Brca Mutations And Other Cancers
Ovarian cancer occurs in roughly 1.3% of women in the general population. For those with BRCA1 mutations, 39% are expected to develop ovarian cancer, while 11% to 17% of those with a BRCA2 mutation will develop the disease.
There are other cancers that can be associated with BRCA mutations as well, such as prostate cancer, pancreatic cancer, and lung cancer.
What Are The Genes That Protect You From Cancer
The breast cancer 1 and breast cancer 2 genes are the genes most commonly affected in hereditary breast and ovarian cancer. Normally, the BRCA1 and BRCA2 genes protect you from getting certain cancers. But certain mutations in the BRCA1 and BRCA2 genes prevent them from working properly, so that if you inherit one
Is Her2 A Cancer
HER2 breast cancers are likely to benefit from chemotherapy and treatment targeted to HER2. Group 4 . This type, which is also called triple-negative breast cancer, includes tumors that are ER negative, PR negative and HER2 negative. Basal-like breast cancers are likely to benefit from chemotherapy.
Read Also: When’s Breast Cancer Month
Targeted Therapies For Brca
There is no single management strategy in reducing the risk of breast and ovarian cancer for BRCA mutation carriers and these issues have been reviewed recently in details by Bougie and Weberpals . The decision-making processes such as surveillance, risk-reducing surgery, and/or chemoprevention are very complex and differ from patient to patient due to their age, family history of female breast, male breast, ovarian, prostate, and pancreatic cancer in the risk stratification model. Thus clinical managements of patients with BRCA mutation carriers are highly challenging. In fact, there are no standard guidelines for recommending BRCA1 or BRCA2 mutation testing. Although surveillance strategies like mammography and breast magnetic imaging is helpful for breast cancer but there is no effective screening strategy has been developed for ovarian cancer . Treatment options often depend on risk-reducing surgical procedures such as bilateral mastectomy and salpingo-oophorectomy . Chemopreventive strategies have been considered to reduce the risk of breast cancer only for high-risk women and involve the use of selective estrogen receptor modulators such as Tamoxifen, Raloxifene and aromatase inhibitors, whereas oral contraceptives have been used for chemoprevention of hereditary ovarian cancer .
Microrna Repression Of Brca1 In Breast Cancers
There are a number of specific microRNAs, when overexpressed, that directly reduce expression of specific DNA repair proteins In the case of breast cancer, microRNA-182 specifically targets BRCA1. Breast cancers can be classified based on receptor status or histology, with triple-negative breast cancer , HER2+ , ER+/PR+ , and Invasive lobular carcinoma . All four types of breast cancer were found to have an average of about 100-fold increase in miR-182, compared to normal breast tissue. In breast cancer cell lines, there is an inverse correlation of BRCA1 protein levels with miR-182 expression. Thus it appears that much of the reduction or absence of BRCA1 in high grade ductal breast cancers may be due to over-expressed miR-182.
In addition to miR-182, a pair of almost identical microRNAs, miR-146a and miR-146b-5p, also repress BRCA1 expression. These two microRNAs are over-expressed in triple-negative tumors and their over-expression results in BRCA1 inactivation. Thus, miR-146a and/or miR-146b-5p may also contribute to reduced expression of BRCA1 in these triple-negative breast cancers.
Don’t Miss: How To Test For Inflammatory Breast Cancer
Genetic Testing For Brca Mutations
Overall, genetic testing for breast cancer genes is not standard. However, it is often recommended for women who have a family history of breast cancer or who have personally had breast cancer at a young age.
While you might have medical indications for getting tested, this is an emotionally charged decision. You may be faced with major decisions if you test positive for BRCA genes or other breast cancer genes .
Many women want to get tested in every way possible, while others prefer to avoid knowing about their risks.
Considerations as you make a decision about getting tested:
- If you are thinking about getting tested for breast cancer genes, you should speak with your healthcare provider and/or a genetic counselor before your test.
- If you’re struggling with the decision to move ahead with BRCA testing, you may benefit from having a conversation with your loved ones about how you might handle your results.
- Your health insurance carrier might cover the cost of genetic testing, but they might have criteria for coverage based on risk. If you are not considered high risk, you still can get tested and pay for it out of pocket, if you desire.
Regardless of your decision about genetic testing, you need to get your recommended mammograms.
Keep in mind that a negative test result does not mean that you will not get breast cancer. Likewise, testing positive doesn’t mean you will absolutely get breast cancer.
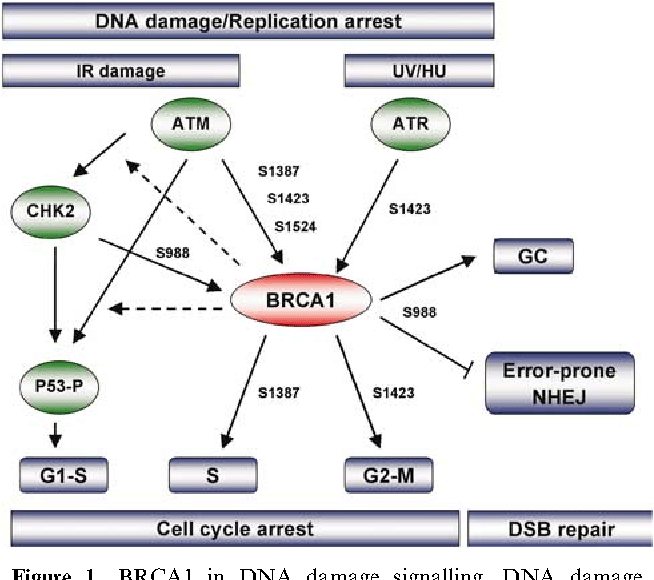
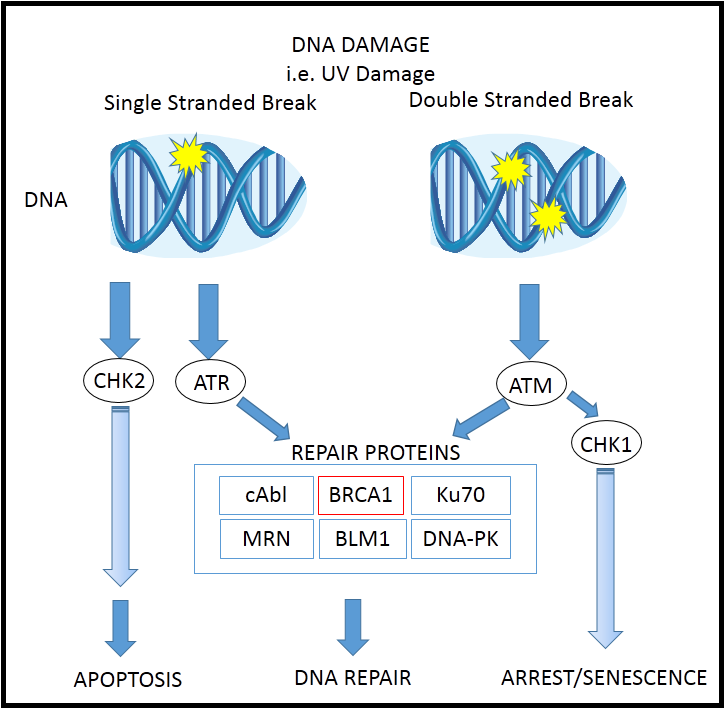
Deficiency Of Brca1 Expression Is Likely Tumorigenic
DNA damage appears to be the primary underlying cause of cancer, and deficiencies in DNA repair appears to underlie many forms of cancer. If DNA repair is deficient, DNA damage tends to accumulate. Such excess DNA damage may increase mutational errors during DNA replication due to error-prone translesion synthesis. Excess DNA damage may also increase epigenetic alterations due to errors during DNA repair. Such mutations and epigenetic alterations may give rise to cancer. The frequent microRNA-induced deficiency of BRCA1 in breast and ovarian cancers likely contribute to the progression of those cancers.
Also Check: How To Treat Stage 4 Breast Cancer
The Brca1 And Brca2 Genes
The genes most commonly affected in hereditary breast and ovarian cancer are the breast cancer 1 and breast cancer 2 genes. About 3% of breast cancers and 10% of ovarian cancers result from inherited mutations in the BRCA1 and BRCA2 genes.
Normally, the BRCA1 and BRCA2 genes protect you from getting certain cancers. But some mutations in the BRCA1 and BRCA2 genes prevent them from working properly, so that if you inherit one of these mutations, you are more likely to get breast, ovarian, and other cancers. However, not everyone who inherits a BRCA1 or BRCA2 mutation will get breast or ovarian cancer.
Everyone has two copies of the BRCA1 and BRCA2 genes, one copy inherited from their mother and one from their father. Even if a person inherits a BRCA1 or BRCA2 mutation from one parent, they still have the normal copy of the BRCA1 or BRCA2 gene from the other parent. Cancer occurs when a second mutation happens that affects the normal copy of the gene, so that the person no longer has a BRCA1 or BRCA2 gene that works properly. Unlike the inherited BRCA1 or BRCA2 mutation, the second mutation would not be present throughout the persons body, but would only be present in the cancer tissue.
If you are concerned that you could have a BRCA1, BRCA2, or other mutation related to breast and ovarian cancer, the first step is to collect your family health history of breast and ovarian cancer and share this information with your doctor.
Conflict Of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
SM and MR are employees of Invictus Oncology Pvt. Ltd. and hold equity of IOPL. All remaining authors have no potential conflicts to disclose.
Recommended Reading: What To Do If You Think You Have Breast Cancer
Family Screening For Brca1 And Brca2 Mutations
Genomic DNA from 348 probands of breast-ovarian cancer families was screened for germline mutations in BRCA1 and BRCA2 genes. Overall, deleterious germline mutations were detected in 35/348 familial cases: 23/131 among “high-risk” and 12/217 among “no high-risk” families .1). Families with 3 or more BC cases, including the 112 reported in our previous studies, showed a prevalence rate of 11.7% . Presence of ovarian cancer in family increased the occurrence of BRCA1-2 germline mutations in either the subset of “high-risk” families or the group of “no high-risk” families . No similar variation of mutation rates was observed in families presenting a male member with breast cancer. Stratification of families according to number of breast-ovarian cancer cases showed that BRCA1/2 positivity was significantly higher in families with 3 or more affected members than those with only two cases, with frequencies of 11.7% and 3.5%, respectively. Among 41/131 “high-risk” probands diagnosed at age 40 years, 12 presented a BRCA1-2 germline mutation.
The overall mutation prevalence was 7% in North Sardinia and 17% and 18% in families from Middle and South Sardinia, respectively. BRCA positivity accounts for 11% , 38% and 19% in “high risk” families from these geographical areas .
Having Certain Benign Breast Conditions
Women diagnosed with certain types of benign breast conditions may have a higher risk of breast cancer. Some of these conditions are more closely linked to breast cancer risk than others. Doctors often divide benign breast conditions into different groups, depending on how they affect this risk.
Non-proliferative lesions: These conditions dont seem to affect breast cancer risk, or if they do, the increase in risk is very small. They include:
- Fibrosis and/or simple cysts
- Mild hyperplasia
- Epithelial-related calcifications
Mastitis is not a tumor and does not increase the risk of breast cancer.
Proliferative lesions without atypia : In these conditions theres excessive growth of cells in the ducts or lobules of the breast, but the cells don’t look very abnormal. These conditions seem to raise a womans risk of breast cancer slightly. They include:
- Usual ductal hyperplasia
- Several papillomas
Proliferative lesions with atypia: In these conditions, the cells in the ducts or lobules of the breast tissue grow excessively, and some of them no longer look normal. These types of lesions include:
Breast cancer risk is about 4 to 5 times higher than normal in women with these changes. If a woman also has a family history of breast cancer and either hyperplasia or atypical hyperplasia, she has an even higher risk of breast cancer.
Lobular carcinoma in situ
For more on these conditions, see Non-cancerous Breast Conditions.
You May Like: Breast Cancer In Lymph Nodes Prognosis
How Many Genes Contribute To Breast Cancer
In fact, its thought that mutations in over 100 genes contribute to risk, and the number of non-BRCA gene mutations that raise breast cancer risk is expected to grow as our knowledge of the genetics of cancer increases. 1 . In addition to BRCA1 and BRCA2 gene mutations, some of these include mutations in ATM, PALB2, PTEN, CDH1, CHEK2, TP53,
What Other Cancers Are Linked To Harmful Variants In Brca1 And Brca2
Harmful variants in BRCA1 and BRCA2 increase the risk of several additional cancers. In women, these include fallopian tube cancer and primary peritoneal cancer , both of which start in the same cells as the most common type of ovarian cancer. Men with BRCA2 variants, and to a lesser extent BRCA1 variants, are also at increased risk of breast cancer and prostate cancer . Both men and women with harmful BRCA1 or BRCA2 variants are at increased risk of pancreatic cancer, although the risk increase is low .
In addition, certain variants in BRCA1 and BRCA2 can cause subtypes of Fanconi anemia, a rare syndrome that is associated with childhood solid tumors and development of acute myeloid leukemia . The mutations that cause these Fanconi anemia subtypes have a milder effect on protein function than the mutations that cause breast and ovarian cancer. Children who inherit one of these variants from each parent will develop Fanconi anemia.
Also Check: Breast Cancer Tumor Markers Prognosis
How Many Mutations Are There In Breast Cancer
Our knowledge about gene mutations that raise breast cancer risk is still incomplete, but we now know that there are at least 72 gene mutations linked to hereditary breast cancer. These mutations are thought to be responsible for the 70 percent to 90 percent of hereditary breast cancers that test negative for BRCA gene mutations. 3 The acronym BRCAX has been coined to describe these other mutations, standing for non-BRCA1 BRCA2- related familial breast cancer.
What Is A Gene
Each persons DNA contains the code used to build the human body and keep it functioning. Genes are the small sections of DNA that code for individual traits. For example, someone with naturally red hair has a gene that causes his or her hair to be red.
All inherited traits are passed down through genes. Each person has two copies of every gene: one gene from each parent. Since each parent passes down exactly half of their genes to each child, any of the parents genetic traits has a 50% chance of being passed on to their offspring.
Also Check: Is Grade 3 Breast Cancer Serious
Mutations And Cancer Risk
Certain variations of the BRCA1 gene lead to an increased risk for breast cancer as part of a hereditary breastovarian cancer syndrome. Researchers have identified hundreds of mutations in the BRCA1 gene, many of which are associated with an increased risk of cancer. Females with an abnormal BRCA1 or BRCA2 gene have up to an 80% risk of developing breast cancer by age 90 increased risk of developing ovarian cancer is about 55% for females with BRCA1 mutations and about 25% for females with BRCA2 mutations.
These mutations can be changes in one or a small number of DNA base pairs , and can be identified with PCR and DNA sequencing.
In some cases, large segments of DNA are rearranged. Those large segments, also called large rearrangements, can be a deletion or a duplication of one or several exons in the gene. Classical methods for mutation detection are unable to reveal these types of mutation. Other methods have been proposed: traditional quantitative PCR,multiplex ligation-dependent probe amplification , and Quantitative Multiplex PCR of Short Fluorescent Fragments . Newer methods have also been recently proposed: heteroduplex analysis by multi-capillary electrophoresis or also dedicated oligonucleotides array based on comparative genomic hybridization .
Some results suggest that hypermethylation of the BRCA1 promoter, which has been reported in some cancers, could be considered as an inactivating mechanism for BRCA1 expression.
Brca1/2 Mutations In Pancreatic Cancer
Pancreatic cancer is a disease with poor prognosis and low survival rates worldwide. Its mortality compares strikingly with its incidence. In the UK in 2011, there were 8,773 diagnosed cases and a mortality rate of 8,320 . Through analysis of the literature it was found that both BRCA1 and BRCA2 mutations are associated with the incidence of pancreatic cancer and that BRCA2 mutation poses an increased risk for developing pancreatic cancer . Furthermore environmental and genetic factors have been proposed as causes of the pancreatic cancer with the genetic factor of particular importance believed to be the BRCA2 gene .
It is clear that BRCA1/2 mutations are evident in many familial breast-pancreas cancer families and that carriers of the BRCA2 mutation have an increased risk of developing pancreatic cancer . Nonetheless, the degree to which family history of pancreatic cancer influences the likelihood of detecting a BRCA1/2 mutation in an individual with breast cancer is less clear . Perhaps, differences in population samples can account for conflicting results within studies making it difficult to make a connection. Furthermore, the use of different analysis models within studies can lead to variations in mutation prevalence.
You May Like: Puckering Of The Skin Breast Cancer
How Much Does Genetic Variation Increase Breast Cancer Risk
Individually, each of the newly identified genetic variants increases the risk of breast cancer only slightly by about 5% to 10%. Still, because the genetic variants are common and their effects on risk are multiplied when a woman has more than one of the variants, the combined effect may be dramatic. The effects of the variants also can be increased by other lifestyle factors that increase breast cancer risk, such as being overweight and smoking cigarettes.
Perspectives For The Treatment Of Patients With Brca Mutations
Recent studies propose that 55-65% of BRCA1 mutation carriers, and about 45% of BRCA2 mutation carriers will develop breast cancer by the age of 70 years . Prophylactic surgery in BRCA carriers i.e. salpingo-oophorectomy and mastectomy are proven to be beneficial for reduction the risk of breast and ovarian cancer development , . The carriers of BRCA1 mutations are more likely to develop triple negative breast cancer . TNBC refers to breast cancers which are negative for the expression of hormone epidermal growth factor receptor 2 , estrogen receptors , and progesterone receptors . Since growth of these types of tumors does not depend on the signaling from these receptors, conventional treatments like hormone therapy and drugs that target estrogen, progesterone, and HER-2 are not effective in TNBC patients . At the same time TNBC tumors are highly heterogeneous that is associated with their high resistance to chemotherapy . The deficiency of BRCA1 and BRCA2 proteins in tumor cells is associated with a higher sensitivity to DNA- damaging agents , , . As a result, BRCA1/2-deficient TNBC cancers are more sensitive to standard chemotherapy and have a higher level of immune cell activation compared to TNBC with functional BRCA1/2 proteins .
Don’t Miss: What Percentage Of Breast Biopsies Turn To Cancer
Functional Diversity Of Brca1
In cytoplasm, BRCA1 regulates mitotic cell division, cytoskeletal rearrangement, apoptosis, and mitochondrial genome repair . The E3 ubiquitin ligase activity of BRCA1/BARD1 has a regulatory role in centrosome duplication and assembly of the mitotic spindle pole . In addition, BRCA1 has been implicated in the mitotic spindle checkpoint and recently Bordie et. al. showed that mutation of the NES, or treatment of cells with leptomycin B, a CRM1 export inhibitor, caused a reduction in BRCA1 transport to the centrosome as well as its overall rate of exchange and retention . BRCA1 has also been reported to ubiquitinate another centrosomal protein, nucleophosmin which is important for centrosome duplication . In addition, Bcl-2 and AKT1 have been reported to redirect BRCA1 to mitochondria and endoplasmic reticulum . Thus, the translocation of BRCA1 between cellular compartments is common and highly related to its function in both normal and cancer cells.