What Do Brca1 And Brca2 Genetic Test Results Mean
BRCA1 and BRCA2 mutation testing can give several possible results: a positive result, a negative result, or a variant of uncertain significance result.
Positive result. A positive test result indicates that a person has inherited a known harmful variant in BRCA1 or BRCA2 and has an increased risk of developing certain cancers. However, a positive test result cannot tell whether or when the tested individual will develop cancer. Some people who inherit a harmful BRCA1 or BRCA2 variant never develop cancer.
A positive test result may also have important implications for family members, including future generations.
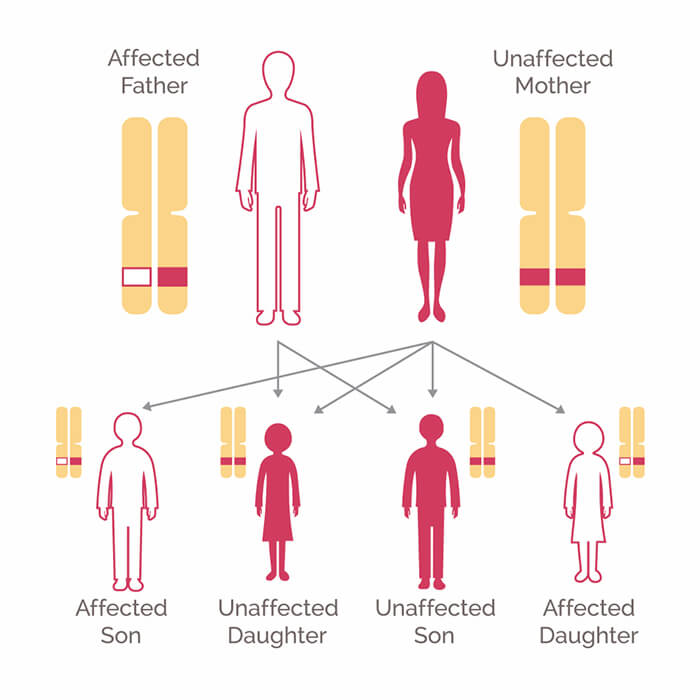
- Both men and women who inherit a harmful BRCA1 or BRCA2 variant, whether or not they develop cancer themselves, may pass the variant to their children. Each child has a 50% chance of inheriting a parents variant.
- All blood relatives of a person who has inherited a harmful BRCA1 or BRCA2 variant are at some increased risk of having the variant themselves. For example, each of that persons full siblings has a 50% chance of having inherited the variant as well.
- Very rarely, an individual may test positive for a harmful variant not inherited from either parent. This is called a de novo variant. Such a variant is one that arose in a germ cell of one of the parents and is present in all the cells of the person who grew from that cell. The children of someone with a de novo variant are at risk of inheriting the variant.
How To Get Brca Genetic Testing
Genetic counseling is recommended for those who are interested in being tested for breast cancer gene mutations.;You can talk to a doctor about getting a referral to a genetic counselor, who can help determine whether genetic testing would make sense based on family history and risk factors.;Since many genetic tests only look for one specific gene mutation, the counselor can often help determine which mutations to test for.
The genetic test itself simply involves taking a small sample of blood or saliva, which is sent to a lab for analysis. Results can take several weeks or months.
Genetic testing results are not always clear-cut:
- A test result can be positive, meaning that the patient does carry the gene mutation.
- A negative test result indicates that they do not have that particular known gene mutation. It does not, however, rule out the possibility of having mutations in other genes. It also does not rule out the possibility of developing breast cancer. Most breast cancer cases are not hereditary, so everyone should still have an;early detection plan.
- Genetic test results can also be uncertain or ambiguous. An ambiguous test result means that a mutation has been found on the gene, but it is not yet known whether that particular mutation has any effect on the chances of developing breast cancer.
- Someone is either negative or positive. Over time, a person cannot go from being negative to being positive or vice versa for the specific gene mutations they were tested for.
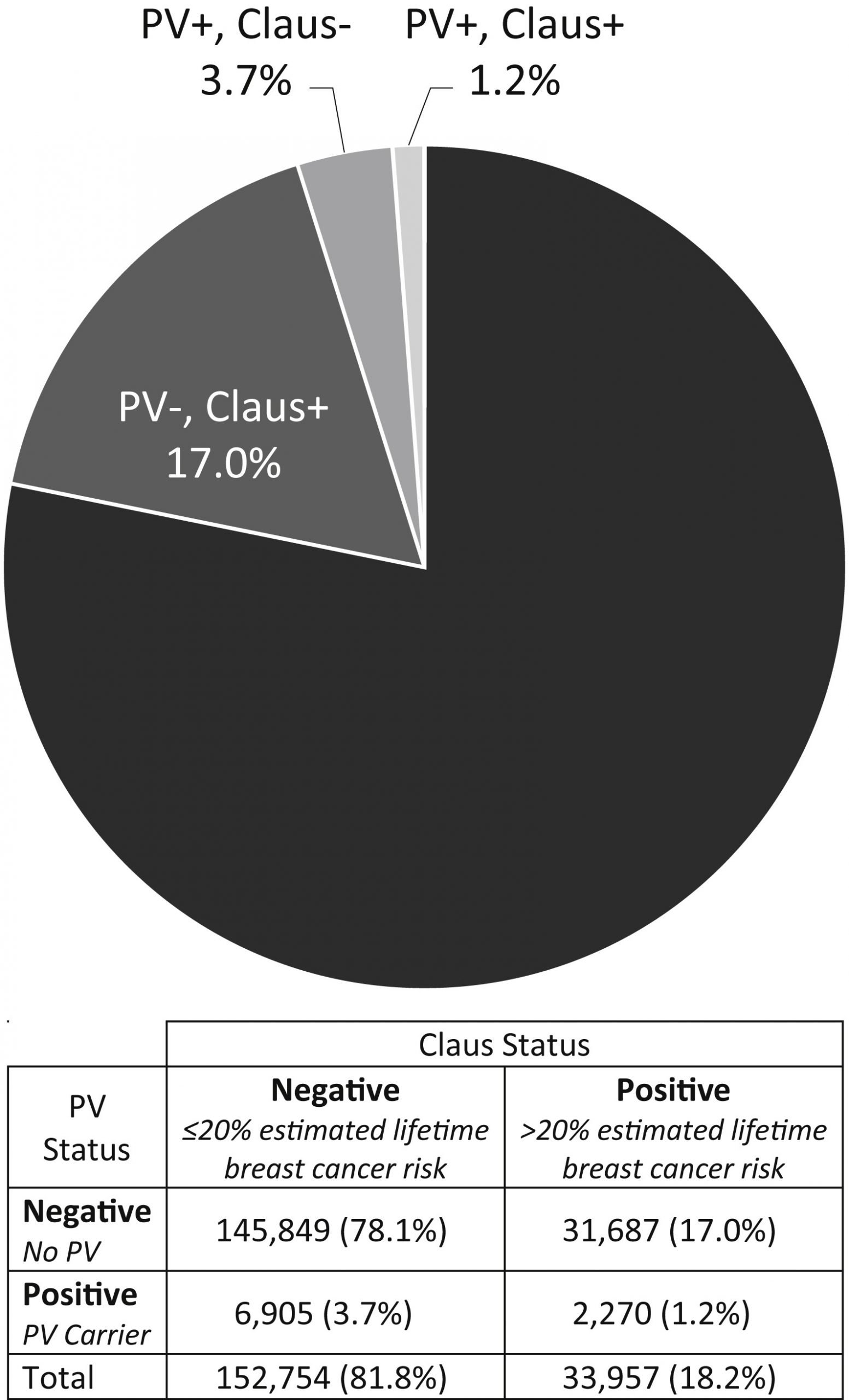
Should All Patients With Breast Cancer Be Offered Expanded Panel Testing
The lowered costs of genomic testing with coverage not infrequently available through health insurance may help facilitate expansion of rather restrictive guideline-based criteria. Removing barriers to testing may increase provider discussions and referrals, reducing the barriers associated with testing. Expanding guidelines may improve support for better management of at-risk populations and their reach to cancer genetic services. Ambiguity of results on moderate penetrance genes and VUS may be alleviated by expanded use of multigene panel testing in diverse populations. Wholesale adoption of universal multigene panel testing in all women diagnosed with breast cancer may help identify many more patients harboring pathogenic variants, which is important for the patients and their families.
Recommended Reading: How To Remove Breast Cancer Naturally
How Much Does Brca1 And Brca2 Mutation Testing Cost
The cost for BRCA1 and BRCA2 mutation testing usually ranges from several hundred to several thousand dollars. Insurance policies vary as to whether the cost of testing is covered. People who are considering BRCA1 and BRCA2 mutation testing may want to find out about their insurance company’s policies regarding genetic tests.
Weighing The Risks And Benefits Of Genetic Testing
A health care provider or genetic counselor can talk with you about the risks, benefits and issues you may face when youre considering genetic testing.
Testing for BRCA1, BRCA2 and other inherited gene mutations only requires a blood or saliva sample. However, there can be physical, emotional and financial impacts of knowing whether or not you have an inherited gene mutation. Thats why its important to carefully consider whether you want to be tested.;
Genetic testing is especially helpful for people who fall into one of the categories listed above.
Even if its recommended, genetic testing is a personal decision. A genetic counselor can help you decide if genetic;testing is right for you . If you decide to get tested, your genetic counselor can help you choose the test that meets your needs.
Recommended Reading: How Quickly Does Triple Negative Breast Cancer Grow
Talk With Your Health Care Provider Or A Genetic Counselor
The process of genetic testing is complex. Its best to meet with a genetic counselor or a trained health care provider to make decisions about testing. They can help you choose a test that meets your needs.
Your health care provider or a genetic counselor can help you correctly interpret the test results. If the testing was not done in a certified lab, your health care provider can help you get a clinical genetic test to confirm the results.
If clinical genetic testing finds a gene mutation related to breast cancer, your health care provider or a genetic counselor can help you make informed decisions about breast cancer screening and any risk-lowering options that may be right for you.
Learn about genetic test results.
How Is Genetic Testing Done
Genetic tests are usually requested by a persons genetic counselor, doctor, or other health care provider who has reviewed the individuals person and family history. The genetic test options from which a health professional may select include those that look at a single gene and those that look for harmful variants in multiple genes at the same time. Tests of the latter type are called multigene tests.
Testing is done on a small sample of bodily fluid or tissueusually blood, but sometimes saliva, cells from inside the cheek, or skin cells. The sample is then sent to a laboratory that specializes in genetic testing. The laboratory returns the test results to the doctor or genetic counselor who requested the test. It usually takes several weeks or longer to get the test results.
Health insurance typically covers genetic counseling and many genetic tests, if they are considered medically necessary. A person considering genetic testing should discuss costs and health insurance coverage with their doctor and insurance company before being tested.
You May Like: Can Breast Cancer Develop In One Year
Who Qualifies For Genetic Testing For Breast Cancer
Organizations such as the National Comprehensive Cancer Network and the U.S. Preventive Services Task Force outline criteria for who should be considered for genetic testing for breast cancer.
Guidelines focus on those who have a higher likelihood of carrying one of the harmful gene mutations associated with breast cancer. Examples include:
- Being diagnosed with breast cancer before the age of 45 or being diagnosed with triple-negative breast cancer;before age 60
- Having a close family member diagnosed with breast cancer at age 50 or younger
- Having a close family member diagnosed with a cancer linked to an inherited risk for breast cancer, such as ovarian cancer or pancreatic cancer
- Having two close family members diagnosed with breast cancer, one of whom was diagnosed at age 50 or younger
- Having three or more relatives on the same side of the family diagnosed with breast cancer at any age
- Having a family history of breast, ovarian or pancreatic cancer and being of Ashkenazi Jewish descent
What To Know About Genetic Testing For Breast Cancer
Genetic testing for breast cancer is easier to get than it ever has been. How do you know if it’s right for you? PEOPLE asked top cancer docs to find out
Ask a Doctor is PEOPLEs series getting you the answers to the medical, health and personal questions that you always wanted to know but werent sure who to ask.
As Breast Cancer Awareness month kicks off in October, its an important time to revisit the screening methods available to help detect the disease early which can be critical in successfully fighting it, as early detection is linked to higher survival rates at five and 10 years out from first diagnosis. In addition to studying the warning signs of breast cancer so you can recognize any changes in your own breasts, mammograms are probably the most common and well-known method of detection; however, sonograms and even MRIs can be used to find tumors.
Doctors also may recommend that higher-risk individuals get genetically tested for breast cancer, as there are a few genetic mutations that, if present, indicate a higher chance of developing breast cancer later on.
Genetic testing has become much more advanced and more widely available, and the costs have plummeted over time, explains Lisa Newman, MD, chief of breast surgery at Weill Cornell Medicine and NewYork-Presbyterian Hospital. Its really wonderful to have access to that information.
So how do you know if you should get tested? PEOPLE spoke with top cancer doctors to find out what you need to know.
Also Check: Can Roundup Cause Breast Cancer
What Do The Results Of Genetic Testing Mean
Genetic testing can give several possible results: positive, negative, true negative, uninformative negative, variant of uncertain significance, or benign variant.
Positive result. A positive test result means that the laboratory found a genetic variant that is associated with an inherited cancer susceptibility syndrome. A positive result may:
- For a person who has cancer, confirm that the cancer was likely due to an inherited genetic variant and help guide treatment choices
- Indicate an increased risk of developing certain cancer in the future and guide future management to lower that risk
- Provide important information that can help other family members make decisions about their own health care, such as whether to have genetic testing to see if they have also inherited the variant.
;Also, people who have a positive test result that indicates that they have an increased risk of developing cancer in the future may be able to take steps to lower their risk of developing cancer or to find cancer earlier, including:
- Being checked at a younger age or more often for signs of cancer
- Reducing their cancer risk by taking medications or having surgery to remove at-risk tissue.
- Changing personal behaviors to reduce the risk of certain cancers
- Getting help to guide decisions about fertility and pregnancy
How Do I Decide Whether To Have A Genetic Test
Before you have a test, the genetic counsellor will talk to you about what your options are if you do have a faulty gene. This is usually part of the process of deciding whether to have the test or not. The options will depend on:
- the particular gene fault that you may have
- which cancers you are at increased risk of developing
- your age and plans for the future
If a faulty gene is found, you may have:
- regular screening to pick up cancers early
- treatment to reduce the risk of cancer, such as medicines or surgery
Read about possible screening and treatment options on the page about getting your genetic test results.
Making a decision about whether to have genetic testing can be difficult. It is normal to feel anxious. Thinking about the possibility of getting cancer is difficult. It may also bring back emotions you felt when other family members were diagnosed with cancer and what they went through.
It is important to take time to think it through. Before you decide, it can help to think about these questions:
- how do you feel about having a test?
- what will the result really mean for you and your family?
- what will you do if the result is positive?
- how will you feel if the result is positive?
- will you feel reassured by a negative test?
- would you rather not know if you have an increased risk of cancer?
- is there treatment to reduce your risk?
- if there is treatment, would you consider having it?
- what will happen if you decide not to have the test could you have regular screening?
Don’t Miss: When Do You Need Radiation For Breast Cancer
Does Insurance Pay For Genetic Testing For Breast Cancer
Insurance pays;for genetic testing for breast;cancer as long as the person meets the criteria. This includes having a family;history of breast;cancer or a family history of cancer, such as pancreatic cancer or ovarian cancer. While oncology costs are much more expensive than gene testing by most laboratories in the United States, insurance companies are often charged a lot of money for the test, which is why they are strict with insurance;coverage.;
Higher risk individuals such as those of Ashkenazi Jewish descent, history or breast cancer, or history of ovarian cancer often receive coverage for breast;cancer;genetic testing. These risk factors increase their susceptibility to a cancer;diagnosis.
Health insurance doesnt always cover 100% of the cost of a DNA test. A co-pay may be required, which is usually a percentage of the total cost. Every health insurance provider has its own costs for breast;cancer;genetic testing and policies differ;greatly.;
Fighting To Bring Down Costs
Health insurers aren’t required to cover cancer screenings, beyond what is mandated by the ACA, which is focused on the “average risk” population. That leads many to struggle to get coverage for earlier, more intensive screenings and risk-reducing surgeries, according to FORCE.
While insurance typically covers the surveillance, those who have high-deductible plans may still wind up with a hefty bill, said FORCE’s Schlager.
“We are testing people but not empowering them with easy access, necessarily, to the follow-up care,” she said.
Medicare doesn’t cover preventive care, unless authorized by Congress. Right now, those over 50 years old can get screening colonoscopies covered and those over 40 can get screening mammograms â as well as a baseline between the ages of 35-39. However, anyone younger on Medicare, such as those with disabilities, won’t be covered.
Medicare also doesn’t cover breast MRIs, which doctors recommend for those with a high breast cancer risk, as well as preventive surgeries, Schlager said.
Our whole health system is focused on treatment. If we were to flip that and focus on prevention, we would probably save the system a lot of money long-term.Lisa Schlagervice president of public policy at FORCE
She’s currently working on legislation with Sen. Lisa Murkowski, R-Alaska, and Rep. Debbie Wasserman Schultz, D-Florida, to amend the Medicare statute to broaden the preventive cancer screenings.
Also Check: How To Find Out You Have Breast Cancer
Genetic Mutations Linked To A Higher Risk Of Breast Cancer
Scientists studying cancer genetics continue to find and evaluate inherited mutations that may increase a familys cancer susceptibility.
The inherited genes most commonly tested because of their association with an increased risk of breast cancer include:
BRCA1: Between 55 percent to 72 percent of women who inherit the BRCA1 genetic mutation will develop breast cancer during their lifetime, according to the NCI. These same women have a 39 percent to 44 percent chance of developing ovarian cancer, compared to approximately 1.2 percent of women in the general population.
BRCA2: Between 45 percent to 69 percent of women who inherit the BRCA2 genetic mutation will develop breast cancer in their lifetime. Their risk of developing ovarian cancer ranges from 11 percent to 17 percent.
Women with BRCA1 and/or BRCA2 mutations are also at increased risk for pancreatic cancer.
Men who inherit one of these BRCA genetic mutations are at higher risk of developing male breast cancer, as well as pancreatic cancer;and prostate cancer.
CHEK2: About 1 percent of people carry this mutation. Its more common than the BRCA mutations, but the risk of developing a cancer associated with it is lower. A woman with a mutation in the CHEK2 gene has a 23 to 48 percent lifetime risk of developing a first breast cancer and a 29 percent chance of developing a second breast cancer within 10 years of the first.
Having this mutation is also associated with a higher risk of colon cancer.
How Can A Person Who Has Inherited A Harmful Brca1 Or Brca2 Gene Variant Reduce Their Risk Of Cancer
Several options are available for reducing cancer risk in individuals who have inherited a harmful BRCA1 or BRCA2 variant. These include enhanced screening, risk-reducing;surgery;, and chemoprevention.
Enhanced screening. Some women who test positive for harmful BRCA1 and BRCA2 variants may choose to start breast cancer screening at younger ages, have more frequent screening than is recommended for women with an average risk of breast cancer, or have screening with magnetic resonance imaging in addition to mammography.;
No effective ovarian cancer screening methods are known. Some groups recommend transvaginal ultrasound, blood tests for the CA-125 antigen , and clinical examinations for ovarian cancer screening in women with harmful BRCA1 or BRCA2 variants. However, none of these methods appear to detect ovarian tumors at an early enough stage to improve long-term survival .;
The benefits of screening men who carry harmful variants in BRCA1 or BRCA2 for breast and other cancers are not known. Some expert groups recommend that such men undergo regular annual clinical breast exams starting at age 35 . The National Comprehensive Cancer Network guidelines recommend that men with harmful germline variants in BRCA1 or BRCA2 consider having a discussion with their doctor about prostate-specific antigen testing for prostate cancer screening starting at age 40 .
You May Like: Is It Possible To Have Breast Cancer At 16