Her2 Breast Cancer Statistics Prognosis & Survival Rate
The incidence of HER2 positive breast cancer is significant studies have shown that around twenty percent of breast cancer cases, 1 in 5, have high levels of the HER2 receptor .
HER2+ breast cancer is an aggressive form of breast cancer and the outlook or prognosis for patients who are HER2+ is not so good. This is a disease with a poor prognosis.
Due to its aggressive nature, HER2+ breast cancer carries an increased chance of the disease spreading to other areas of the body away from the breast and also reoccurring. Compared to HER2 negative breast cancer, HER2+ breast cancer has a reduced life expectancy .
For example, studies suggest that a woman diagnosed with early stage HER2 positive breast cancer has a 68% chance of surviving more than 5 years . This is lower than the overall survival rates for early stage breast cancer which range from around 74% to 88% depending on their actual sub stage.
Compared to HER2 negative patients, HER2 positive breast cancer patients have a higher risk of breast cancer reoccurring after diagnosis.
Breast Cancer And Its Classification
Breast cancer is a malignant clonal proliferation of benign breast tissue that continues to pose a significant threat to women across the globe. As of 2013, American women run a 1 in the 8-lifetime risk of breast cancer, up from 1 in 11 during the 1970s . Fortunately, however, we have seen several advancements in the screening, prevention, and treatment of breast cancer throughout the last half-century due to an immense multi-disciplinary effort encompassing the disciplines of researchers, clinicians, pharmaceutical companies, technology, and many others. Of these advancements, breast cancer treatment has debatably seen the most innovation and is a direct consequence of our greater understanding of breast cancers pathophysiological foundations.
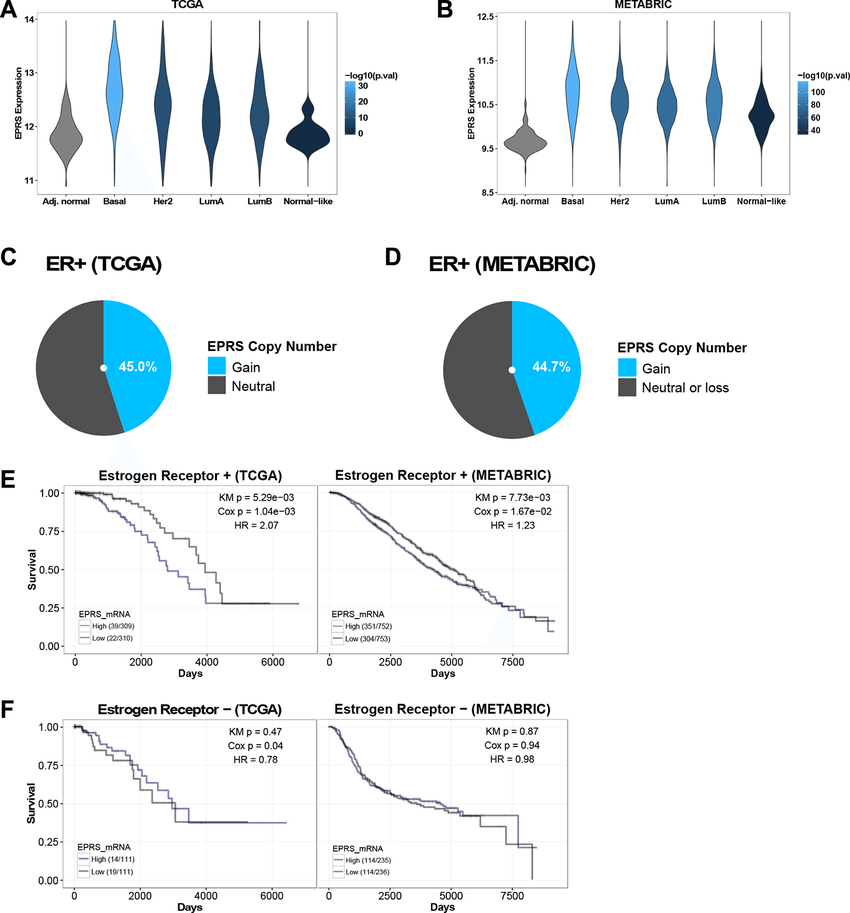
At the time of diagnosis, approximately 90% of breast cancers are not metastatic however, in addition to the 10% metastatic at diagnosis, approximately 10-60% of localized breast cancers develop systemic relapse . Furthermore, the prognosis for ER+ mBC is a median five-year survival rate of 27%, suggesting the need for new therapies that significantly impact progression-free and overall survival in this population . In this article, we aim to briefly describe the history of ER+ mBC treatment, current translational research in development and suggest a theoretically promising molecular therapy combination for future clinical study in ER+ mBC.
Supplementary Figure 3 Clonal Structure And Evolutionary Dynamics Of Uncharacterized Her2 Mutations
Clonal dynamics are shown for three metastatic samples with uncharacterized HER2 mutations by comparing the metastatic clonal cell fraction/CCF to the matched primary CCF . ERBB2 mutations are mapped to metastatic acquired clones in all three patients while not detected in the matched primary . ‘Truncal mutations that are shared between metastatic and primary tumors are found in all patients, demonstrating that the primary and metastatic samples are clonally related . Primary-specific mutations are found in clones that were dominant in the primary tumor but not observed in the metastatic tumor . The phylogenetic relationships among clones are reconstructed for each patient starting from the normal cell connected to the ancestral cancer cells . The phylogenetic divergence of the primary clones and subclones is depicted with blue edges, and that of the metastatic clones and subclones in red. Selected mutations in cancer genes are marked on the corresponding branches of the cancer phylogeny.
Don’t Miss: What Is The Prognosis For Stage 4 Breast Cancer
Clinicopathologic Characteristics Of Single Hormone Receptor
The median follow-up duration for the 6,980 patients included in this analysis was 45 months . In this study, 4,651 cases were double HR+ tumors, 1,758 were double HR- tumors, and 571 cases were single hormone-receptor positive tumors, of which 90 cases were ER-PR+ tumors and 481 were ER + PR- tumors. The clinicopathological characteristics of the four subtypes are summarized in Table . Overall, ER+/PR- tumors were found more frequently in postmenopausal women than other subtypes . Compared with ER + PR+ tumor, ER + PR- tumors were not significantly different in staging , but ER+PR- tumors exhibited higher nuclear grade , higher Ki-67 level , and higher EGFR and HER2 expression . However, compared with ER-PR- tumors, ER + PR- tumors showed lower stage , lower NG , lower Ki-67 level , lower p53 expression and lower EGFR expression , but there was no difference in HER2 overexpression .
Table 1 Clinicopathologic characteristics of patients with ER + PR+, ER + PR-, ER-PR+ and ER-PR- tumors
ER-PR+ tumors had higher NG , higher Ki-67 level , and higher expression of p53 and EGFR than ER + PR+ tumors. However, compared with ER-PR- tumors, there was no difference in stage or NG . Also, there was no difference in expression of Ki-67 , p53 , EGFR or HER2 .
The Present: Addressing Hormone Resistance Via Molecular Therapies
Since their FDA approval in the latter 20th century, modern hormonal therapies have demonstrated significant PFS for ER+ mBC patients . However, post-diagnosis approximately 30-50% ER+ breast cancer patients on these hormonal therapies acquire resistance, requiring additional or substitutive treatment for the further clinical benefit . Recent research suggests this resistance to occur via the PI3K-AKT-mTOR, CCND1-CDK4/6-RB, BCL2-p53-MDM2, ESR1 and other cell-signaling pathways, demonstrating the potential efficacy of molecular-based therapies in advanced breast cancer.
Despite early successes in molecular targeting of the PI3K-AKT-mTOR pathway, others pursued the molecular targeting of other frequently deregulated pathways in ER+ mBC. The CCND1-CDK4/6-RB pathway, innately vital to cell cycle control, regulates whether a cell advances or arrests at the G1-S phase of the cell cycle. Furthermore, it was estimated that 35% HR+ breast cancers demonstrated amplification in the CCND1, the gene that encodes cyclin-D1, and 16% demonstrated amplification in the gene encoding CDK4, suggesting the theoretical utility of their inhibitors in ER+ mBC therapeutics .
Also Check: What Is The Prognosis For Stage 4 Breast Cancer
What Happens During Er/pr Testing
Your provider will need to take a sample of breast tissue in a procedure called a breast biopsy. There are three main types of breast biopsies:
- Fine needle aspiration biopsy, which uses a very thin needle to remove a sample of breast cells or fluid
- Core needle biopsy, which uses a larger needle to remove a sample
- Surgical biopsy, which removes a sample in a minor, outpatient procedure
Fine needle aspiration and core needle biopsies usually include the following steps:
- You will lay on your side or sit on an exam table.
- A health care provider will clean the biopsy site and inject it with an anesthetic, so you won’t feel any pain during the procedure.
- Once the area is numb, the provider will insert either a fine aspiration needle or core biopsy needle into the biopsy site and remove a sample of tissue or fluid.
- You may feel a little pressure when the sample is withdrawn.
- Pressure will be applied to the biopsy site until the bleeding stops.
- Your provider will apply a sterile bandage at the biopsy site.
In a surgical biopsy, a surgeon will make a small cut in your skin to remove all or part of a breast lump. A surgical biopsy is sometimes done if the lump can’t be reached with a needle biopsy. Surgical biopsies usually include the following steps.
Metformin Trial: This Is It
Arteaga also highlighted CCTGMA.32 , a phase 3 randomized, placebo-controlled adjuvant trial of the diabetes drug metformin vs placebo in early breast cancer. Results of the primary efficacy analysis of the trial will be presented at the meeting.
The Canadian-led study seeks to determine if metformin can decrease breast cancer cell growth and work with cancer therapies to prevent disease recurrence. The study design calls for patients to take twice-daily oral metformin or placebo pills for up to 5 years in the absence of disease progression.
The primary outcome of the 3500-plus patient trial is invasive disease-free survival in hormone receptor negative and positive subgroups.
Metformin has actually been associated with improved survival in patients on chemotherapy. But we dont know exactly how, he said. Theres never been a head-to-head comparison in the adjuvant setting . This is it.
Don’t Miss: What Is Stage 3a Breast Cancer
What Are Estrogen Receptor/progesterone Receptor Tests
Estrogen receptor/progesterone receptor tests are used to help guide breast cancer treatment. Receptors are proteins that attach to certain substances. ER/PR tests look for receptors that attach to the hormones estrogen and progesterone in a sample of breast cancer tissue. Estrogen and progesterone play key roles in a woman’s sexual development and reproductive functions. Men also have these hormones, but in much smaller amounts.
About 70 percent of all breast cancers in women have receptors that attach to estrogen and/or progesterone. About 80 percent to 90 percent of breast cancers in men have these receptors. Breast cancers with estrogen and/or progesterone receptors include the following types:
- ER-positive : Cancers that have estrogen receptors
- PR-positive : Cancers that have progesterone receptors
- Hormone receptor-positive : Cancers that have one or both types of these receptors.
Breast cancers without ER or PR receptors are known as HR-negative .
ER/PR tests will show whether there are ER and/or PR receptors on your breast cancer cells. Test results are frequently referred to as the hormone receptor status. If your hormone receptor status shows you have one or both of these receptors on your cancer cells, you may respond well to certain types of treatments.
Other names: ER/PR IHC testing, hormone receptor status
What This Means For Patients
Because the results of ER and PR testing can make a difference in a persons treatment and chance of recurrence, it’s important that these tests are accurate. This guideline was developed to help both doctors and laboratories know how to improve the accuracy of ER and PR testing for those with breast cancer. Understanding the ER/PR status of the primary tumor and any distant or recurrent tumors can help doctors make sure that patients receive the appropriate treatment and avoid side effects of a treatment that may not work. Use this guideline to talk with your doctor about the accuracy of your ER and PR test results and what that means for your treatment.
Also Check: Invasive Ductal Carcinoma Estrogen Receptor Positive
How To Read Hormone Receptor Test Results
Most testing labs use a special staining process that makes the hormone receptors show up in a sample of breast cancer tissue. The test is called an immunohistochemical staining assay, or ImmunoHistoChemistry . Not all labs use the same method for analyzing the results of the test, and they do not have to report the results in exactly the same way. So you may see any of the following on your pathology report:
- A percentage that tells you how many cells out of 100 stain positive for hormone receptors. You will see a number between 0% and 100% .
- An Allred score between 0 and 8. This scoring system is named for the doctor who developed it. The system looks at what percentage of cells test positive for hormone receptors, along with how well the receptors show up after staining . This information is then combined to score the sample on a scale from 0 to 8. The higher the score, the more receptors were found and the easier they were to see in the sample.
- The word positive or negative.
Keep in mind that a test should be done for both estrogen receptors and progesterone receptors. If your result is reported as just the word positive or negative, ask your doctor for a more definite percentage, rating, or other number. You also can ask about how these more precise results might influence treatment decisions for your particular situation.
Current Status Of Ferroptosis Studies In Breast Cancer
Breast cancer can be divided into several types, including luminal A/B, HER-2 enriched, basal-like and normal-like subtypes. According to NCCN guidelines, endocrine therapy is used for ER-positive breast cancer and anti-HER2 targeted therapy is used for HER2-positive breast cancer. However, there is no targeted therapy for triple-negative breast cancer. Due to the lack of effective endocrine therapy and anti-HER2 targeted therapy, triple negative breast cancer patients are characterized by high recurrence rates and poor prognosis. Recently, some researchers have found that triple-negative breast cancer is more sensitive to ferroptosis than ER positive breast cancer . Therefore, triggering ferroptotic cell death of breast cancer seems to be an effective treatment strategy, especially in triple negative subtype.
Read Also: What Is Stage 3a Breast Cancer
On The Horizon For Advanced Breast Cancer
A very important study of an investigational oral agent employed in heavily pretreated postmenopausal women with estrogen receptorpositive advanced breast cancer headlines the meeting.
This international, multicenter trial could have practice-changing implications, Arteaga told Medscape Medical News.
The phase 3 EMERALD trial pits elacestrant, a selective estrogen receptor degrader , against standard endocrine therapy in patients with metastatic breast cancer whose disease has progressed after treatment with at least one endocrine therapy and a CDK4/6 inhibitor.
The trial is important because many patients with breast cancer have estrogen receptor mutations, which are a major mechanism of resistance and thus progression on earlier therapy, Arteaga said.
Elacestrant is in good company among a plethora of oral SERDs under investigation in advanced breast cancer however, currently, fulvestrant which requires an intramuscular injection in the buttocks every month is the only approved SERD.
Theres plenty of preclinical data that suggest that these drugs may have activity against these mutant forms of the receptor, which occur in up to 40% of patients with advanced ER+ breast cancer, he explained.
Researchers will present data on two primary outcome measures from the phase 3 trial: progression-free survival based on mutations of the estrogen receptor 1 gene and PFS in all subjects regardless of ESR1 status.
All About Er Positive Her2 Negative Breast Cancer

About one in eight women in the United States will develop breast cancer, according to commonly used statistics.
But other reports indicate that breast cancer rates are on the decline, likely because of improved recognition, prevention, and treatment. One advancement is the ability to identify different breast cancer types based on specific molecules found in tumors. The distinction greatly aids in breast cancer treatment selection and helps doctors predict how aggressive cancers will advance.
A crucial step in the process of beast cancer evaluation is testing tumor tissue removed during a biopsy or surgery to determine if it has estrogen and progesterone receptors molecules that the hormones bind to.
Cancerous cells may have none, one, or both receptors. Breast cancers that have estrogen receptors are called ER-positive . Those with progesterone receptors are referred to as PR-positive .
In addition to hormone receptors, some breast cancers have high levels of a growth-promoting protein called HER2/neu. If a tumor has this property, it is called HER2-positive. HER2 positive cancers are more aggressive than HER2 negative cancer.
Knowing breast cancer type, leads doctors to determining best treatments.
HER2 negative cancers will not respond to treatment with drugs that target HER2, such as trastuzumab and lapatinib .
Overall, estrogen receptor-positive breast cancer is treatable, especially when diagnosed early.
Don’t Miss: What Percentage Of Breast Cancer Is Triple Negative
What Is The Life Expectancy For Each Cancer Stage
Your outlook depends on the stage of your cancer when its discovered. Cancer is staged by number, starting with 0 and going to 4. Stage 0 is the very beginning and stage 4 is the last stage, also called the metastatic stage because its when cancer has spread to other areas in the body.
Each number reflects different characteristics of your breast cancer. These include the size of the tumor and whether cancer has moved into lymph nodes or distant organs, like the lungs, bones, or brain.
The cancer subtype doesnt play a role in staging, only in treatment decisions.
Survival statistics of women with the major subtypes of breast cancer such as ER-positive, HER2-positive, and triple-negative are grouped together. With treatment, most women with very early stage breast cancers of any subtype can expect a normal life span.
Survival rates are based on how many people are still alive years after they were first diagnosed. Five-year and 10-year survival are commonly reported.
According to the American Cancer Society, 5-year survival rates are:
- stage 0 100 percent
- stage 3 72 percent
- stage 4 22 percent
One thing to note is that these statistics also included women with the more aggressive HER2-positive and triple-negative cancers. And it takes five years to get to a five-year statistical survival rate, so newer therapies are not included in these numbers.
Its likely that a woman with ER-positive breast cancer diagnosed today may have a higher chance of survival.
Supplementary Figure 1 Spectrum Of Her2 Mutations Observed In Mbc Across Several Studies
HER2 mutations in MBC identified in this study as well as in several recent studies are depicted along the length of the protein. In addition to the current study, we aggregated HER2 mutations observed in MBC in Lefebvre et al. and Yates et al. , as well as the MBC subset from the MET500 study of Robinson et al. , the MBC subset from the MSK-IMPACT compendium of Zehir et al. and the MBC subset from the AACR Project GENIE Consortium V1.0.15 , excluding duplicate patients from MSK-IMPACT. The mutations identified in the current study are highlighted. Among these, P1074L, I628M, R143G, and S653C have not been previously described . G727A, Leu755Ser, V777L, L869R, and R1153L have been observed in MBC in other studies. A more detailed list of the mutations can be found in Supplementary Table .
Read Also: Invasive Breast Cancer Survival Rates