Histopathological Evaluation Of Til Density
TIL density was evaluated pathologically using biopsy specimens. The pathological diagnosis and examination were jointly performed by two breast pathologists. The definition and evaluation method for TILs followed the International TILs Working Group 2014 . Specifically, the density of infiltrating lymphocytes was averaged on full sections, at least five fields, of the tumor stroma. The results were divided into four groups according to previous reports .
Fig. 1
Histopathologic evaluation of the tumor-infiltrating lymphocytes density was performed on hematoxylin and eosin-stained tumor section. The density of them was averaged on full sections, at least five fields, of the tumor stroma. The results were divided into four groups ,> 1050% ,10% , and absent , respectively)
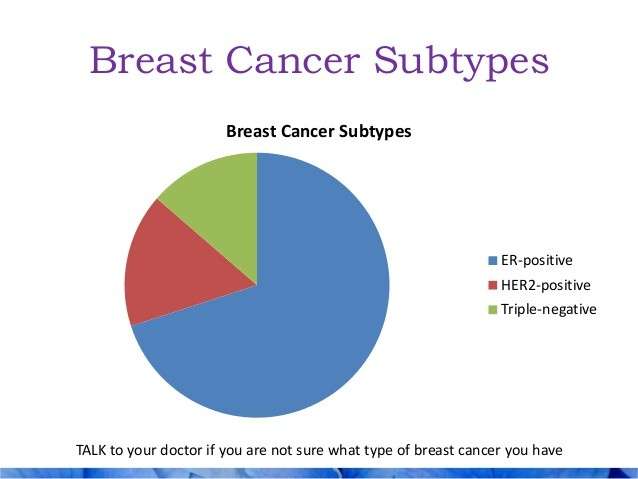
Breast Cancer Hormone Receptor Status
Breast cancer cells taken out during a biopsy or surgery will be tested to see if they have certain proteins that are estrogen or progesterone receptors. When the hormones estrogen and progesterone attach to these receptors, they stimulate the cancer to grow. Cancers are called hormone receptor-positive or hormone receptor-negative based on whether or not they have these receptors . Knowing the hormone receptor status is important in deciding treatment options. Ask your doctor about your hormone receptor status and what it means for you.
Vaccine Derived From Her2 Protein May Help Prevent Breast Cancer Recurrence
A new breast cancer vaccine that is derived from the HER2 protein may help prevent recurrence in patients with HER2-positive disease and appears safe. Phase II study results of the vaccine were released at the 2014 Breast Cancer Symposium, September 46, in San Francisco.
The HER2 protein, also known as human epidermal growth factor receptor 2, is found on the surface of certain cancer cells, including breast cancer. In normal cells HER2 helps control cell growth. Cancer cells, however, can make too much of the protein, which can cause cells to grow more quickly and be more likely to spread to other parts of the body.
The HER2-derived vaccine, known as GP2, is designed to provoke the bodys immune system to fight cancer by recognizing tumor cells that express HER2. It is administered in addition to standard breast cancer treatment, such as Hercpetin® , with the goal of preventing recurrence.
Based on these findings, the GP2 vaccine appears promising in addition to standard therapy in women with HER2-positive breast cancer, as it might have the potential to safely and effectively prevent recurrences. The researchers also speculate that GP2 works with Herceptin in a specific way to stimulate immune response and that further research into this interaction is warranted.
Copyright © 2016 CancerConnect. All Rights Reserved.
Also Check: What Does Breast Cancer Affect
Eat A Wide Variety Of Healthy Foods
According to a 2017 review of studies to date, people with breast cancer who eat a diet rich in vegetables, fruits, whole grains, fish, and poultry have better survival rates. There are many phytonutrients in the foods we eat, several of which have anti-cancer properties. That said, it’s likely that the combination of nutrients found in these foods that’s key, rather than any particular food.
To understand this, it helps to realize that cancer cells are “smart.” Unlike the popular conception of cancer, tumors are not unchanging clones of cells, but continually develop new mutations. Some of these mutations help a tumor grow. Some help a tumor avoid death . Others help a tumor spread, or suppress the body’s attempt to eliminate the cells . Just as tumor cells have many ways to continue their growth , a combination of healthy nutrients gives us the best opportunity to stay as healthy as possible.
Reducing Risk Of Recurrence
There are a number of myths regarding what may reduce the risk of breast cancer recurrence, as well as evidence-based information that is easily overlooked. We will look at measures that may reduce your risk based on credible studies, as well as practices that are unclear that you may wish to discuss with your oncologist.
In some cases, though the benefit on recurrence risk is still not clear, your quality of life may be improved. And living well with cancer is as important as extending your life with cancer.
Before talking about measures that may help lower recurrence risk, its important to not add to the stigma of the disease. Some people do absolutely everything right and their breast cancer recurs anyway. Similarly, some people eat poorly, smoke, and drink heavily and their cancer never recurs. While you may be able to decrease your risk of recurrence to a degree, dealing with breast cancer is dealing with a mutated clone of cells that doesnt think or follow the rules.
For those who have a recurrence, it doesnt mean they have done anything wrong. It simply means cancer is being cancer.
Recommended Reading: What Supplements Are Good For Hormonal Acne
Don’t Miss: Does Pain In Your Breast Mean Cancer
Her2 Positive Breast Cancer Survival Rate
The survival rate for HER2 positive breast cancer is a very broad, general indication of outcomes only. Those who are learning about the survival rate for HER2 positive breast cancer should remember that it does not predict what will happen for any particular patient. Rather, the survival rate is an average based on a large number of patients with HER2 positive breast cancer. Therefore, the survival rate should only be used as a point of reference.
Survival rates are discussed in terms of years. For example, the five-year survival rate for HER2 positive breast cancer shows the percentage of patients who survive five years or longer following their diagnosis. It is likely that the survival rate for HER2 positive breast cancer will continue to improve as new and better treatments are developed, and patients who are diagnosed today are projected to have better outcomes than those whom the current survival rates are currently based on.
You May Like: Is Breast Cancer Internal Cancer
Patients And Tumor Samples
The TransATAC project was initiated in 2002 to establish a tissue bank from formalin-fixed paraffin-embedded primary tumor blocks from post-menopausal ER+ breast cancer patients from the monotherapy arms of the ATAC trial.3,5 Archival tumor blocks were requested for patients except those known to be ER and PgR negative according to local tests, and those randomly assigned to the combination arm. RNA was extracted from FFPE blocks collected from the United Kingdom by Genomic Health Inc. for RS testing.24 Samples with sufficient residual RNA available for BCI analysis were used in this study. The conduct of this work was covered by an approval from the South-East London Research Ethics Committee and the Massachusetts General Hospital Institutional Review Board.
Recommended Reading: How Old Does Breast Cancer Start
Risk Of Recurrence: Early And Late
Research has shown the HER2-positive early breast cancers are two to five times more likely to recur than HER2-negative tumors. Even very small HER2-positive tumors with negative lymph nodes have a much higher risk of recurrence relative to tumors that are HER2-negative. Treatment with Herceptin can cut this risk by half.
The pattern of breast cancer recurrence may also differ. Small tumors are also more likely to have a metastatic recurrence if they are HER2-positive.
Despite the fact that HER2-positive and estrogen receptor-negative tuors are more likely to recur early on than estrogen receptor-positive and HER2-negative cancers, late recurrences are much less common.
With estrogen receptor positive breast cancers, the cancer is more likely to recur after five years than in the first five years, and the risk of recurrence remains steady each year for at least 20 years following the diagnosis. In contrast, those who have HER2 positive tumors and reach their five-year mark are much more likely to be in the clear and remain recurrence free.
Read Also: Are There Different Kinds Of Breast Cancer
What Are Hormones And Hormone Receptors
Hormones are substances that function as chemical messengers in the body. They affect the actions of cells and tissues at various locations in the body, often reaching their targets through the bloodstream.
The hormones estrogen and progesterone are produced by the ovaries in premenopausal women and by some other tissues, including fat and skin, in both premenopausal and postmenopausal women and in men. Estrogen promotes the development and maintenance of female sex characteristics and the growth of long bones. Progesterone plays a role in the menstrual cycle and pregnancy.
Estrogen and progesterone also promote the growth of some breast cancers, which are called hormone-sensitive breast cancers. Hormone-sensitive breast cancer cells contain proteins called hormone receptors that become activated when hormones bind to them. The activated receptors cause changes in the expression of specific genes, which can stimulate cell growth.
Breast cancers that lack ERs are called ER negative, and if they lack both ER and PR they may be called HR negative.
Approximately 67%80% of breast cancers in women are ER positive . Approximately 90% of breast cancers in men are ER positive and approximately 80% are PR positive .
Read Also: Do Cell Phones Cause Breast Cancer
Lisa Fought Breast Cancer For 8 Years Heres Her Story
In contrast to the common belief that surviving for five years after cancer treatment is equivalent to a cure, with hormone-sensitive breast tumors there is a steady rate of recurrence risk for at least 20 years after the original diagnosis, even with very small node-negative tumors.
Overall, the chance that an estrogen receptor-positive tumor will recur between five years and 20 years after diagnosis ranges from 10% to over 41%, and people with these tumors remain at risk for the remainder of their lives.
An awareness of the risk of late recurrence is important for a number of reasons. People are often shocked to learn that their breast cancer has come back after say, 15 years, and loved ones who don’t understand this risk are often less likely to be supportive as you cope with the fear of recurrence.
While chemotherapy has little effect on the risk of late recurrence hormonal therapy does, and estimating this risk may help determine who should receive extended hormonal therapy . Finally, late recurrences can differ from early relapse with regard to sites of metastases and survival.
Factors such as initial tumor size, number of nodes involved, and receptor status play into the risk of late recurrence, but tumor biology appears to have the greatest effect, and research is actively looking for ways to look at gene expression and copy number to predict risk.
Optimizing Adjuvant Therapy For Women With Estrogen Receptorpositive Node
Nodal status remains the single most important prognostic marker in outcomes for women with estrogen receptorpositive, HER2-negative breast cancer. For that reason, it makes sense to think about optimizing adjuvant therapy, including endocrine treatments, chemotherapy, and targeted therapy, Harold J. Burstein, MD, FASCO, PhD, told participants at the 2021 Lynn Sage Breast Cancer Symposium.1
Over the years, I have become progressively more persuaded that using adjuvant bisphosphonate therapy can help reduce the risk of cancer recurrence and improve long-term outcomes. Harold J. Burstein, MD, FASCO, PhDTweet this quote
Dr. Burstein is Professor of Medicine, Harvard Medical School, and medical oncologist at Dana-Farber Cancer Institute in Boston. The symposium was sponsored by Northwestern Medicine/Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago.
Two Fundamental Modalities
The two fundamental approaches to estrogen receptorpositive, early-stage breast cancer remain endocrine therapy and chemotherapy. Studies have looked at targeted treatment with cyclin-dependent kinases 4 and 6 inhibitors, but these agents have not yet been approved in the early-stage setting, and criteria for their use are undefined.
Reducing the Risk of Recurrence
Ovarian Suppression
Duration of Treatment
Optimizing Endocrine Therapy
Recapping, Dr. Burstein listed the following recommendations for optimizing endocrine treatment:
Bisphosphonates
Who Needs Chemotherapy?
You May Like: What Is Inflammatory Breast Cancer
Factors That Can Influence Survival Rate
There are a number of lifestyle factors that can influence outcomes for women with HER2 positive breast cancer. To give themselves the best chance at achieving a favorable outcome, it is recommended that patients:
- Maintain a healthy weight
- Eat a healthy and balanced diet
- Remain physically active, if possible
- Avoid tobacco use
Moffitt Cancer Center is a leader in cancer research and treatment. We provide our patients with individualized treatment plans and a full range of supportive care services to ensure all their needs are met as they undergo treatment. As a result, we are able to achieve the best possible outcomes and quality of life for our patients.
Those who have questions about the survival rate for HER2 positive breast cancer are encouraged to consult with a physician at Moffitt. To request an appointment with or without a referral, call or submit a new patient registration form online.
- BROWSE
You May Like: How Do I Tell If I Have Breast Cancer
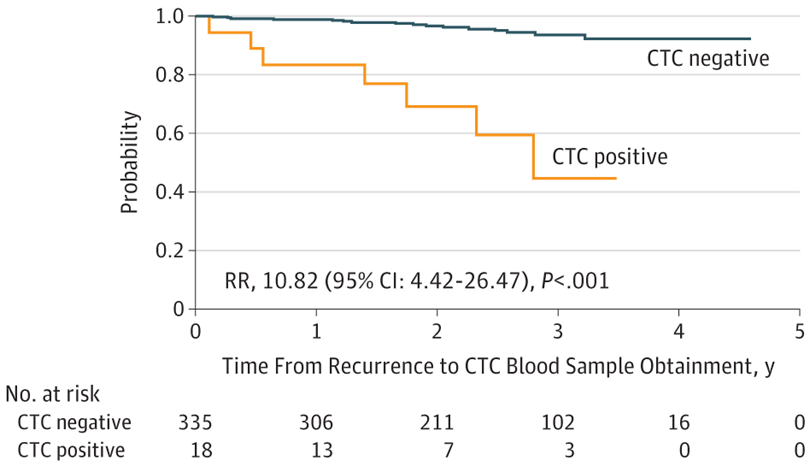
What Types Of Breast Cancer Have The Highest Recurrence Rates
A study published in the Journal of Clinical Oncology found the risk of recurrence for all breast cancers was highest in the first five years from the initial cancer diagnosis at 10.4%. This was highest between the first and second years after the initial diagnosis. During the first five years after the initial diagnosis, patients with oestrogen receptor positive breast cancer had lower rates of recurrence compared with those with ER negative disease. However, beyond five years, patients with ER positive disease had higher rates of recurrence.
You May Like: Do You Lose Weight When You Have Breast Cancer
Recurrences Can Occur Far Beyond The 5
Unlike the common perception that people who have survived for five years are “cured,” we know that some breast cancers, particularly hormone receptor positive breast cancers, can recur many years and even decades later. In fact, estrogen receptor positive early breast cancers are more likely to recur five years to 10 years after diagnosis than in the first five years.
A 2017 study in JAMA looked at over 62,000 cisgender women with estrogen receptor positive breast cancer over a period of 20 years. The women all received endocrine therapy for five years and were free of cancer when they stopped their medication. Over the next 15 years a steady number of these women developed distant recurrences of their cancer.
There are algorithms that can be used to estimate the risk of recurrence of a breast cancer, but none of these take into account all of the nuances of an individual person.
Recurrences sometimes occur locally in the breast, or regionally in nearby lymph nodes, but far too often are distant recurrences recurrences that show up in distant regions of the body such as the bones, lungs, liver, brain, or other areas. Once a distant recurrence occurs, breast cancer is no longer considered “curable” and the median survival rate of stage 4 breast cancer is only three years with treatment.
Estimating Risk Of Late Recurrence In Patients With Er+ Early
Association of tumor size, nodal status, and grade with risk of recurrence in years 5 to 10 and 10 to 20
| . |
|---|
However, these standard clinicopathologic features, although prognostic, are far from ideal predictors of who is at risk of late recurrence and do not provide sufficient guidance to make treatment decisions at the individual level because a substantial number of patients in each risk group will not experience a relapse within the 20-year follow-up period. In this regard, several diagnostic tests and scores derived from analyses of the primary tumor have been developed to identify patients at risk of early or late recurrence vs patients for whom deescalation of treatment is appropriate . These tests include the immunohistochemical 4 protein test, 21-gene Recurrence Score , PAM50 intrinsic subtype , 12-gene Recurrence Score , 2-component Breast Cancer Index , and 70-gene signature .
Univariate HRs and 95% CI indexes for all prognostic signatures in postmenopausal women according to nodal status during years 0 to 10
| Signature . |
|---|
You May Like: Can Breast Cancer Lead To Lung Cancer
Why Is This Study Important
The results of this study offer an immediate new treatment option for some people with HER2-negative metastatic breast cancers. Doctors look for the presence of the HER2 protein in breast cancer cells to guide treatment. In the past, people with breast cancer were considered HER2-positive
breast cancer. They are relevant to both hormone receptor-positive and hormone receptor-negative metastatic
Prognosis Of Late Vs Early Cancer Recurrence
Late recurrence is associated with a better prognosis than early recurrence in estrogen receptor-positive breast cancer. A 2018 study in Clinical Breast Cancer found that survival after recurrence was significantly longer in people with a late versus early recurrence . In this study, the lungs were the most common site of late distant recurrence.
Recommended Reading: Is There Immunotherapy For Breast Cancer
Binding And Functional Selectivity
The ER’s helix 12 domain plays a crucial role in determining interactions with coactivators and corepressors and, therefore, the respective agonist or antagonist effect of the ligand.
Different ligands may differ in their affinity for alpha and beta isoforms of the estrogen receptor:
- estradiol binds equally well to both receptors
- estrone, and raloxifene bind preferentially to the alpha receptor
- estriol, and genistein to the beta receptor
Subtype selective estrogen receptor modulators preferentially bind to either the – or the -subtype of the receptor. In addition, the different estrogen receptor combinations may respond differently to various ligands, which may translate into tissue selective agonistic and antagonistic effects. The ratio of – to – subtype concentration has been proposed to play a role in certain diseases.
The concept of selective estrogen receptor modulators is based on the ability to promote ER interactions with different proteins such as transcriptionalcoactivator or corepressors. Furthermore, the ratio of coactivator to corepressor protein varies in different tissues. As a consequence, the same ligand may be an agonist in some tissue while antagonistic in other tissues . Tamoxifen, for example, is an antagonist in breast and is, therefore, used as a breast cancer treatment but an ER agonist in bone and a partial agonist in the endometrium .