancer
- Have ever had ovarian cancer
- Are male and have had breast cancer at any age
- Have had a male relative diagnosed with breast cancer
- Are of Ashkenazi Jewish descent and have a personal or family history of breast, ovarian, prostate or pancreatic cancer
Your Family
- Has had someone diagnosed with breast cancer before age 50
- Has had someone diagnosed with ovarian cancer
- Has had two breast cancers in the same person or on the same side of the family
- Has had a male family member diagnosed with breast cancer
- Has had someone diagnosed with triple negative breast cancer at any age
- Has three or more family members with HBOC-associated** cancer on the same side of the family
- Has had a previously identified BRCA1, BRCA2 or other mutation in the family
Also Check: What Are The Chances Of Her2 Positive Breast Cancer Returning
Study Participants And Data Collection
Koo Foundation Sun Yat-Sen Cancer Center treats over 1000 newly diagnosed breast cancer patients annually. Between July 30, 2015 and March 31, 2016, we enrolled 480 individuals fulfilling at least one of the six eligibility criteria: family history of breast or ovarian cancer at any age , personal history of breast cancer with age of diagnosis less than or equal to 40, bilateral breast cancer diagnosed at the same time or sequentially, triple negative breast cancer, breast and ovarian cancer in the same individual, and male breast cancer. None of the participants had known mutation status in any cancer susceptibility genes prior to enrollment. Clinical information was collected through participant surveys, electronic medical records, and the institutional breast cancer database.
Evaluation Of Suspected Hereditary Predisposition To Breast Cancer
Individuals with a family and personal history suspicious for a familial syndrome should be referred to a genetic counselor for a comprehensive evaluation. Testing for mutations in cancer-associated genes is individually based, and requires a high index of suspicion for a particular gene based on the clinical situation. In general, when a family history is suggestive, it is best to test the individual with a cancer diagnosis, as this increases the probability of a positive test result. Standard clinical BRCA1 and BRCA2 testing has been carried out using PCR amplification and Sanger sequencing. For the Ashkenazi Jewish population, testing can be initially targeted to the three major founder mutations. In 2007, testing for large rearrangements was added for secondary analysis after research studies published that 6%18% of individuals who are BRCA mutation negative by sequencing can be explained by large insertions and deletions in the BRCA1 and BRCA2 genes using multiplex ligation-dependent probe amplification technology . If a mutation is identified, targeted testing can be done for other members of the family to assess risk. Possible outcomes of genetic testing are a true positive, a true negative , uninformative , or a variant of unknown significance . By definition, a VUS is a detected genetic change without a good description of any correlating clinical risk.
You May Like: What Is Grade 0 Breast Cancer