What Genes Are Linked To Breast Cancer
The term breast cancer genes means genes that, when altered , increase your risk of getting breast cancer. These gene mutations shut down some of your natural cancer-fighting genes. When you dont have your full army of genes fending off cancer, your risk of certain cancers goes up.
BRCA1 and BRCA2 are the most common breast cancer genes when mutated, followed closely by PTEN mutations, says Dr. Eng. But several other breast cancer gene mutations exist. We know of at least 14 different genes right now, and we are currently exploring several others, too.
These gene mutations arent limited to breast cancer risk. Some of these gene mutations may also increase the risk of:
What Is Genetic Testing
This type of testing is done to determine if a person has a specific mutation that puts them at a higher risk of developing cancer.
Genetic testing can be done on samples of blood or saliva, or from a swab of the inside of a cheek, according to the American Cancer Society. The samples are sent to a lab for testing.
Genetic testing for cancer is usually done in a doctors office , but there are a few tests available for people to purchase commercially.
Considering Genetic Testing For Breast And Ovarian Cancers
Identifying whether you have an abnormal gene related to breast cancer could help predict what other cancers you might be at risk for, including ovarian cancer. Knowing this information allows your health care providers to recommend strategies to prevent or detect those cancers at an earlier stage. And, if you’ve been diagnosed with breast or ovarian cancer, knowing your genetic status might alter the treatment plan for you.
BRCA Genes
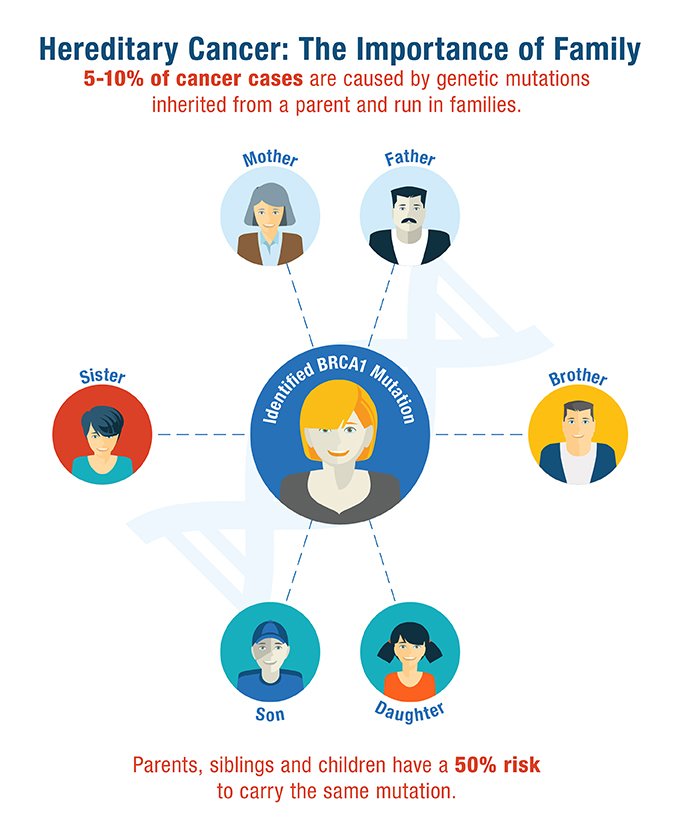
In 10 percent of breast cancer cases, the cancer is caused by an abnormal gene mutation from one of the parents. The most common genes that cause breast cancer are known as BRCA1 and BRCA2. In families where one parent carries one of the genes, there is often at least one woman most often, more who has developed breast cancer before she turned 50. Another clue that a BRCA1 or BRCA2 abnormality exists is the presences of ovarian cancer, male breast cancer, or breast cancer in both breasts.
The mutated gene can be found in any family with the appropriate cancer history, although these mutations are more prevalent in Ashkenazi Jewish families. In Jewish families, genetic testing should be considered for any woman who has two close relatives diagnosed with breast cancer before age 65, or any instance of ovarian cancer.
Hereditary Breast and Ovarian Cancer Syndrome
For women and men with HBOC,
Other Hereditary Breast Cancer Genes
Other, more rare, hereditary cancer syndromes associated with increased risk to develop breast cancer include:
Read Also: What Blood Test Can Detect Breast Cancer
What To Do If You’re Worried
Speak to a GP if cancer runs in your family and you’re worried you may get it too. They may refer you to a local genetics service for an NHS genetic test, which will tell you if you have inherited one of the cancer risk genes.
This type of testing is known as predictive genetic testing. It’s “predictive” because a positive result means you have a greatly increased risk of developing cancer. It does not mean you have cancer or are definitely going to develop it.
You may be eligible for this NHS test if the faulty gene has already been identified in one of your relatives, or if there is a strong family history of cancer in your family.
If Your Risk Is Assessed As Moderate Or High

Consider changing other risk factors for breast cancer as outlined above for women with normal or near-normal risk.
You will be offered a referral to see a doctor who is a specialist. He or she will make a detailed assessment of your risk on the basis of family history.
You may be offered genetic testing and counselling. This is usually done in a specialist genetics clinic. This may involve tests to see if you carry one or more of the faulty genes mentioned above. A blood test may also be taken from your family member who has breast cancer.
Depending on the outcome of the tests and assessment of the risk, some women are offered regular tests such as mammography or MRI scans for screening from an early age. The timing and frequency of any screening tests will depend on your own individual risk.
For a small number of women, whose risk is very high, surgery to remove the breasts and/or ovaries before cancer develops may be an option. This is not an option which is taken lightly and is only done after full risk assessment and counselling.
There are medicines which have also been shown to reduce the risk of breast cancer in women who are at increased risk of the disease.
Recommended Reading: How Likely Am I To Get Breast Cancer
Guidelines For Breast Cancer Screening
Breast cancer screening guidelines for average risk women have become confusing. One organization recommends that women start getting mammograms every other year at age 50 and another recommends yearly mammograms between age 45 and 55 with every other year mammograms thereafter. One reason for these differences is disagreement as to whether annual mammography in younger women can reduce the risk of dying of breast cancer. At Johns Hopkins, we continue to recommend annual mammography beginning at age 40 for average risk women,
Extra screening tests are recommended for women with higher than average risk for breast cancer. Current guidelines suggest that if you have more than a 20% risk of developing breast cancer during your lifetime you should consider adding screening breast MRI to your mammogram. Women who carry mutations in BRCA1, BRCA2, PALB2, or CHEK2 will meet this risk threshold. Other women with family history of breast cancer or a history of a breast biopsy showing high risk changes may meet this criterion as well. You can calculate your breast cancer risk online using the Gail model or the BCSC model . Breast specialists in the Johns Hopkins Breast Center have access to additional resources for calculating your breast cancer risk. At Johns Hopkins enhanced surveillance for high risk women consists of a breast exam every 6 months alternating mammograms with MRI scans.
Are Harmful Variants In Brca1 And Brca2 More Common In Certain Racial/ethnic Populations Than Others
Yes. The likelihood of carrying an inherited mutation in BRCA1 or BRCA2 varies across specific population groups. While the prevalence in the general population is about 0.2%0.3% , about 2.0% of people of Ashkenazi Jewish descent carry a harmful variant in one of these two genes and the variants are usually one of three specific variants, called founder mutations. Other populations, such as Norwegian, Dutch, and Icelandic peoples, also have founder mutations .
Different racial/ethnic and geographic populations also tend to carry different variants in these genes. For instance, African Americans have BRCA1 variants that are not seen in other racial/ethnic groups in the United States . Most people of Ashkenazi Jewish descent in the United States who carry a BRCA variant have one of three specific variants . In the Icelandic population, a different variant in BRCA1 is common among those who inherit a mutation in BRCA1.
Also Check: Did Anne Hathaway Have Breast Cancer
Should I Have Genetic Testing
The decision to undergo genetic testing is a very personal one. There is no right or wrong choice however, genetics is an area of cancer research where knowledge is growing rapidly. It is important to get the most up-to-date information from healthcare providers who are specially trained in cancer genetics when you are making the decision whether to have genetic testing.
Who Should Consider Genetic Counseling And Testing For Brca1 And Brca2 Variants
Anyone who is concerned about the possibility that they may have a harmful variant in the BRCA1 or BRCA2 gene should discuss their concerns with their health care provider or a genetic counselor.
Tests are available to see if someone has inherited a harmful variant in BRCA1 and BRCA2. However, testing is not currently recommended for the general public. Instead, expert groups recommend that testing be focused on those who have a higher likelihood of carrying a harmful BRCA1 or BRCA2 variant, such as those who have a family history of certain cancers. Testing can be appropriate for both people without cancer as well as people who have been diagnosed with cancer. If someone knows they have a mutation in one of these genes, they can take steps to reduce their risk or detect cancer early. And if they have cancer, the information about their mutation may be important for selecting treatment.
Before testing is done, a person will usually have a risk assessment, in which they meet with a genetic counselor or other health care provider to review factors such as which of their relatives had cancer, what cancers they had, and at what ages they were diagnosed. If this assessment suggests that someone has an increased risk of carrying a harmful BRCA1 or BRCA2 gene variant, their genetic counselor can discuss the benefits and harms of testing with them and order the appropriate genetic test, if the individual decides to have genetic testing .
You May Like: Will My Breast Cancer Come Back
Inheriting Certain Gene Changes
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene changes passed on from a parent.
BRCA1 and BRCA2: The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of these genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has up to a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer.
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts.
- Women with one of these gene changes also have a higher risk of developing ovarian cancer and some other cancers.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi origin than in other racial and ethnic groups, but anyone can have them.
Other genes: Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
Mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Questions To Ask The Health Care Team
If you are concerned about your risk of cancer, talk with your health care team. It can be helpful to bring someone along to your appointments to take notes. Consider asking your health care team the following questions:
-
What is my risk of developing breast cancer and ovarian cancer?
-
What is my risk for other types of cancer?
-
What can I do to reduce my risk of cancer?
-
What are my options for cancer screening?
If you are concerned about your family history and think your family may have HBOC, consider asking the following questions:
-
Does my family history increase my risk of breast cancer, ovarian cancer, or other types of cancer?
-
Should I meet with a genetic counselor?
-
Should I consider genetic testing?
Also Check: Is Weight Gain A Symptom Of Breast Cancer
Alterations In Apoptosis Regulation
Dysregulation of apoptosis plays an important role in the pathogenesis and progression of breast cancer, as well as in responses of tumors to therapeutic intervention. Overexpression of BCL2 is commonly observed in estrogen receptor-positive sporadic breast carcinomas and has been associated with a good prognosis. Compared with BCL2, far less is known about the expression of other apoptotic markers in breast tumors in general, and in hereditary cases in particular.
Overexpression of BCL2 in BRCA2 tumors has been reported in several studies, confirming the good correlation between these markers and estrogen receptor status. By contrast, low levels of BCL2 but high levels of caspase 3 were observed in BRCA1 tumors. Caspase 3 is a cytosolic enzyme that is activated only in cells committed to undergoing apoptosis, and is strongly associated with morphological assessment. Thus, previous studies have shown that the apoptotic index obtained by measuring caspase activation was higher in high-grade, estrogen receptor-negative tumors, as has been observed in BRCA1-associated carcinomas. These data are in accordance with an expression study using cDNA microarrays that showed BRCA1-mutation-positive tumors to have increased expression of genes associated with inducing apoptosis , and decreased expression of genes involved in suppressing apoptosis .
Risk Reducing Bilateral Salpingo
Risk reducing bilateral salpingo-oophorectomy is recommended for female BRCA1/2 carriers who have completed childbearing and should be completed by age 35 to 40 for BRCA1, 40 to 45 for BRCA2 carriers or earlier as per patients relevant family history . It has been demonstrated that rrBSO reduces the risk for ovarian cancer by 80% and all-cause mortality by 68% in female BRCA1/2 carriers . The beneficial effect of rrBSO on breast cancer risk reduction has also been assessed but current data are less conclusive. Some prospective studies confirmed that rrBSO reduces BC risk for both BRCA1/2 carriers . However, a large case-control study showed a benefit for rrBSO only for BRCA1 carriers when performed before the age of 40, while a more recent study identified a benefit only for BRCA2 carriers when performed prior to 50 years old . Oophorectomy has been associated with a significant decrease in the risk of IBR and CBC .
Also Check: What Is The Prognosis For Stage 4 Breast Cancer
Hereditary Breast Cancer: The Era Of New Susceptibility Genes
Florentia Fostira
1Molecular Diagnostics Laboratory, INRASTES, National Center for Scientific Research Demokritos, Athens, Greece
Abstract
Breast cancer is the most common malignancy among females. 5%10% of breast cancer cases are hereditary and are caused by pathogenic mutations in the considered reference BRCA1 and BRCA2 genes. As sequencing technologies evolve, more susceptible genes have been discovered and BRCA1 and BRCA2 predisposition seems to be only a part of the story. These new findings include rare germline mutations in other high penetrant genes, the most important of which include TP53 mutations in Li-Fraumeni syndrome, STK11 mutations in Peutz-Jeghers syndrome, and PTEN mutations in Cowden syndrome. Furthermore, more frequent, but less penetrant, mutations have been identified in families with breast cancer clustering, in moderate or low penetrant genes, such as CHEK2, ATM, PALB2, and BRIP1. This paper will summarize all current data on new findings in breast cancer susceptibility genes.
1. Introduction
2. Patient Eligibility
The implementation of hereditary multigene panel testing arises many issues, such as which are the criteria that patients have to meet in order to undergo the test and the patient clinical management. The utilization of the test must be in compliance with the recommendations for genetic testing identified in the ASCO policy .
3. Penetrance
3.1. High-Penetrant Genes
3.1.1. BRCA1
3.1.2. BRCA2
3.1.3. TP53
3.1.4. PTEN
3.1.5. STK11
What Is Hereditary Breast And Ovarian Cancer
A diagnosis of Hereditary Breast and Ovarian Cancer Syndrome is considered when there are multiple cases of breast cancer and/or ovarian cancer on the same side of the family. The chance that a family has HBOC increases in any of these situations:
-
1 or more women are diagnosed at age 45 or younger
-
1 or more women are diagnosed with breast cancer before age 50 with an additional family history of cancer, such as prostate cancer, melanoma, and pancreatic cancer
-
There are breast and/or ovarian cancers in multiple generations on the same side of the family, such as having both a grandmother and an aunt on the fathers side both diagnosed with these cancers
-
A woman is diagnosed with a second breast cancer in the same or the other breast or has both breast and ovarian cancers
-
A male relative is diagnosed with breast cancer
-
There is a history of breast cancer, ovarian cancer, prostate cancer, and/or pancreatic cancer on the same side of the family
-
Having Ashkenazi Jewish ancestry
Recommended Reading: How To Tell If Breast Cancer Has Metastasized
Implications For Genetic Testing
The results presented above on the morphological and immunohistochemical characteristics of hereditary breast cancer illustrate major differences between genotypes. The most important were those between tumors in BRCA1 carriers and all other categories. These histopathological features, in conjunction with clinical data, can be used to predict BRCA1 status and, to a lesser extent, BRCA2 and non-BRCA1/2 status and this could have implications for the process of mutation screening.
In families with a high incidence of breast and ovarian cancer there is a high probability of finding a BRCA1 or BRCA2 germline mutation. In the absence of other clinical features suggesting the alteration of a specific gene, such as prostate cancer and BRCA2 mutations, histopathological features can be used to indicate which gene should be screened first. Grade 3, estrogen receptor- and progesterone receptor-negative infiltrating ductal carcinomas are more common among BRCA1 patients, specially if they show medullary features. These cases should be also tested for CK5/6 and EGFR expression, since the positive staining of any of these makers further increase the probability of being a BRCA1 mutation carrier. Estrogen receptor- and/or progesterone receptor-positive tumors without evidence of basal differentiation should first be tested for BRCA2 mutations.
Pathological Characteristics Of Hereditary Breast Cancer
The majority of invasive breast cancers arising in BRCA1 and BRCA2 carriers are invasive ductal carcinomas . A higher frequency of BRCA1 tumors are classified as medullary carcinomas compared to sporadic tumors ., Medullary carcinomas are poorly differentiated, high-grade carcinomas with diffuse lymphocytic infiltrate but with a remarkably favorable prognosis, probably because of low incidence of lymph node metastasis. Notably, 11% of medullary carcinomas carry BRCA1 germline mutations. By contrast, excess of invasive lobular and tubular carcinomas has been reported for BRCA2 relative to BRCA1 tumors.,BRCA1 tumors are more frequently high-grade compared to sporadic tumors. They have a higher number of mitosis, and show a high frequency of necrotic areas and a higher proportion of continuous pushing margins and lymphocytic infiltration. All these features point toward a more aggressive tumor type., Most BRCA2 tumors are grade 2/3 with high mitotic rates. Continuous pushing margins are also characteristic of BRCA2 tumors.
In contrast to BRCA1 tumors, BRCA2 tumors seem to be more similar to sporadic tumors with relation to the expression of IHC markers. Most BRCA2 breast tumors show a luminal phenotype by overexpressing ER and PR and the cytokeratins CK8 and CK18.
Also Check: Did Anne Hathaway Have Breast Cancer