Assessment Of Risk For Breast Cancer
Various methods are available to identif y women at increased risk for breast cancer, including formal clinical risk assessment tools or assessing breast cancer risk factors without using a formal tool.
Numerous risk assessment tools, such as the National Cancer Institute Breast Cancer Risk Assessment Tool,5 estimate a womans risk of developing breast cancer over the next 5 years. There is no single cutoff for defining increased risk for all women. Women at greater risk, such as those with at least a 3% risk for breast cancer in the next 5 years, are likely to derive more benefit than harm from risk-reducing medications6 and should be offered these medications if their risk of harms is low. Some women at lower risk for breast cancer have also been included in trials documenting reduced risk for breast cancer when taking tamoxifen, raloxifene, or aromatase inhibitors.3,4 However, when balancing the harms associated with these medications, the net benefit will be lower among women at lower risk.
Women not at increased risk for breast cancer, such as women younger than 60 years with no additional risk factors for breast cancer, or women with a low 5-year risk of breast cancer should not be routinely offered medications to reduce risk of breast cancer because the risk of harms from these medications likely outweighs their potential benefit.
Drugs That Block Estrogen
Some drugs work by blocking estrogen from causing cancer cells to grow.
Tamoxifen is a drug that prevents estrogen from telling cancer cells to grow. It has a number of benefits:
- Taking Tamoxifen for 5 years after breast cancer surgery cuts the chance of cancer coming back by half. Some studies show that taking it for 10 years may work even better.
- It reduces the risk that cancer will grow in the other breast.
- It slows the growth and shrinks cancer that has spread.
- It reduces the risk of getting cancer in women who are at high risk.
Other drugs that work in a similar way are used to treat advanced cancer that has spread:
- Toremifene
- Fulvestrant
A Couple Commonly Considered Natural Treatments For Breast Cancer
We understand that you may have concerns about conventional cancer treatment and may be looking for more natural ways to fight cancer. But even natural approaches may be harmful in certain amounts and in certain situations.
Below are two approaches were aware of patients using or considering to treat their breast cancer. Although some may be beneficial in helping you tolerate conventional treatment, there’s no reliable scientific evidence that theyre effective treatments on their own.
Medical marijuana:No scientific studies provide evidence that cannabis or CBD oil can cure, or even treat, cancer, and the NIH notes that the U.S. Food and Drug Administration has not approved cannabis as a medical treatment. FDA approved cannabinoid prescription medications, however, may help treat side effects of cancer and its treatment, such as loss of appetite, neuropathic pain, nausea and vomiting.
Research shows that patients who choose complementary medicine are more likely to delay or reject some types of conventional treatment, which results in worse cancer outcomes. Another study that included women with nonmetastatic breast cancer who initially chose alternative medicine instead of conventional cancer treatment showed those women had more than a fivefold increased risk of death.
Recommended Reading: Is Chemo Always Needed For Breast Cancer
Should A Person Take Hrt
The benefits of taking HRT can vary from person to person. Some people decide that the benefits outweigh the risks.
HRT can help relieve the symptoms of menopause. It can also help reduce the risk of developing osteoporosis.
A person should discuss the benefits and risks with a healthcare professional before deciding whether HRT is right for them.
If a person decides to take HRT, they should attend all their breast cancer screening appointments.
Aromatase Inhibitors Such As Arimidex Femara And Aromasin

Aromatase inhibitors work by blocking the production of estrogen in the body. They are generally reserved for postmenopausal women with breast cancer whose estrogen is primarily produced by the aromatase enzyme. Aromatase inhibitors may be used in premenopausal women if ovarian suppression treatments are also used.
Unlike tamoxifen, aromatase inhibitors have a low risk of causing uterine cancer or blood clots. However, aromatase inhibitors can cause muscle and joint pain, which can lead to some women discontinuing treatment. Because they block the production of estrogen, aromatase inhibitors can cause bone loss in women after menopause.
Common side effects of aromatase inhibitors include vaginal dryness, muscle pain, joint aches, and hot flashes or night sweats.
Also Check: Which Breast Cancer Is Genetic
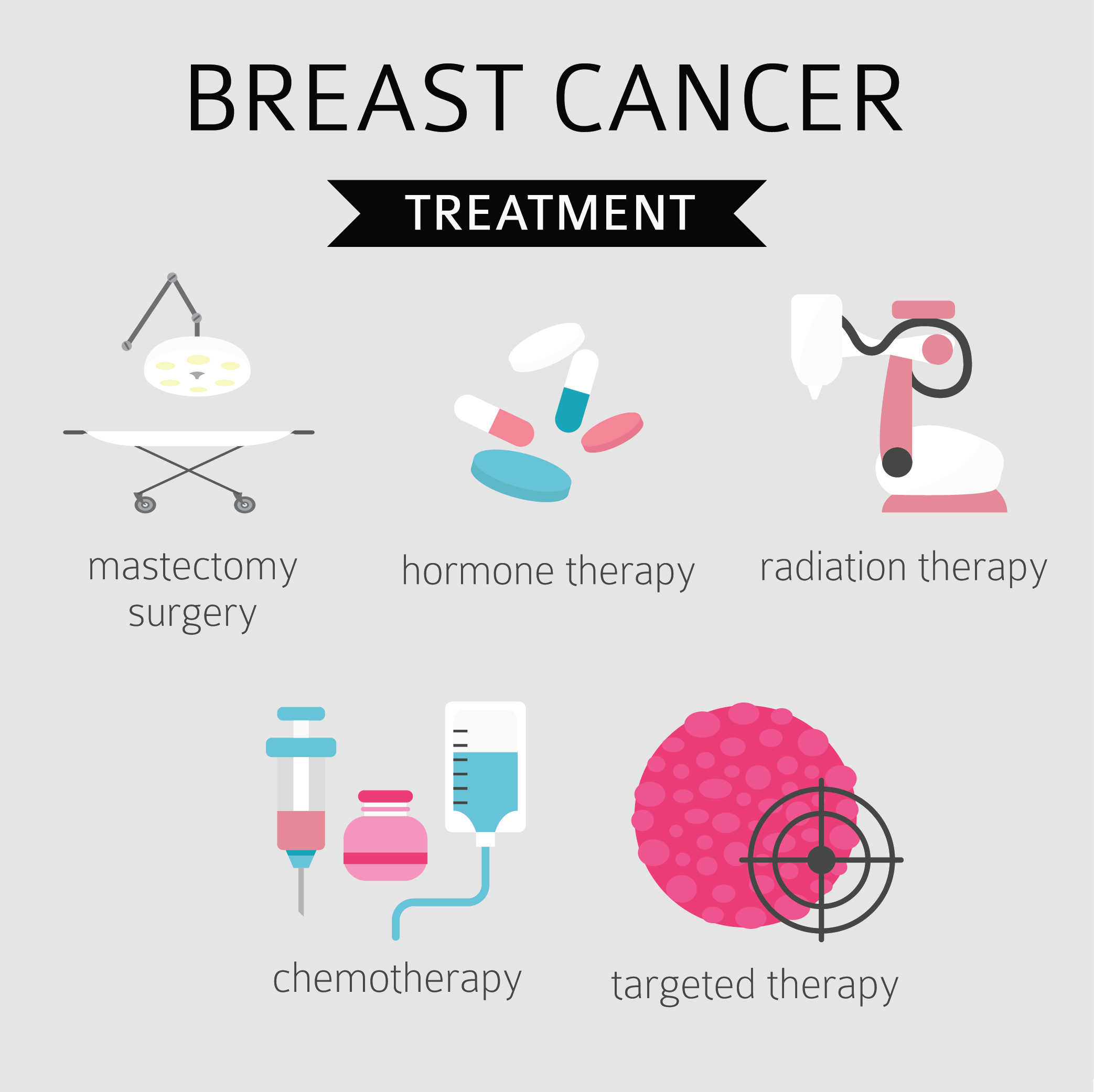
Advances In Conventional Breast Cancer Treatment
Early-stage, localized breast cancer is highly treatable, but not everyone is aware that cancer treatment in general has evolved and improved in the last few years. Advances in breast cancer treatment have improved patient outcomes while also reducing side effects patients may experience during treatment. Below are a few of the most promising developments.
Who Should Consider Pbi
The American Society of Therapeutic Radiology and Oncology provides the following recommendations:
You May Like: Does Breast Cancer Have Any Symptoms
Other Serms Such As Evista And Fareston
Raloxifene and toremifene are other SERMs that act similarly to tamoxifen. They stop cancer growth by binding to estrogen receptors and blocking the ability of estrogen to bind to these receptors. However, SERMs can also mimic the effects of estrogen in other parts of the body, such as the uterus, which can increase the risk of certain cancers. These drugs are not usually recommended if previous treatment with tamoxifen has not been successful. Toremifene is only approved for the treatment of metastatic breast cancer in postmenopausal women, so its uses are more limited than those of tamoxifen.
Some healthcare providers may prescribe raloxifene over tamoxifen due to its lower risk of serious side effects, such as uterine cancer. Raloxifene may be prescribed to postmenopausal women with osteoporosis who are at a high risk of invasive breast cancer. However, raloxifene may be less effective at preventing breast cancer than tamoxifen and has only been tested in postmenopausal women. On the other hand, tamoxifen is an option to prevent breast cancer in premenopausal women.
SERMs are generally taken by mouth. Side effects may include hot flashes, muscle or joint pain, and leg cramps. Serious side effects may include an increased risk of uterine or endometrial cancer and blood clots in the legs or lungs.
Can Other Drugs Interfere With Hormone Therapy
Certain drugs, including several commonly prescribed antidepressants , inhibit an enzyme called CYP2D6. This enzyme plays a critical role in the body’s use of tamoxifen because CYP2D6 metabolizes, or breaks down, tamoxifen into molecules, or metabolites, that are much more active than tamoxifen itself.
The possibility that SSRIs might, by inhibiting CYP2D6, slow the metabolism of tamoxifen and reduce its effectiveness is a concern given that as many as one-fourth of breast cancer patients experience clinical depression and may be treated with SSRIs. In addition, SSRIs are sometimes used to treat hot flashes caused by hormone therapy.
Many experts suggest that patients who are taking antidepressants along with tamoxifen should discuss treatment options with their doctors, such as switching from an SSRI that is a potent inhibitor of CYP2D6, such as paroxetine hydrochloride , to one that is a weaker inhibitor, such as sertraline or citalopram , or to an antidepressant that does not inhibit CYP2D6, such as venlafaxine . Or doctors may suggest that their postmenopausal patients take an aromatase inhibitor instead of tamoxifen.
Other medications that inhibit CYP2D6 include the following:
- quinidine, which is used to treat abnormal heart rhythms
Also Check: Does Alcohol Increase The Risk Of Breast Cancer
What Are The Alternatives To Traditional Radiation Therapy For Breast Cancer
Dana Casciotti, PhD, Anna E. Mazzucco, PhD, and Danielle Shapiro, MD, MPH, Cancer Prevention and Treatment Fund
Almost all women with early-stage breast cancer will live just as long if they choose lumpectomy instead of mastectomy. However, traditional radiation treatment is recommended for lumpectomy patients because it lowers their chances of the cancer returning.
Traditional radiation therapy is given on an outpatient basis 5 days each week for 6-8 weeks, and that is a difficult schedule for many patients. Many women living in rural areas or far from the hospital choose to get a mastectomy because daily radiation is so inconvenient.
For some women, radiation to a smaller area of the breast over a shorter period of time may be a useful alternative. These options are called partial breast irradiation .
PBI can be given with just 5-10 treatments over about a weeks time, and researchers are testing if treatments can be shortened to 2 days. According to experts, PBI can reduce the chances of a tumor coming back in the area around the lumpectomy from 10-25% to 3-4%.
Based on a comprehensive 2016 research review, women who had PBI were more likely to have their tumor come back or to have a new tumor form in the same breast than women who had whole breast radiation treatment . However, women who had PBI were not more likely to die any sooner or to later need a mastectomy.
Reducing Vaginal Dryness And Vaginal Atrophy
- Nonhormonal moisturizers.We recommend nonhormonal vaginal moisturizers like Replens and Hyalo GYN to hydrate, increase comfort with sexual activity, and help restore elasticity of the vaginal tissue, Dr. Goldfarb says. They can also be used in combination with lubricants for intercourse. Some women especially those who are taking aromatase inhibitors, which lower estrogen levels may need to use vaginal moisturizers more often than the three times per week recommended on the package in order to get the most benefit.
Along with Jeanne Carter, Director of MSKs Female Sexual Medicine and Womens Health Program, and medical oncologist Maura Dickler, Dr. Goldfarb is studying different ways of using these moisturizers and other intravaginal therapies to determine the optimal treatment and frequency of application in women with breast cancer. We are also investigating whether the product helps reduce insertional pain experienced by some patients at the beginning of intercourse, she says.
Recommended Reading: How Many Stages Are There To Breast Cancer
Combined Hrt And Breast Cancer
Combined estrogen and progesterone may have the highest risk factor of any type of HRT. According to BreastCancer.org, the risk of developing breast cancer increases by 75% for those taking combined HRT.
The organization also noted that combined HRT increases the chance that a healthcare professional may diagnose a persons breast cancer at a more advanced stage, which increases the likelihood of mortality.
According to the , the risk of breast cancer increases the longer a person takes HRT. However, it also decreases significantly after a person discontinues HRT.
The American Cancer Society states that the risk of breast cancer returns to average 3 years after a person discontinues combined HRT.
However, the researchers for the 2020 study found that risk reduced after 5 years for medroxyprogesterone, and 10 years for levonorgestrel, which are types of progesterone.
Combined HRT is also linked to breast density, which can make it harder to locate cancer on a mammogram. Breast density is a term to describe the amount of dense tissue compared to fatty tissue in a persons breast. Dense tissue is more fibrous than fatty tissue.
HRT containing estrogen alone can also increase the risk of a person developing breast cancer. However, it may only increase the risk after 10 years of continued use.
A person who has had or has breast cancer should not take HRT. Instead, they should speak with a doctor about alternative options.
Potential Benefits Of Risk
The USPSTF found convincing evidence that risk-reducing medications provide at least a moderate benefit in reducing risk for invasive estrogen receptorpositive breast cancer in postmenopausal women at increased risk for breast cancer .
Trials included women whose 5-year risk of breast cancer may have been lower than 3%.
Per 1000 women over 5 years of use.
§Results from the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene trial.
Both tamoxifen and raloxifene can reduce risk of some types of skeletal fractures, independent from the risk of breast cancer.
The USPSTF found that the benefits of taking tamoxifen, raloxifene, and aromatase inhibitors to reduce risk for breast cancer are no greater than small in women not at increased risk for the disease.
Also Check: Is Serovital Safe For Breast Cancer Survivors
Does Taking The Combined Pill Increase The Risk Of Breast Cancer
Taking the combined pill will slightly increase the risk of breast cancer compared to people who are not taking it. But its important to remember that there are other things that have a bigger effect on breast cancer risk. For example, being overweight or obese increases the risk of breast cancer much more than taking the pill does.
When you stop taking the pill, your breast cancer risk stops increasing. About 10 years after stopping, a persons risk is no longer affected.
Recommended Reading: What Are Some Symptoms For Breast Cancer
Hormones And Breast Cancer
The hormones estrogen and progesterone make some breast cancers grow. They are called hormone-sensitive breast cancers. Most breast cancers are sensitive to hormones.
Estrogen and progesterone are produced in the ovaries and other tissues such as fat and skin. After menopause, the ovaries stop producing these hormones. But the body continues to make a small amount.
Hormone therapy only works on hormone-sensitive cancers. To see if hormone therapy may work, doctors test a sample of the tumor that has been removed during surgery to see if the cancer might be sensitive to hormones.
Hormone therapy can work in two ways:
Read Also: What Is Considered Early Stage Breast Cancer
Where Does Evidence About The Health Effects Of Mht Come From
The most comprehensive evidence about the health effects of MHT comes from two randomized clinical trials that were sponsored by the National Institutes of Health as part of the Womens Health Initiative :
- The WHIEstrogen-plus-Progestin Study, in which women with a uterus were randomly assigned to receive either a hormone pill containing both estrogen and progestin or a placebo. The median duration of treatment was 5.6 years.
- The WHI Estrogen-Alone Study, in which women without a uterus were randomly assigned to receive either a hormone pill containing estrogen alone or a placebo. The median duration of treatment was 7.2 years.
More than 27,000 healthy women who were 50 to 79 years of age at the time of enrollment took part in the WHI hormone therapy trials. The goals of these trials were to see if MHT prevents heart disease and bone fractures in postmenopausal women and to determine if MHT affects risks of breast cancer and, for women with a uterus, endometrial cancer. Both trials were stopped early , when it was determined that both types of therapy were associated with specific health risks, but long-term follow up of the participants continues to provide new information about the health effects of MHT.
Can A Person With A Family History Of Breast Cancer Take Hrt
A 2019 article in the journal Archives of Breast Cancer states that there are no guidelines on the safety of HRT use in those with a family history of breast cancer.
A systematic review from 2021 notes that HRT does not have a relevant effect on the risk of cancer in those who carry the BRCA gene.
Another study from 2018 found that the use of estrogen after surgery to remove the ovaries does not increase the chance of breast cancer in those with the BRCA1 gene. However, they also note that further research is needed on the effect of progesterone-containing HRT.
Breast Cancer Now suggests that a person should speak with a doctor before using HRT if they have inherited a breast cancer gene, such as BRCA1 or BRCA2.
Recommended Reading: What Does Stage 4 Breast Cancer Mean
Hormones After Breast Cancer: Not Fuel For The Fire After All
Natural hormones reduce breast cancer tumors and have positive effects on cardiac and bone health
Parsemus Foundation
image: Mice on hormones exercised more than ones on the current treatment, estrogen blockers, leading to better overall health.view more
A new study supports a growing body of research suggesting a safe and effective role for natural steroid hormones in treating postmenopausal breast cancer, with fewer detrimental side effects and improved health profile than with standard anti-hormone therapies. The study will be published in final format today in the open-access journal Reproductive Biology and Endocrinology.
Breast cancer is the most frequently diagnosed cancer in women in the United States. Approximately 70% of breast cancers are diagnosed in postmenopausal women. Major clinical trials and experimental studies showed that a class of anti-estrogen drugs called aromatase inhibitors is effective against postmenopausal breast cancer. Yet despite their effectiveness in reducing tumor recurrence, aromatase inhibitors have adverse effects on the cardiovascular system and increase osteoporosis and bone fractures, which may explain their lack of overall survival improvement versus the older treatment, tamoxifen. These effects, together with undesirable side effects such as incontinence and bone and joint pain, cause many women to discontinue using AIs. Alternatives are needed.
HORMONES: NOT ALL THE SAME
COUNTERINTUITIVE RESULTS
Journal
Follow Up Care After Breast Cancer Treatment
Many women are relieved or excited to be finished with breast cancer treatment. But it can also be a time of worry, being concerned about the cancer coming back, or feeling lost without seeing their cancer care team as often.
For some women with advanced breast cancer, the cancer may never go away completely. These women may continue to get treatments such as chemotherapy, hormone therapy, or other treatments to help keep the breast cancer under control and to help relieve symptoms from it. Learning to live with breast cancer that doesnt go away can have its own type of uncertainty.
Even if you have completed breast cancer treatment, your doctors will want to watch you closely. Its very important to go to all of your follow-up appointments. During these visits, your doctors will ask if you are having any problems, and will probably examine you. Lab tests and imaging tests arent typically needed after treatment for most early stage breast cancers, but they might be done in some women to look for signs of cancer or treatment side effects.
You May Like: What Blood Test Can Detect Breast Cancer