Annual Hazard Rate Of Lrr
Figure 4 shows the annual LRR patterns of the three groups in the entire cohort, HR+ cohort, and HR cohort. Visual inspection of the LRR hazard curves showed a difference in LRR patterns between the HER2 group and HER2+ + T group and HER2+ T group. In the entire cohort, the annual hazard rate of LRR in the HER2+ T group was consistently higher than that in the HER2 group or HER2+ + T group. The annual LRR curve of the HER2+ T group displayed an obvious double-peaked pattern, with an early peak at ~2.5 years and a late peak at ~9 years. The annual LRR curve of the HER2+ + T group displayed a single early peak at ~2.5 years. The annual LRR curve of the HER2 group displayed a continuously low risk without an obvious peak . The observed difference in LRR among these three groups occurred mainly during the first 5 years rather than beyond 5 years. The annual LRR rate of HER2, HER2+ + T, and HER2+ T groups was 1.4%, 1.3% and 3.0% during the first 5 years , and 0.5%, 0.4% and 1.9% after 5 years , respectively.
Figure 4 Annual hazard rates for locoregional recurrence of the entire group , HR-positive patients , and HR-negative patients grouped according to HER2 status and trastuzumab treatment. HR, hormonal receptor-negative HR+, hormonal receptor-positive HER2, HER2-negative HER2+ + T, HER2-positive with trastuzumab HER2+ T, HER2-positive without trastuzumab.
Relative Survival Rates For Breast Cancer
The National Cancer Institute gives 5-year relative survival rates for breast cancer based on how far the disease had spread before a doctor found it.
- Localized : 99%
- Regional : 86%
- Distant : 28%
- Unknown stage: 55%
- All stages: 90%
While these numbers can give you a general idea, they are an average for women with any type of breast cancer. They arent specific to the HER2+ type. They also come from data that researchers collected from 2010 to 2016, so they dont reflect more recent treatment advances.
What Is The Stage Of My Cancer
Cancer staging is a standardized way of classifying the severity of a patients cancer. There are various systems that use number or letter codes to designate the cancers status and how far it may have spread.
You may have heard of Stages 0 through IV, which reflect a tumors size and the extent of metastasis. A higher stage means a larger tumor and wider distribution of cancer cells.
Your doctor uses staging to plan your treatment, gauge your prognosis and communicate with other cancer specialists. What stage your cancer is in also will help determine whether youre eligible for clinical trials which offer newer treatment options.
Don’t Miss: What Is De Novo Metastatic Breast Cancer
According To A Ground
This means that 95% of all cancer cases are caused by environmental factors and lifestyle, i.e. epigenetics.
The M.D. Anderson study mentioned above determined that amongst the lifestyle factors that play a big part in cancer risk are:
-diet
-obesity, and
-cigarette smoking
What this means is that you can TURN OFF cancer-causing genes by improving your lifestyle with The 7 Essentials. Thiss concentrated attention and focus may also TURN ON cancer-protective ones.
Curcumin, Blueberries Found to Reduce HER2 Positive Breast Cancer Cells
Externally-influenced cellular expression can lead to disease but it can also be a factor for encouraging the body to heal. An example of this is how moving your body every day can boost energy, lower inflammation and lower your risk of Breast Cancer.
Regarding HER2 expression, results of a 2012 study published in the journal Evidence-based
Complementary and Alternative Medicine found that curcumin has potential as a treatment for HER-2-overexpressed breast cancer. Other studies have found that phytonutrients called peonidin-3-glucoside and cyaniding-3-glucoside, found in many fruits, vegetables and herbs, can encourage HER2 Positive Breast Cancer cell death in both in in vitro and in vivo studies.
YOU Control Your Genetic Destiny
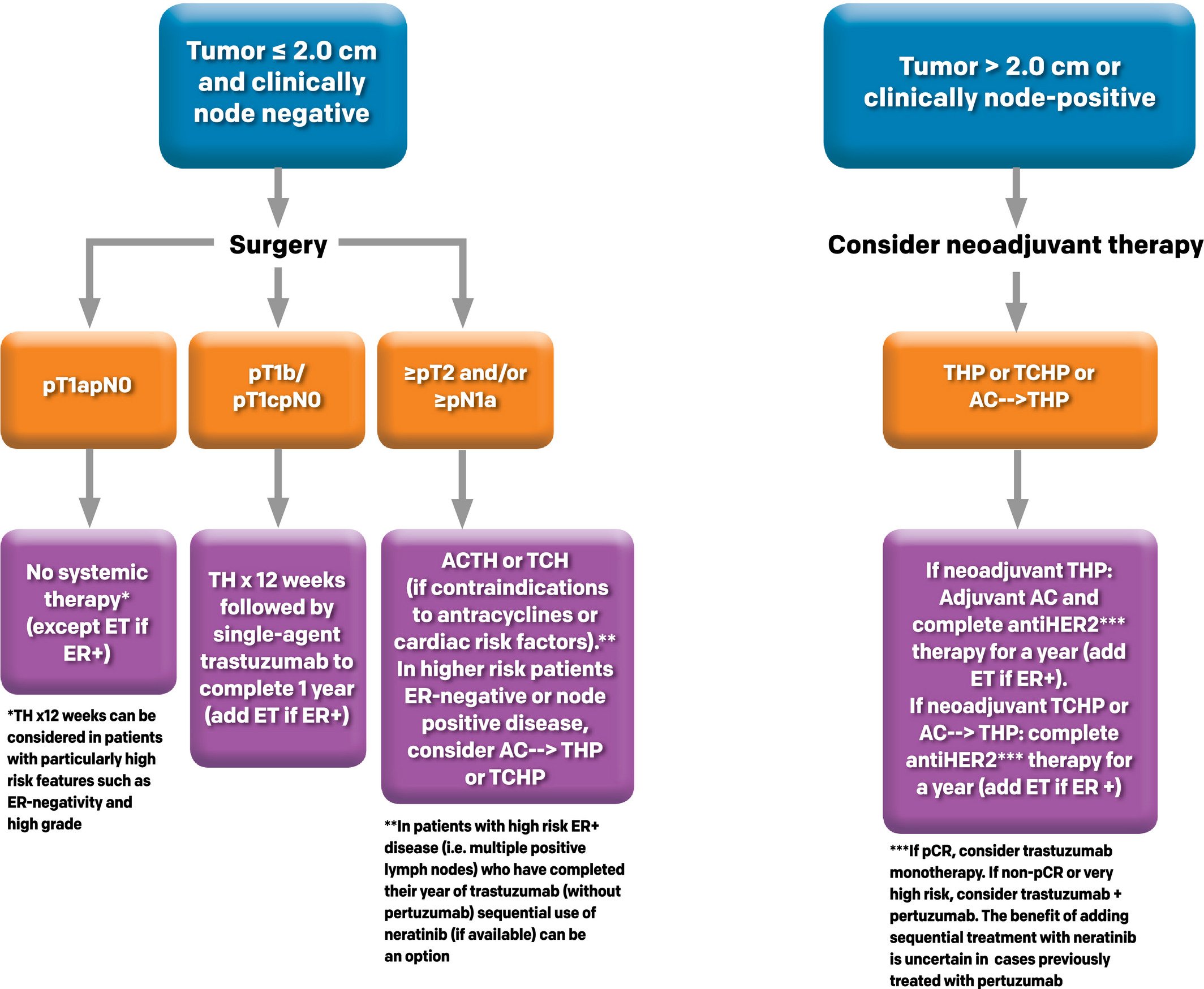
What Kind Of Therapy Is Used For Her2 Positive Breast Cancer
If the breast cancer cells overexpress HER2, it is called HER2-positive breast cancer. The following targeted therapy drugs have been specially designed to attach to the extra HER2 proteins to stop the growth of HER2-positive breast cancer cells. Trastuzumab is the most common targeted therapy drug used to treat HER2-positive breast cancer.
You May Like: What Are Some Signs And Symptoms Of Breast Cancer
Is The Cancer In My Lymph Nodes
Whether your breast cancer has spread to your lymph nodes the filtering mechanisms in your armpits and elsewhere in the body that are part of the immune system is one of the most important predictors of the severity of your disease.
Involvement of the lymph nodes changes the treatment plan, says Dr. Abraham. When breast cancer cells have spread to the lymph nodes, we tend to discuss more aggressive treatment options, such as chemotherapy.
Trastuzumab Provides A Comparable Prognosis In Patients With Her2
- Department of Radiation Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Background and Purpose: We investigated the locoregional effect of trastuzumab, and determined whether patients with human epidermal growth factor receptor 2-positive breast cancer treated with trastuzumab could achieve comparable efficacy to that of patients with HER2-negative BC.
Materials and Methods: This was post hoc analyses of data of 793 BC patients from a randomized controlled trial comparing post-mastectomy hypofractionated radiotherapy with conventional fractionated radiotherapy. Survival rates were analyzed by the KaplanMeier method and compared by the log-rank test.
Results: Patients were classified into three groups: HER2-negative , HER2-positve with trastuzumab , and HER2-positive without trastuzumab . The HER2+ + T group had significantly lower locoregional recurrence , distant metastasis and higher disease-free survival at 5 years than that of the HER2+ T group . The HER2 group had significantly lower LRR , DM and higher DFS at 5 years than that of the HER2+ T group . The difference in LRR, DM and DFS at 5 years was not significant between the HER2+ + T group and HER2 group . Different annual LRR patterns was found among groups according to HR status.
Recommended Reading: Does Breast Cancer Cause Hot Flashes
Histological Grade And Ki67
Histological grade information was available from the ICD-O-3 code and categorized as low , intermediate and high according to the Elston-Ellis modification of the Scarff-Bloom-Richardson grading system . Women with anaplastic carcinoma were excluded, leaving n=24,137 women for the analysis . Ki67 has been recorded routinely since 2011 and was categorized as low , intermediate or high according to cutoffs in the Norwegian treatment guidelines .
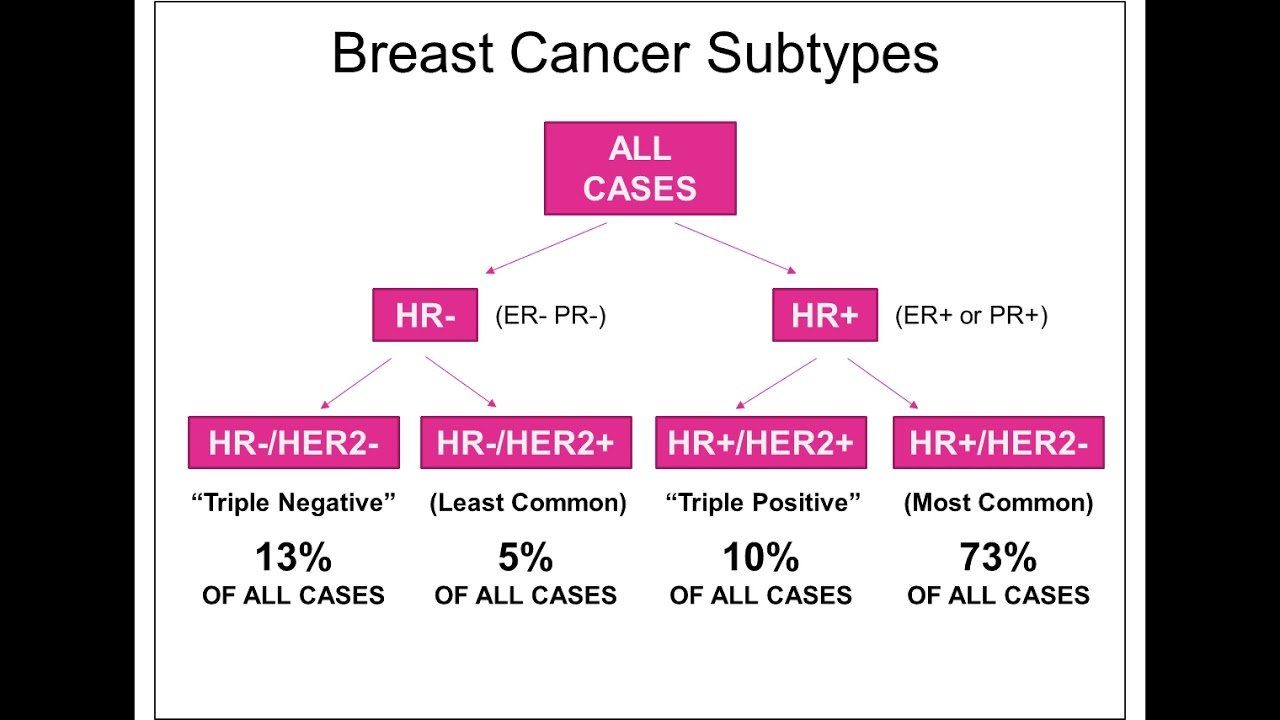
Why Receptor Status Matters
Breast cancer is not a single disease, and researchers now have the ability to break down breast cancer into different subtypes based on the receptor status of the tumors. Among the variations between different types of breast cancers are the proteins found on cell surfaces, which are involved tumor growth. These proteins are related to the genetic material of cancer cells.
For example, with estrogen receptor-positive breast cancer, estrogen binds to specific receptors on breast cancer cells, stimulating proliferation. Similarly, HER2 receptors on the surface of breast cancer cells are stimulated by HER2 protein, promoting the growth and spread of breast cancer.
It’s important to note, however, that all breast cellsboth cancerous and noncanceroushave HER2 receptors other their surfaces. The difference is that HER2-positive breast cancer cells have 40 to 100 times more receptors than HER2-negative breast cancer cells or normal breast cells. In positive cases, the abundance of receptors fuels the cancer.
Breast Cancer Discussion Guide
Get our printable guide for your next healthcare provider’s appointment to help you ask the right questions.
Recommended Reading: What Is The Survival Rate Of Breast Cancer Stage 4
How Is Her2 Cancer Diagnosed
Samples of breast tissue are removed during a biopsy or surgery and tested in the laboratory to look for presence of HER2 proteins. Commonly used tests to diagnose HER2 positivity include:
- Immunohistochemistry test: IHC test uses a chemical dye that stains HER2 protein and reveals its presence. The HER2 protein levels are scored from zero to three. Zero and one are considered HER2-negative, two is inconclusive and three is positive.
- Fluorescence in situ hybridization test: FISH test uses fluorescent pieces of DNA that attach to the HER2 gene and show if there are extra copies. FISH tests are usually performed if the IHC result is inconclusive, because they are more expensive and results take longer.
- Inform Dual ISH test: Inform Dual ISH test uses a stain that makes the HER2 protein change color.
The IHC tests are also used to find if the cancer cells have estrogen receptors and/or progesterone receptors . A positive result indicates that the cancer grows in response to these two female hormones.
Breast cancers are categorized into the following groups based on the HER2 and hormone receptor status:
- Luminal A: ER- and PR-positive, and HER2-negative breast cancer
- Luminal B: ER-positive, PR-negative and HER2-positive breast cancer
- HER2-positive: HR-negative and HER2-positive breast cancer
- Triple positive: ER-, PR- and HER2-positive breast cancer
- Triple negative : HR- and HER2-negative breast cancer
Original Articleher2 Positivity Is Not Associated With Adverse Prognosis In High
ER+/HER2+ early breast cancer patients treated with trastuzumab-based chemotherapy had superior prognosis.
-
ER+/HER2+ early breast cancer patients had distinct patterns of relapse or death from those of ER+/HER2-patients.
-
HER2 positivity itself may not be considered as an unfavorable factor for ER + patients in the era of trastuzumab.
Read Also: How To Determine Breast Cancer Risk
Researchers Develop Additional Her2
Despite these successes, many women with breast cancer dont benefit from current HER2-targeted treatments, or they become resistant to the effects of these drugs after initial treatment.
Therefore, researchers continue to test new or modified drug combinations. For example, in 2012, FDA approved pertuzumab as a treatment for women with HER2-positive metastatic breast cancer to be used in combination with trastuzumab and docetaxel , a chemotherapy drug. In 2017, pertuzumab received approval for use in combination with the same drugs as an adjuvant treatment for patients with HER2-positive early breast cancer at high risk of recurrence. Pertuzumab works by blocking HER2 from sending signals to other proteins that cause cells to grow and replicate.
Trastuzumab Has Radically Improved Prognosis For Her2+ Breast Cancer
HER2-positive breast cancer has gone from & quot worst to first& quot because of the success of the monoclonal antibody drug trastuzumab in combination with chemotherapy.& nbsp
Harold J. Burstein, MD, PhD
HER2-positive breast cancer has gone from “worst to first” because of the success of the monoclonal antibody drug trastuzumab in combination with chemotherapy, said breast oncologist Harold Burstein, MD, of the Dana-Farber Cancer Institute, speaking Saturday in Chicago at the 19th Annual Lynn Sage Breast Cancer Symposium, sponsored by Northwestern University’s Robert H. Lurie Comprehensive Cancer Center.
Disease-free survival rates have increased so dramatically since trastuzumab was introduced in 1998, and without significant toxicity from the drug, that, for a large proportion of patients, being diagnosed with this aggressive cancer is not the dire event it used to be.
About 1 in 5 of the 250,000 new breast cancers diagnosed every year is HER2 positive. About half are stage I and the remainder are stage II or III. Though HER2-positive cancers are more common in young women, they can occur at any age.
However, trastuzumab remains the starting point. A study of more than 4000 patients, published in 2014, showed that adding trastuzumab to chemotherapy led to a 37% relative improvement in overall survival, increasing 10-year survival from 75.2% to 84%. The 10-year disease-free survival rate increased from 62.2% to 73.7%. All patient subgroups benefited.2
References
Read Also: How Much Is Genetic Testing For Breast Cancer
Survival Rates For Breast Cancer
Survival rates can give you an idea of what percentage of people with the same type and stage of cancer are still alive a certain amount of time after they were diagnosed. They cant tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful.
Keep in mind that survival rates are estimates and are often based on previous outcomes of large numbers of people who had a specific cancer, but they cant predict what will happen in any particular persons case. These statistics can be confusing and may lead you to have more questions. Talk with your doctor about how these numbers may apply to you, as he or she is familiar with your situation.
What Is My Her2 Status
HER2 is another type of growth signal receptor which may be present on your breast cancer cells. About 25% of breast cancers are HER2-positive. HER2-positive cancers are a mix of good and bad news.
The bad news is the tumors tend to grow more aggressively than those without the HER2 receptor. The good news is that like ER/PR-positive cancers, medicines can switch the HER2 growth receptor off.
New drugs such as trastuzumab, pertuzumab, T-DM1 and lapatinib are extremely effective at this and have dramatically improved the prognosis for HER2-positive patients, Dr. Abraham says. Treatment outcomes are now as good as those with HER2-negative tumors.
But HER2-positive tumors bigger than half a centimeter or that have spread into the lymph nodes may require treatment with chemotherapy and one of the medicines specifically targeting the HER2 receptor, such as trastuzumab.
Recommended Reading: Where Would Breast Cancer Lumps Be
What Does Testing Involve
If a doctor confirms an unusual growth, they will take a biopsy. To collect a sample, they may perform one of the following procedures:
- Use a fine needle to remove a sample of breast cells or a liquid in fine-needle aspiration.
- Use a larger needle in a core needle biopsy.
- Carry out minor surgery as an outpatient procedure.
According to the American Cancer Society, a core needle biopsy is often the preferred option.
The doctor will send the tissue samples to a laboratory to test whether or not breast cancer is present. If it is, the pathologist will test to see if the cancer is HER2-positive.
The two main tests for determining whether or not HER2-positive cancer is present are the fluorescent in situ hybridization test and the immunohistochemistry test.
The FISH test looks for additional copies of the HER2 gene in breast cancer cells. It uses special labels that attach to the HER2 proteins that glow in the dark.
The IHC test uses a chemical dye to stain HER2 proteins and can determine how much HER2 protein is present in breast cancer cells.
Often, the pathologist will carry out the IHC test and then the FISH test. IHC testing is faster and less costly than FISH testing. However, if the results of the IHC test are unclear, a person will need a FISH test to determine whether or not a tumor is HER2-positive.
What Is A Hormone Receptor
In breast cancer, hormone receptors are the proteins located in and around breast cells. These receptors signal cells both healthy and cancerous to grow. In the case of breast cancer, the hormone receptors tell the cancer cells to grow uncontrollably, and a tumor results.
Hormone receptors can interact with estrogen or progesterone. Estrogen receptors are the most common. This is why ER-positive is the most common form of breast cancer.
Some people are diagnosed with progesterone receptor-positive breast cancer. The key difference is whether cancerous cells are getting growth signals from estrogen or progesterone.
Testing for hormone receptors is important in treating breast cancer. In some cases, there are no hormone receptors present, so hormone therapy isnt a good treatment option. This is called hormone receptor-negative breast cancer.
According to BreastCancer.org, about 2 out of 3 people with breast cancer have some form of hormone receptors present. This makes them candidates for hormone therapy.
Also Check: Does All Breast Cancer Chemo Cause Hair Loss
Tumour Size Nodal Status And Tnm Stage
Pathologic T and N status was coded according to AJCC 4th edition for 20052008 and AJCC 6th edition for 20082015 and categorized as pT1 , pT2 , pT3 , pT4, pN0 , pN1 , pN2 , pN3 and pN+ , and combined as pT1pN0, pT2pN0, pT1-2pN+ and pT3-4pN0/+ according to Norwegian treatment guidelines. Patients receiving neoadjuvant treatment were missing pTN status. Pathologic TNM stage was categorized into I, IIA, IIB, IIIA, IIIB or IV . This was combined with a SEER summary stage variable based on clinical data when pTNM missing into a TNM stage variable .
Will I Need Chemotherapy
Typically chemotherapy is a consideration for patients with high-risk breast cancers. Some factors that may indicate the need for chemotherapy are:
- Lymph node involvement.
- Tumors that are higher-grade, ER/PR-negative, HER2-negative or triple-negative .
- Tumors that are HER2-positive.
- Breast cancers in younger patients, especially those below the age of 40.
If you need chemotherapy, it will be given as an outpatient treatment every two to three weeks, delivered either directly into a vein or through a port.
Also Check: Does Breast Cancer Show Up In Blood Work
Her2s Genetic Link To Breast Cancer Spurs Development Of New Treatments
Single breast cancer cell and microenviornment visualized by transparent tumor tomography.
When NCI-supported researchers discovered that the HER2 gene is important for breast cancer growth, this led to the development of the drug trastuzumab and other targeted treatments that have improved survival for women with HER2-positive breast cancer.
What Are The Symptoms Of Her2 Breast Cancer

The most common symptom of most breast cancers, including HER2 breast cancer is a lump in the breast. A painless, hard mass with irregular edges is most likely cancer, but breast cancers can also have a lump that is soft and tender to the touch. Other possible symptoms in the first three stages of breast cancer include:
- Change in the size and shape of the breast
- Jaundice and stomach swelling
Also Check: How Many People Survive Breast Cancer